Abstract
Background
Pre-hospital ultrasound is a new challenge and lung ultrasound could be an interesting opportunity in the pre-hospital medical service. The aim of our study was to evaluate the efficacy of lung ultrasound in out-of-hospital non-traumatic respiratory insufficiency.
Methods
We planned a case-controlled study in the ULSS 5 ovest vicentino area (Vicenza—Italy) enrolling subjects with severe dyspnea caused by cardiac heart failure or acute exacerbation of chronic obstructive pulmonary disease. We compared drugs administration, oxygen delivery, and laboratory tests between those patients with ultrasound integrated management and those without ultrasound.
Results
Pre-hospital lung ultrasound had a high specificity (94.4%) and sensitivity (100%) for the correct identification of alveolar interstitial syndrome using B lines, whereas the percentages obtained with pleural effusion were lower (83.3, 53.3%, respectively). The patients with ultrasound integrated management received a more appropriate pharmacological therapy (p 0.01), as well as non-invasive ventilation (CPAP) was used more frequently in those with an acute exacerbation of chronic obstructive pulmonary disease (p 0.011). Laboratory tests and blood gases analysis were not significant different between the two study groups. In a sub-analysis of the patients with an A profile, we observed a significant lower concentration of PCO2 in those with an ultrasound integrated management (PCO2: 42.62 vs 52.23 p 0.049). According with physicians’ opinion, pre-hospital lung ultrasound gave important information or changed the therapy in the 42.3% of cases, whereas it just confirmed physical examination in the 67.7% of cases.
Conclusions
Pre-hospital lung ultrasound is easy and feasible, and learning curve is rapid. Our study suggests that cardiac heart failure and acute exacerbation of chronic obstructive pulmonary disease can be considered two indications for pre-hospital ultrasound, and can improve the management of patient with acute respiratory insufficiency.
Similar content being viewed by others
Background
Pre-hospital ultrasound is considered one of the top five research priorities according to the opinion of a consensus meeting of a European expert panel, to identify which ultrasound examinations can be reliably transferred to the pre-hospital setting, how they affect patient management and pathway, and how providers can achieve and maintain specific ultrasound skills [1].
The indications are few and well defined, physicians and operators must be adequately trained, and the examinations must be short, focused, and strictly connected with the patients’ symptoms and history. The technical skills are the same of in-hospital critical ultrasound or even simpler [2,3,4,5,6,7,8].
The FAST protocol has been used successfully for the management of trauma, both inside and outside the hospital [9, 10].
Ultrasound was included in the latest guidelines for cardiopulmonary resuscitation as a supplementary tool for the identification of reversible causes of cardiac arrest [11].
In the same document, ultrasound was recognized as an additional device for airway management and for post-procedural check of the correct placement of an endo-tracheal tube [11, 12].
The lung ultrasound has changed significantly in-hospital management of non-traumatic respiratory insufficiency, and it could be a new and interesting opportunity also in the pre-hospital setting with a few and clear indications: the determination of the lung profile (A: no signs of increased extravascular lung water—“dry lung”; B: increased extravascular lung water—“wet lung”), the identification of pleural effusions, and the diagnosis of pneumothorax [2, 13].
Lung evaluation is rapid and physicians can reach a reliable diagnosis in a few minutes [13,14,15].
A rapid two-point technique (upper anterior and basal lateral areas) is usually enough to rule in or rule out an interstitial syndrome, a pneumothorax, or a pleural effusion [13, 15,16,17].
Nevertheless, there are not many studies evaluating the real effectiveness of the pre-hospital lung ultrasound: Neesse et al. [15] showed that the identification of a pleural effusion is useful for the differentiation between a cardiac heart failure (CHF) and an acute exacerbation of a chronic obstructive pulmonary disease (COPD). Strnad et al. and Ferrari and collaborators suggested that lung ultrasound is reliable to monitor response to pre-hospital treatment with continuous positive airway pressure (CPAP) in patients with CHF [18, 19].
The primary and secondary outcomes of our work evaluated the efficacy of lung ultrasound in out-of-hospital non-traumatic respiratory insufficiency, by analyzing clinical and laboratory parameters after the arrival at the emergency department. In particular, we compared drug administration, ventilation, oxygen delivery, and laboratory tests between those patients with ultrasound integrated management and those without ultrasound.
Methods
We planned a case-controlled study in the pre-hospital emergency setting of the ULSS 5 ovest vicentino area (Vicenza—Italy) between January 2016 and December 2016.
This area included one major emergency department with 35.000 accesses par year, and a minor emergency department located in the countryside with 6000 accesses par year, each one with an emergency physician-led advanced life support (ALS) ambulance.
The former had an ultrasound portable device (Nanomax Sonosite) in the ambulance; the latter did not. All controlled cases were collected from the second one.
All patients included in the studied were treated in the major emergency department.
Inclusion criteria was severe dyspnea as prevalent symptom most likely caused by CHF or COPD exacerbation and digital pulse oximetry ≤ 90%, whereas exclusion criteria were other causes of respiratory insufficiency (for example: trauma, pulmonary embolism, cancer) and subjects less that 18 years old.
The two groups were matched for age, gender, type of respiratory insufficiency, and digital pulse oximetry recorded by the ambulance crew.
All recruited patients underwent a rapid and complete physical examination. Blood pressure, heart frequency, and pulse oximetry were tested.
Oxygen was delivered using an oxymask and inspiratory fraction of oxygen was extrapolated by oxygen flow according with the operating instructions.
Non-invasive ventilation was performed using a Boussignac system that allowed the application of a continuous positive airway pressure (PEEP) from 5 to 10 cmH2O and the possibility to choose among three different percentages of oxygen: 30, 50, and 100%. The criteria used for using the CPAP were the presence of at least one of the following findings: a persistent oximetry lower than 90% even after oxygen supplementation with the oxymask, respiratory rate higher than 30 per min, mild drowsiness.
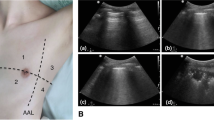
Lung ultrasound was performed after the clinical examination with a rapid two-point technique (upper anterior and basal lateral areas). The type of lung profile (A profile: dry lung; B profile: wet lung) and the presence of a pleural effusion were recorded.
An interstitial syndrome was defined by the presence of three or more B lines in a longitudinal plane between two ribs in two or more regions bilaterally with a symmetrical pattern, with or without a pleural effusion.
All ultrasound examinations were performed with the same ultrasound device (Sonosite Nanomax) using a convex probe (3.5–5 MHz). A linear probe was used to improve the accuracy in case of an undefined diagnosis.
Operators were certified emergency physicians who had accomplished a full mentoring program for “UltraSound Life Support”.
In-hospital assessment included a physical examination, laboratory tests, blood gases analysis, a chest X-ray, in-hospital lung ultrasound, a focused echocardiography, and a static and dynamic evaluation of the vena cava.
The diagnosis made after discharge from the emergency department or after hospitalization was compared with the one made by the physician in the ambulance.
In-hospital lung ultrasound was blinded with respect to pre-hospital one and performed soon after the arrival at the hospital by the emergency physician of the emergency department.
The study evaluated the feasibility of pre-hospital lung ultrasound and the improvement of both pharmacological and oxygen administration in the ambulance and of the blood gases analysis (pH and CO2) at the arrival at the emergency department.
Finally, we compared hospitalization rate and the time spent in the emergency department between the two study groups.
The study was conducted in accordance with Helsinki Declaration, it had been previously approved by local medical ethics committee and a written informed consent was collected from all the patients.
Statistical analysis
We expressed as mean and standard deviation all the anthropometric and laboratory parameters of the patients.
Standard T test was used for the comparison of parametric variables, whereas Chi-square analysis was chosen for non-parametric data.
Sensitivity, specificity, and positive (PPV) and negative (NPV) predictive values were calculated to test the diagnostic capability of the pre-hospital lung ultrasound.
Finally physician’s opinions about the utility of the pre-hospital ultrasound were transformed into percentages.
Results were considered statistically significant for p value lower than 0.05.
Statistical analysis was made using SPSS 16.0.
Results
We recruited 30 patients affected by non-traumatic respiratory insufficiency caused by CHF (12 patients) or acute exacerbation of COPD (18 patients), who underwent an ultrasound integrated management (US group) and were compared with 30 patients managed without ultrasound (NUS group).
The characteristics of the two groups are described in Table 1. The two groups were comparable for age, gender, type of respiratory insufficiency, and pulse oximetry values at the arrival of the ALS ambulance.
Pre-hospital lung ultrasound was accurate for the identification of the correct lung profile, in particular for the diagnosis of an interstitial syndrome.
B lines had both a high sensitivity (100%) and specificity (94.4%), and a high PPV and NPV (92.3 and 100%, respectively) for the diagnosis of cardiac heart failure.
The presence of a pleural effusion was not as accurate as B lines for CHF: sensitivity 83.3%, specificity 58.3%, PPV 75.0%, and NPV 70.0%.
Finally, the same percentages obtained by the combination of B lines with pleural effusion for the diagnosis of CHD were 77.8, 100, 100, and 75.5%, respectively.
The number of patients who received an appropriate pharmacological treatment was significantly higher in US group (p < 0.001), especially in those subjects with an A profile (non-cardiogenic respiratory insufficiency—COPD; p < 0.0001). In this subgroup, the mean dose of furosemide was significantly lower in the US group than the NUS group (3.33 mg vs 15.29 mg p = 0.036). On the contrary, in the subgroup of patients with a B profile (CHF), the mean dosage of furosemide was higher in the US groups (42.50 mg vs 29.41 mg), even though not significantly (Fig. 1).
The corticosteroid administration (methylprednisolone) was comparable both between the two groups with an A profile (34.72 vs 29.00 mg) and with a B profile (9.62 vs 11.36 mg) (Fig. 1).
We did not find any difference in the pre-hospital administration of other medications such us morphine, salbutamol, nitroglycerin, and vasoactive agents.
Comparing the use of CPAP, in those patients with an A profile, it was employed more in the US group than in the NUS one (p 0.011), whereas the use was comparable in the two groups with a B profile. Moreover, the FIO2 administered was not significantly different between groups.
Blood gases analysis was not significantly different in the US group than in the NUS group.
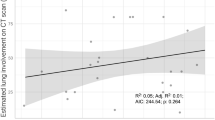
Anyway, a sub-analysis of patients with the A profile showed that PCO2 was significantly lower in the US group than NUS group (PCO2: 42.62 vs 52.23 p 0.049) (Fig. 2).
We did not found any significant difference in all the other laboratory examinations (Table 1).
Two patients were intubated in the NUS group and one in the US group, without any statistical significance.
The convex probe was always the probe of choice and the linear probe was never used.
Hospitalization rate was comparable between the two study groups, whereas we observed a reduction of the overall time spent in the emergency department by the US group (267.77 ± 406.15 vs 463.24 ± 521.29 min), but these data did not reach a full statistical significance.
According with physicians’ opinion, pre-hospital lung ultrasound either gave important information or changed the therapy in the 42.3% of cases, whereas it just confirmed physical examination and therapy in the remaining 67.7% of cases.
Discussion
Lung ultrasound is undoubtedly an effective and reliable instrument capable to improve medical care [13].
It has changed in-hospital management of respiratory insufficiency, it has demonstrated remarkable results in patients with trauma of the chest, and both the FAST and the Extended-FAST (EFAST) are two effective protocols that are used worldwide [9, 10, 20,21,22,23].
Anyway it is not clear if the same efficacy can be exploited in the pre-hospital medical service for non-traumatic respiratory insufficiency [15,16,17,18].
The critical points are three: which are the most remarkable indications? Does it influence the management of respiratory insufficiency? Does it change short- and long-term prognosis?
In our article, we focused our attention on patients affected by cardiac heart failure and acute exacerbation of chronic obstructive pulmonary disease.
We chose CHF and COPD, because their ultrasound patterns are completely different and ultrasound has a high sensitivity and specificity for the identification of the type of lung profile: the former has a B profile (wet lung) and the latter an A profile (dry lung) (Fig. 3) [13, 24].
Our data confirm that pre-hospital ultrasound can differentiate them with a high sensitivity and sensibility.
The examination time was very rapid, all the scans lasted less than 3 min, the two points technique was adequate to examine the chest and the convex probe was always appropriate [2, 13].
The linear probe would have been used if lung profile had not been clear enough, but it never happened.
We tested B lines, the pleural effusion, and the combination between them as ultrasonographic signs for the diagnosis of CHD.
Neesse et al. [15] showed that the identification of a pleural effusion is useful for the diagnosis of CHD in the pre-hospital setting. Nevertheless, our data indicate that B lines had a higher sensitivity and specificity and the combination of the two findings did not improve the diagnostic capability.
Since the identification of B lines is simpler and faster than the diagnosis of pleural effusion, we think that the presence of a bilateral, diffuse, and symmetrical B profile of the lungs is enough for the diagnosis of CHD in a pre-hospital setting.
We did not have any recordings about the time required for the sole identification of the lung profile, but it would have been certainly shorter than the 3 min described above, probably within 1 min.
The second question regards the possibility to influence medical decision-making?
A more accurate diagnosis brought about a more adequate therapy.
In the US group, the patients with CHF received a higher dosage of furosemide, even though not significantly, whereas it was significantly lower in case of COPD. The data are certainly more remarkable in those with an acute exacerbation of COPD, because it reduced inappropriate drug administration preventing hypotension, dehydration, and electrolyte imbalance.
Non-invasive ventilation (CPAP) was used thoroughly in patients affected by CHD, whereas, in those with COPD exacerbation, it was applied more often in the US group than in the NUS group. We think that the possibility to identify the correct lung profile made the physicians more confident in choosing the most appropriate type of ventilation and setting for the CPAP.
Eventually in-hospital blood gas analysis showed a lower level of PCO2 in patients affected by COPD when ultrasound was used. The better diagnostic performances given by ultrasound helped the physicians to titrate the oxygen better, reducing the risk of hypercapnia and acidosis.
One of the most remarkable consideration that comes out from these results is that ultrasound made more homogeneous the pre-hospital approach, independently from the medical specialization of the physicians. Indeed, since the physicians who worked in the ambulance with the ultrasound and in the one without were the same, we might assess that the improvement of diagnostic accuracy and medical assistance was determined by the ultrasound integrated approach.
This was possible, because the identification of the lung patter is simple and extremely different between a pulmonary oedema and an acute exacerbation of COPD (Fig. 3). The possibility to “watch the diagnosis on the screen” permitted to choose easily the most appropriate therapy, despite all the confounding elements that are usually caused by the noise and the narrow spaces inside the ambulance or by the patient conditions.
Moreover, the learning curve for the identification of the lung profile is easy and rapid [25]. Consequently, it lets also paramedics, who work in the pre-hospital medical service, to approach lung ultrasound, as it has already been done with FAST, so that the choice of ventilation, oxygen administration, and CPAP setting would become easier and safer for everyone.
Finally, we are not able to answer the third question: we did not collect enough information about the prognosis and the outcome of patients. Anyway, we found a reduction of the time spent in the ED by the patients with the ultrasound integrated approach. We think that the result is interesting even if it was not completely significant and, according to the extent of the reduction, the lack of significance might be caused by the small number of subjects. The possibility to reach the correct diagnosis and to set the right therapy earlier permitted to speed up the in-hospital management of the patients.
Limitations
The study has certainly several limitations.
First of all, the number of patients is low and should be increased, including other causes of respiratory insufficiency.
Then, it is a case–control study, whereas a randomized-controlled trial could have been more adequate from a statistical point of view.
Most of pre-hospital scans were not re-evaluated by a blinded second operator, because they had not been stored or recorded properly.
The two study groups were matched by comparing digital oxygen values recorded by the ambulance crew, without considering the duration of symptoms and previous history of COPD.
Conclusions
Pre-hospital lung ultrasound is easy and feasible, and learning curve is very rapid [25].
Pulmonary oedema and COPD should be considered as proven indications for pre-hospital ultrasound, since it can improve both pharmacological therapy and oxygen delivery.
Our study population was small, so that other studies should be planned to support our findings, and to establish the influence of ultrasound on invasive management of airways and on short- and long-term prognosis.
Abbreviations
- ALS:
-
advanced life support
- COPD:
-
chronic obstructive pulmonary disease
- CHF:
-
cardiac heart failure
- CPAP:
-
continuous positive airway pressure
- Cr:
-
serum creatinine
- CPR:
-
C reactive protein
- DBP:
-
diastolic blood pressure
- FAST:
-
fast assessment sonography for trauma
- EFAST:
-
extended fast assessment sonography for trauma
- FIO2 :
-
fraction of inspired oxygen
- Hb:
-
haemoglobin concentration
- HR:
-
heart rate
- LUS:
-
lung ultrasound
- NUS group:
-
group without an ultrasound integrated management
- PCO2 :
-
partial pressure of carbon dioxide
- PEEP:
-
continuous positive airway pressure
- PPV:
-
positive predictive value
- NPV:
-
negative predictive value
- O2%:
-
pulse oximetry
- SBP:
-
systolic blood pressure
- US group:
-
ultrasound integrated management group
- WBC:
-
white blood cells
References
Fevang E, Lockey D, Thompson J, Lossius HM, Torpo Research Collaboration (2011) Top five research priorities in physician-provided pre-hospital critical care: a consensus report from a European research collaboration. Scand J Trauma Resusc Emerg Med 13:19–57
Zanatta M, Benato P, Cianci V (2016) Pre-hospital ultrasound: current indications and future perspectives. Int J Crit Care Emerg Med 2:019. https://doi.org/10.23937/2474-3674/1510019
Bush M (2006) Portable ultrasound in pre-hospital emergencies: a feasibility study. Acta Anaesthesiol Scand 50:754–758
Taylor J, McLaughlin K, McRea A, Lang E, Anton A (2014) Use of prehospital ultrasound in North America: a survey of emergency medical services medical directors. BMC Emerg Med 1:14–16
Knudsen L, Sandberg M (2011) Ultrasound in pre-hospital care. Acta Anaesthesiol Scand 55:377–378
El Sayed MJ, Zaghrini E (2013) Prehospital emergency ultrasound: a review of current clinical applications, challenges, and future implications. Emerg Med Int 2013:531674. https://doi.org/10.11155/2013/531674
Lapostolle F, Petrovic T, Lenoir G, Catineau J, Galinski M, Metzger J, Chanzy E, Adnet F (2006) Usefulness of hand-held ultrasound devices in out-of-hospital diagnosis performed by emergency physicians. Am J Emerg Med 24:237–242
O’Dochartaigh D, Douma M, MacKenzie M (2017) Five-year retrospective review of physician and non-physician performed ultrasound in a Canadian critical care helicopter emergency medical service. Prehosp Emerg Care 21:24–31
Rozycki GS, Ochsner MG, Schmidt JA, Frankel HL, Davis TP, Wang D, Champion HR (1995) A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma 39:492–500
Scalea TM, Rodriguez A, Chiu WC, Brenneman FD, Fallon WF Jr, Kato K, McKenney MG, Nerlich ML, Ochsner MG, Yoshii H (1999) Focused assessment with sonography for trauma (FAST): results from an international consensus conference. J Trauma 46:466–472
Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, Brooks SC, de Caen AR, Donnino MW, Ferrer JM, Kleinman ME, Kronick SL, Lavonas EJ, Link MS, Mancini ME, Morrison LJ, O’Connor RE, Samson RA, Schexnayder SM, Singletary EM, Sinz EH, Travers AH, Wyckoff MH, Hazinski MF (2015) Part 1: executive summary: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132(18 Suppl 2):S315–S367. https://doi.org/10.1161/CIR.0000000000000252
Brun PM, Besserau J, Cazes N, Querrelou E, Chenaitia H (2012) Lung ultrasound associated to capnography to verify correct endotracheal tube positioning in prehospital. Am J Emerg Med 30(2080):e5–e6
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T, International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS) (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38:577–591
Hoyer HX, Vogl S, Schiemann U, Haug A, Stolpe E, Michalski T (2010) Prehospital ultrasound in emergency medicine: incidence, feasibility, indications and diagnoses. Eur J Emerg Med 17:254–259
Neesse A, Jerrentrup A, Hoffman S, Sattler A, Gorg C, Kill C, Gress TM, Kunsch S (2012) Prehospital chest emergency sonography trial in Germany: a prospective study. Eur J Emerg Med 19:161–166
Zechner PM, Aichinger G, Riguad M, Wildner G, Prause G (2010) Prehospital lung ultrasound in the distinction between pulmonary edema and exacerbation of chronic obstructive pulmonary disease. Am J Emerg Med 28:389.e1-2
Stefanone G, Boero E, Sverzellati N, Cardinale L, Bussi M, Boccuzzi F, Tullio M, Lamorte A, Stefanone V, Ferrari G, Veltri A, Francisco MF (2014) Semi-quiantification of pneumothorax volume by lung ultrasound. Intensive Care Med 40:1460–1467
Strnad M, Prosen G, Borovnik Leskjak V (2016) Bedside lung ultrasound for monitoring effectiveness of prehospital ultrasound treatment with continuous positive airway pressure in acute decompensated heart failure. Eur J Emerg Med 23:50–55
Ferrari G, Esquinas AM (2015) Lung ultrasound in prehospital acute cardiac pulmonary edema: a new practical toll for CPAP assessment. Eur J Emerg Med 22:146–147
Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, Hameed SM, Brown R, Simons R, Dulchavsky SA, Hamiilton DR, Nicolaou S (2004) Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST). J Trauma 57:288–295
Jorgensen H, Jensen CH, Dirks J (2010) Does pre-hospital ultrasound improve treatment of the trauma patient? A systematic reviews. Eur J Emerg Med 17:249–253
Rudolph SS, Sorensen MK, Svane C, Hessefeldt R, Steinmez J (2014) Effect of pre-hospital ultrasound on clinical outcomes of non-trauma patients—a systematic review. Resuscitation 85:21–30
O’Dochartaigh D, Douma M (2015) Pre-hospital ultrasound of the abdomen and thorax changes trauma patients management: a systematic review. Injury 11:2093–2102
Copetti R, Soldati G, Copetti P (2008) Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 29:6–16
Picano E, Frassi F, Agricola E, Gligorova S, Gargani L, Mottola G (2006) Ultrasound lung comets: a clinically useful sign of extravascular lung water. J Am Soc Echocardiogr 19:356–363
Authors’ contributions
MZ: study conception and design, acquisition of data, analysis and interpretation of data, drafting the manuscript, and critical revision. PB: study conception and design, acquisition of data, and critical revision. SDB: acquisition of data and critical revision. CP: acquisition of data and critical revision. RI: acquisition of data and critical revision. VC: study conception and design, drafting the manuscript, and critical revision. All authors read and approved the final manuscript.
Acknowledgements
We thank Cristina Dalla Pellegrina, a nurse of our emergency department, for her precious job in filing all the documents.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by local medical ethics committee and an informed consent was collected from all the patients.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zanatta, M., Benato, P., De Battisti, S. et al. Pre-hospital lung ultrasound for cardiac heart failure and COPD: is it worthwhile?. Crit Ultrasound J 10, 22 (2018). https://doi.org/10.1186/s13089-018-0104-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13089-018-0104-5