Abstract
Background
Point-of-care (POCUS) education is rapidly expanding within medical schools and internal medicine residency programs, but lack of trained faculty is a major barrier. While POCUS training can improve short-term outcomes, knowledge and skills rapidly decay without deliberate practice and feedback. The purpose of this study was to evaluate the performance of focused cardiac ultrasound (FCU) by volunteer general internal medicine (GIM) faculty participating in a longitudinal POCUS curriculum.
Methods
Participants: Nine GIM clinician-educators participated in a 6-month POCUS curriculum. Faculty performance was compared to three cardiology fellows. Three diagnostic cardiac sonographers (DCS) were also evaluated and served as the gold standard. Evaluation: the primary outcome was a FCU efficiency score, calculated by dividing image quality score by exam duration. FCU exams were conducted on three standardized patients after completion of an introductory workshop, at 3 months, and at 6 months. Two blinded cardiologists scored the exams. Analysis: mean efficiency scores were compared using a linear mixed effects model, followed by pairwise comparisons using Tukey’s test.
Results
GIM faculty’s FCU efficiency scores were maintained over the 6-month period (2.2, SE 1.0 vs. 3.8, SE 1.0, p = 0.076). Their scores at each session were similar to cardiology fellows (p > 0.69), but inferior to DCSs (p < 0.0001).
Conclusion
GIM faculty participating in a POCUS curriculum maintained their FCU performance over 6 months with efficiency scores comparable to experienced cardiology fellows.
Similar content being viewed by others
Background
Point-of-care ultrasound (POCUS) is clinician-performed ultrasonography used to guide real-time diagnostic and management decisions. POCUS training is rapidly expanding in undergraduate and graduate medical education. Twenty-eight percent of medical schools offer POCUS curricula [1], including several well-established, vertically-integrated programs [2,3,4]. A survey of Association of Program Directors in Internal Medicine members found that 25% of respondents reported formal POCUS curricula, with another 25% planning to implement programs within a year [5]. Educational leaders in these studies identified faculty development as a major barrier to broader adoption of POCUS training [1, 5].
Despite the increasing need for POCUS-trained faculty in medical education, limited research has investigated training programs for general internal medicine (GIM) faculty. One 10-week faculty program resulted in improved self-reported confidence and exam scores, but image acquisition skills were not assessed [6].
POCUS training can improve short-term outcomes, but knowledge and skills decay without ongoing support. A study of internal medicine physicians who completed a 3-year POCUS curriculum during residency demonstrated poor retention of cardiac ultrasound skills after more than 1 year of nonuse [7]. Surgical residents and medical students who participated in a 2-h cardiac ultrasound course had significant decay in their knowledge and skills within 1 month [8]. Studies of internal medicine residents found knowledge deteriorated in the months following workshop-based training [9], but that longitudinal support prevented knowledge decay [10].
This study investigated the impact of a longitudinal POCUS curriculum on GIM faculty’s performance of focused cardiac ultrasound (FCU). We hypothesized that at the end of the study period, GIM faculty performance of FCU would be resilient to skills decay and comparable to cardiology fellows’ performance.
Methods
Participants and setting
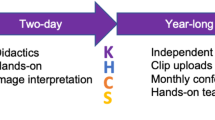
Nine volunteer GIM clinician-educators at an academic health center participated in a 6-month POCUS curriculum with a goal of developing core faculty for a residency program. Faculty did not receive protected time from other duties. Figure 1 illustrates the structure and content of the faculty development curriculum, including elements that were eligible for continuing medical education (CME) credit. The introductory workshop was required, but all other curricular elements were voluntary. Subsequent lectures and workshops were scheduled to accommodate as many participants as possible. Before these sessions, participants were asked to review relevant online modules from free open-access medical education resources. Modules were typically 10–15 min in duration. In-person didactics were recorded and posted to an online learning management system for asynchronous review. Peer-group practice was arranged by group members.
GIM faculty performance was compared to three senior cardiology fellows who had completed level 1 echocardiography training [11], including performance of 75 comprehensive echocardiographic studies. Three registered diagnostic cardiac sonographers (DCS) served as the gold standard.
Evaluation
We scored FCU exams using a validated image acquisition assessment tool [12]. As in the validation study, our primary outcome was an FCU efficiency score, calculated by dividing an image quality score by exam duration in minutes. The original 68-point image quality score was modified to 66-points, as two scoring items were not taught (inferior vena cava M-mode and respiratory variation measurement). The scoring instrument was comprised of two sections. The first section included scoring of anatomic structures and image optimization (appropriate depth, gain, and centering) in the following views: parasternal long axis; parasternal short-axis aortic valve, mitral valve, mid-papillary, and apex; apical four chamber; subcostal long axis; and subcostal inferior vena cava (IVC). The second section scored the overall diagnostic image quality of the exam for common clinical questions, such as left ventricular systolic function. Assessments took place after completion of an 8-h introductory workshop (baseline), at 3 months, and at 6 months. FCU exams were performed on the same three standardized patients (SPs) at each session. The research team chose SPs that represented a cross-section of typical IM patients (two women, age 48–79 years, body mass index 23–39 kg/m2). One SP had a hiatal hernia, which was not known prior to the research sessions. Using cart-sized point-of-care ultrasound machines (Sparq; Philips Healthcare, Andover, MA), participants captured video loops in the required views, outlined above. Before each session, written instructions were provided to participants, facilitators, and SPs (Additional file 1: Appendix S1). The machines used for the assessment were the same as those available to GIM faculty during their curriculum. Before each assessment session, the cardiology fellows and DCS received an in-person tutorial on machine set-up and knobology. Two board-certified cardiologists scored the FCU exams. They were blinded to participant group, SP, and exam session. Prior to scoring research images, they scored three pilot exams together to ensure similar application of the scoring instrument. They then independently scored two pilot exams, resulting in nearly identical scores (53 vs. 52 and 41.5 vs. 42.5 points).
Analysis
Mean FCU efficiency scores, image quality total score, image quality sub-group scores, and exam duration were compared using a linear mixed effects model with random effects for SP and participant and fixed effects for session and group (GIM faculty, cardiology fellows, and DCSs). If the interaction of group and session were statistically significant, Tukey’s test was performed to make pairwise comparisons of the mean scores between the three groups for each session. If the interaction of group and session was not significant, pairwise comparisons were performed between the groups (combining sessions) and between the sessions (combining groups). Model adjusted means and standard errors (SE) were used for descriptive statistics. Spearman correlation coefficients were used to assess the association of total CME hours with efficiency score. p < 0.05 was considered statistically significant. Statistics were calculated using SAS Version 9.4 software (SAS Inc., Cary, NC). The University of Nebraska Medical Center Institutional Review Board approved the study (163-16-EX).
Results
Four of nine GIM faculty were female (44%) and eight (89%) had no prior POCUS training. Eight participants (89%) completed all three sessions. Faculty earned an average of 30.6 CME hours (SD 8.6 h) over the 6 months. The average attendance at voluntary curricular components (workshops, didactics, and image review sessions) over the 6 months was 68% (range 38–88%). FCU efficiency score data are displayed in Table 1. GIM faculty efficiency scores were maintained over the 6-month study period (baseline 2.2, SE 1.0 vs. 6 months 3.8, SE 1.0, p = 0.076). There was no difference between mean GIM faculty and cardiology fellow efficiency scores during any of the three assessment sessions (Fig. 2). DCSs performed significantly better than GIM faculty and cardiology fellows during all three assessments (p < 0.0001).
GIM faculty image quality scores were sustained between the baseline and 6-month evaluations (36.7, SE 5.2 vs. 39.7, SE 5.3, p = .34). In the linear mixed effect model analysis, there was no significant interaction between group and session for image quality score (p = 0.73), so pairwise comparison was made combining the three sessions. Overall, cardiology fellows had a higher mean image quality score than GIM faculty (50.6, SE 6.0 vs. 40.8, SE 5.0, p = 0.037). Table 2 displays the image quality scores for each exam sub-section. GIM faculty and cardiology fellow sub-group scores were comparable for the parasternal long axis and subcostal long axis views, as well as for overall diagnostic quality. Cardiology fellow scores were significantly higher for the parasternal short axis, apical four chamber, and subcostal IVC.
GIM faculty’s exam duration decreased during the study period (baseline 17.5 min, SE 1.5 vs. 6 months 13.0, SE 1.5 min, p < .001). Combining the three sessions, GIM faculty and cardiology fellow exam duration were comparable across the three sessions (faculty 15.3 min, SE 1.4 vs. fellows 13.8 min, SE 1.8, p = 0.64).
Discussion
GIM faculty participating in a voluntary, multi-modal curriculum maintained their FCU acquisition skills over a 6-month period. GIM faculty efficiency scores were similar to those previously reported by critical care physicians with American Society of Echocardiography level III certification (although the latter performed FCU on mechanically ventilated patients) [12]. Our findings highlight the importance of longitudinal support when teaching FCU to novice faculty. FCU performance requires integration of a complex set of psychomotor skills, which cannot be mastered without regular practice and feedback. Prior studies of novice cardiology fellows [13] and hospitalists [14] found that FCU skills can be developed in weeks to months with frequent expert coaching. The duration of training required to achieve proficiency likely depends on institutional resources and needs. In the present study, GIM faculty did not have dedicated time and was concomitantly learning non-cardiac POCUS applications, requiring a longer curriculum.
Our primary outcome was a measure of efficiency, which Gaudet et al. [12] have argued is a “hallmark of expertise”. Efficiency has been used as an assessment variable in prior FCU performance studies [15] and is important for several reasons. First, POCUS must be economical for integration into clinicians’ daily workflow. Exam efficiency is also vital for the prompt assessment of time-sensitive clinical conditions, such as shock. Finally, task efficiency may precede improvements in performance quality. This phenomenon has been observed in prior FCU studies [12, 13] and performance research for other fine-motor skills, such as endoscopy [16].
While GIM faculty had efficiency scores similar to cardiology fellows, their total image quality scores were lower. This reason for this is likely multifactorial. GIM faculty may not have engaged in enough deliberate practice over the 6 months to advance their image acquisition skills [17]. Additionally, cardiology fellows’ extensive experience in interpreting diagnostic echocardiography studies may have contributed to their superior scores. It should also be noted that our FCU protocol included views which are more technically challenging for novices [15]. Some of these views, such as apical four chambers, are excluded from commonly-used FCU exam protocols [18]. Although their total image quality scores were lower, GIM faculty performed comparably to cardiology fellows for overall diagnostic quality. This may be the most clinically relevant outcome, as the primary purpose of POCUS is to quickly gain information to guide clinical decision making.
This study adds to the existing literature in several ways. It is one of the first papers to examine the educational outcomes of a longitudinal POCUS curriculum for GIM faculty. Studies of residents and fellows may not be applicable to faculty, given differences in clinical experience, time availability, and willingness to adopt innovations [19]. Additionally, we assessed performance of a complete FCU exam protocol including all recommend views [20] and utilized a validated scoring instrument. Finally, the baseline assessment occurred after an intensive introductory workshop, allowing us to evaluate the impact of the longitudinal portion of the curriculum independent of the introductory training.
There are limitations to this study. It was conducted at a single institution with few participants. Repeated scanning of the same SPs may have led to higher scores due to familiarity, although this was likely limited by the 3-month washout periods. Furthermore, only the GIM faculty group showed improvement across all testing periods. We were unable to accurately track the number of exams performed by each participant during the curriculum to look for correlation with performance outcomes. Additionally, our study did not assess image interpretation skills, which typically develop more quickly than image acquisition skills [21].
In conclusion, GIM faculty participating in a longitudinal POCUS curriculum maintained their FCU acquisition skills over a 6-month period. Efficiency scores were comparable to cardiology fellows, but overall image quality was lower. Future studies will need to examine if GIM performance of FCU is sustainable beyond 6 months.
Abbreviations
- POCUS:
-
point-of-care ultrasound
- GIM:
-
general internal medicine
- FCU:
-
focused cardiac ultrasound
- CME:
-
continuing medical education
- DCS:
-
diagnostic cardiac sonographer
- SP:
-
standardized patient
- SE:
-
standard error
- BLUE:
-
bedside lung ultrasound in emergency
- CLUE:
-
cardiopulmonary limited ultrasound examination
- RUSH:
-
rapic ultrasound for shock and hypotension
References
Dinh VA, Fu JY, Lu S et al (2016) Integration of ultrasound in medical education at United States medical schools: a national survey of directors’ experiences. J Ultrasound Med 35(2):413–419. https://doi.org/10.7863/ultra.15.05073
Hoppmann RA, Rao VV, Poston MB et al (2011) An integrated ultrasound curriculum (iUSC) for medical students: 4-year experience. Crit Ultrasound J 3(1):1–12. https://doi.org/10.1007/s13089-011-0052-9
Bahner DP, Adkins EJ, Hughes D et al (2013) Integrated medical school ultrasound: development of an ultrasound vertical curriculum. Crit Ultrasound J 5(1):6. https://doi.org/10.1186/2036-7902-5-6
Wilson SP (2017) Implementation of a 4-year point-of-care ultrasound curriculum in a liaison committee on medical education-accredited US medical school. J Ultrasound Med 36(2):321–325. https://doi.org/10.7863/ultra.16.03068
Schnobrich DJ, Gladding S, Olson AP et al (2013) Point-of-care ultrasound in internal medicine: a national survey of educational leadership. J Grad Med Educ 5(3):498–502. https://doi.org/10.4300/jgme-d-12-00215.1
Maw A, Jalali C, Jannat-Khah D et al (2016) Faculty development in point of care ultrasound for internists. Med Educ Online 21:33287. https://doi.org/10.3402/meo.v21.33287
Kimura BJ (2016) Retention of ultrasound skills and training in “point-of-care” cardiac ultrasound. J Am Soc Echocardiogr 29(10):992–997. https://doi.org/10.1016/j.echo.2016.05.013
Yamamoto RR (2018) Rapid decay of transthoracic echocardiography skills at 1 month: a prospective observational study. J Surg Educ. https://doi.org/10.1016/j.jsurg.2017.07.011
Town JA et al (2016) Internal medicine residents’ retention of knowledge and skills in bedside ultrasound. J Grad Med Educ 8(4):553–557. https://doi.org/10.4300/jgme-d-15-00383.1
Kelm DJ, Ratelle JT, Azeem N et al (2015) Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ 7(3):454–457. https://doi.org/10.4300/jgme-14-00284.1
Ryan T et al (2015) COCATS 4 task force 5: training in echocardiography: endorsed by the American society of echocardiography. J Am Soc Echocardiogr 28(6):615–627. https://doi.org/10.1016/j.echo.2015.04.014
Gaudet J, Waechter J, McLaughlin K et al (2016) Focused critical care echocardiography: development and evaluation of an image acquisition assessment tool. Crit Care Med. https://doi.org/10.1097/ccm.0000000000001620
Prinz C, Dohrmann J, van Buuren F et al (2012) The importance of training in echocardiography: a validation study using pocket echocardiography. J Cardiovasc Med (Hagerstown, Md) 13(11):700–707. https://doi.org/10.2459/jcm.0b013e328356a55f
Lucas BP et al (2009) Diagnostic accuracy of hospitalist-performed hand-carried ultrasound echocardiography after a brief training program. J Hosp Med 4(6):340–349. https://doi.org/10.1002/jhm.438
Chisholm CB et al (2013) Focused cardiac ultrasound training: how much is enough? J Emerg Med 44(4):818–822. https://doi.org/10.1016/j.jemermed.2012.07.092
Verdaasdonk EGG et al (2007) Construct validity and assessment of the learning curve for the SIMENDO endoscopic simulator. Surg Endosc 21(8):1406–1412. https://doi.org/10.1007/s00464-006-9177-5
Ericsson KA (2008) Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med 15(11):988–994. https://doi.org/10.1111/j.1553-2712.2008.00227.x
Kimura BJ et al (2015) Cardiac limited ultrasound examination techniques to augment the bedside cardiac physical examination. J Ultrasound Med 34(9):1683–1690. https://doi.org/10.7863/ultra.15.14.09002
Sahin I (2006) Detailed review of Rogers’ diffusion of innovations theory and educational technology-related studies based on Rogers’ theory. Turk Online J Educ Technol 5(2):14–22
Via G, Hussain A, Wells M et al (2014) International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr 27(7):683.e1–683.e33. https://doi.org/10.1016/j.echo.2014.05.001
Hellmann DB, Whiting-O’Keefe Q, Shapiro EP et al (2005) The rate at which residents learn to use hand-held echocardiography at the bedside. Am J Med 118(9):1010–1018. https://doi.org/10.1016/j.amjmed.2005.05.030
Authors’ contributions
CS and TM: study design, literature review, original writing, data collection, figure design. AM and CB: ultrasound exam scoring. EL: statistical analysis. All authors participated in manuscript editing. All authors read and approved the final manuscript.
Acknowledgements
The authors wish to thank Dr. Kevin Piro for his help in reviewing this paper and Dr. Kristy Carlson for assisting with figure design.
Competing interests
The authors declare that they have no competing interests. All authors had access to the data and a role in writing the manuscript.
Consent for publication
We obtained informed consent from all study participants.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB) of the University of Nebraska Medical Center (163-16-EX).
Funding
The study was completed with no funding.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1.
Instructions for study participants, facilitators, and standardized patients.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Smith, C.J., Morad, A., Balwanz, C. et al. Prospective evaluation of cardiac ultrasound performance by general internal medicine physicians during a 6-month faculty development curriculum. Crit Ultrasound J 10, 9 (2018). https://doi.org/10.1186/s13089-018-0090-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13089-018-0090-7