Abstract
Background
Female sterilization by tubal ligation is a safe, extremely effective, and permanent way to limit childbearing. It is the most popular modern contraceptive method worldwide. The simplest way to provide tubal ligation is by a procedure called minilaparotomy, generally performed with the client under local anesthesia with systemic sedation and analgesia. In Tanzania, unmet need for family planning is high and has declined little in the past decade. Access to tubal ligation is limited throughout the country, in large part because of a lack of trained providers. Clinical officers (COs) are midlevel health workers who provide diagnosis, treatment, and minor surgeries. They are more prevalent than physicians in poorer and rural communities. Task shifting—the delegation of some tasks to less-specialized health workers, including task shifting of surgical procedures to midlevel cadres—has improved access to lifesaving interventions in resource-limited settings. It is a cost-effective way to address shortages of physicians, increasing access to services. The primary objective of this trial is to establish whether the safety of tubal ligation by minilaparotomy provided by COs is noninferior to the safety of tubal ligation by minilaparotomy provided by physicians (assistant medical officers [AMOs]), as measured by rates of major adverse events (AEs) during the procedure and through 42 days of follow-up.
Methods/design
In this facility-based, multicenter, noninferiority randomized controlled trial, we are comparing the safety of tubal ligation by minilaparotomy performed by trained COs versus by trained AMOs. The primary outcome is safety, defined by the overall rate of major AEs occurring during the minilaparotomy procedure and through 42 days of follow-up. The trial will be conducted among 1970 women 18 years of age or older presenting for tubal ligation at 7 study sites in northern Tanzania.
Discussion
If no major safety issues are identified, the data from this trial may facilitate changes in the Tanzanian government’s regulations, allowing appropriately trained COs to provide tubal ligation by minilaparotomy. Positive findings may have broader implications. Task shifting to provide long-acting contraceptives, if proven safe, may be an effective approach to increasing contraceptive access in low- and middle-income countries.
Trial registration
ClinicalTrials.gov, NCT02944149. Registered on 14 October 2016.
Similar content being viewed by others
Background
Female sterilization by tubal ligation is a safe, extremely effective, and permanent way to limit childbearing, and it is the single most popular modern contraceptive method worldwide [1]. The simplest way to provide tubal ligation is through a procedure called minilaparotomy, which is generally performed with the client under local anesthesia with systemic sedation and analgesia. According to the World Health Organization (WHO), tubal ligation by minilaparotomy is a minor surgery that can be performed in resource-limited settings on an outpatient basis with low risk of complications [2, 3]. Although data are limited and published reports are for the most part several decades old, complication rates of 0.7–3.4% following tubal ligation by minilaparotomy performed by physicians have been reported in several countries in Africa [4,5,6,7,8,9].
Among currently married Tanzanian women 15–49 years old, 25.7% do not want to have any more children, whereas 3.4% have had a tubal ligation [10]. Although modern contraceptive use has steadily increased over the last decade, from 20% in 2004–2005 to 27% in 2010 and 32% in 2015–2016, unmet need for family planning has remained steady at 22–24% since 1999 [10]. Use of tubal ligation among currently married women has more than doubled, from 1.6% in the early 1990s to 3.4% today; however, it represents only about 11% of all contraceptive use, despite the large numbers of women who desire no more children [10].
Despite a high demand for modern contraceptives, access to tubal ligation in Tanzania is limited, with 58% of hospitals and 38% of health centers offering tubal ligation services. (In some cases, only counseling is provided.) Availability is roughly evenly divided between government, private for-profit, and faith-based facilities [11]. The government of Tanzania (GOT) recognizes that most health facilities in the country are understaffed, with the greatest need in rural areas, and that a lack of trained providers significantly limits the availability of services, including tubal ligation [12]. Clinical officers (COs) are midlevel providers who diagnose and treat illnesses and perform minor surgeries. They outnumber physicians, both medical officers (MOs) and assistant medical officers (AMOs), by a 2:1 ratio, and they are more prevalent in rural communities [11].
Task shifting, described as delegation or shifting of some tasks to less-specialized health workers, is one method used to expand the health workforce [13, 14]. Task shifting of surgical procedures to midlevel cadres, including COs, has improved access to lifesaving interventions in resource-limited settings and is considered a safe and cost-effective way to address physician shortages [15]. Two recent systematic reviews of older studies, as well as two recent small-scale studies in Uganda and Malawi, suggest that task-shifting tubal ligation via minilaparotomy to nonphysician clinicians is safe, although available evidence is limited and well-designed clinical trials are needed to definitively demonstrate safety, efficacy, and acceptability of task-shifting the procedure to midlevel providers [16,17,18,19]. WHO guidelines on optimizing health workers’ roles for maternal and newborn health include COs among those considered competent to provide tubal ligation; however, the recommendation was not based on a review of evidence [20].
Task shifting of tubal ligation by minilaparotomy to COs would increase access to tubal ligation for many Tanzanian women who are most in need and is of interest to the GOT as a way to assist in meeting the needs of the growing numbers of women seeking permanent contraception. With this in mind, the primary objective of the present study is to establish whether the safety of tubal ligation by minilaparotomy, as measured by rates of major adverse events (AEs) during study participation, when provided by trained COs is noninferior to the safety of the procedure when provided by trained AMOs.
Methods/design
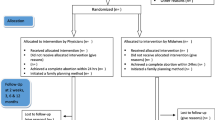
This study is a noninferiority randomized controlled trial (RCT) comparing the safety of tubal ligation by minilaparotomy conducted by trained COs and by trained AMOs in Tanzania. We will randomize a total of 1970 women 18 years of age and older presenting at 7 sites for tubal ligation in a 1:1 ratio to have the procedure done by a CO or an AMO. In addition to the screening and enrollment/tubal ligation visit, there will be three scheduled follow-up visits at 3, 7, and 42 days postsurgery. Figure 1 depicts the flow of study participants. We have included a Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) checklist in Additional file 1.
Intervention
The study intervention is tubal ligation via minilaparotomy conducted by a CO in the intervention arm and by an AMO is the control arm. To ensure adequate skills to perform minilaparotomy, COs and AMOs (none of whom had prior experience performing tubal ligation by minilaparotomy) participated in competency-based training according to GOT guidelines and standards prior to the start of the study [21].
Outcome measures
The primary objective is to establish whether the safety of tubal ligation by minilaparotomy as provided by COs is noninferior to the safety of tubal ligation by minilaparotomy as provided by AMOs. The primary study outcome is safety, defined by the overall rate of major AEs observed during the procedure and through 42 days of follow-up. We will compare the rate of major AEs observed following procedures conducted by COs with that of procedures performed by AMOs. Major AEs include the following:
-
1.
Injuries to abdominal viscera, pelvic abscess, or severe peritonitis leading to unintended major surgery
-
2.
Severe intra- or immediate postoperative hemorrhage requiring blood transfusion
-
3.
Febrile morbidity (oral temperature > 38 °C on at least 2 postoperative days, excluding the first 24 h after surgery)
-
4.
Life-threatening event (including cardiopulmonary crisis or anaphylaxis)
-
5.
Readmission to the hospital any time after discharge after the procedure through the end of follow-up, owing to a complication related to the minilaparotomy procedure
-
6.
Death or complication resulting in death occurring within 42 days of the surgery related to the minilaparotomy procedure
Secondary objectives and their outcomes include comparison of the following:
-
1.
The safety of tubal ligation by minilaparotomy provided by COs versus AMOs as measured by AE rates (major and minor) at different points in time (intraoperatively, immediately postoperatively, and at each follow-up visit)
-
2.
The performance (e.g., procedure times, difficulties performing the procedure, inability to complete the procedure, need for assistance to complete the procedure, and maximum reported pain experienced by the participant during the procedure) of COs versus AMOs for conducting tubal ligation by minilaparotomy
-
3.
Participant satisfaction with the tubal ligation conducted by COs versus AMOs
-
4.
The self-efficacy of COs versus AMOs in performing tubal ligation by minilaparotomy, defined by provider confidence, comfort, and perception of their ability to perform the procedure
Detailed definitions of the primary and secondary outcomes, including the domain (name of the outcome), specific measurement, metric, method of aggregation, and time point for measurement can be found in Table 1.
Study sites
We will conduct the study at seven sites based at health care facilities in northern Tanzania (Table 2). In addition to provision of tubal ligation services at these seven static sites, we will use outreach approaches that are currently part of the GOT’s approach to increasing access to family planning. During outreach events, the trained COs and AMOs from the seven static study sites will travel to and perform procedures at other facilities where tubal ligation is not routinely available. All seven of the static study sites, as well as the outreach sites, are currently part of the GOT family planning program, with tubal ligation by minilaparotomy normally provided by physicians who are not among the providers included in the study.
Study population and eligibility criteria
We will recruit a total of 1970 participants from among women presenting at static or outreach study sites for tubal ligation. Study staff will ask women if they are potentially interested in participating in the study after they have undergone the standard GOT family planning counseling, chosen tubal ligation as the contraceptive option of their choice, and signed the GOT informed consent documents for the tubal ligation procedure.
We will randomize women if they meet any of the following criteria:
-
1.
Are aged 18 years or older
-
2.
Requested and consented (in accordance with GOT procedures) to tubal ligation and additionally freely consented to participate in the study and signed a study informed consent form
-
3.
Are of sound mind, are in good general health, and are deemed suitable to undergo tubal ligation by minilaparotomy in accordance with the GOT guidelines [21]
-
4.
Are able to understand study procedures and the requirements of study participation
-
5.
Agree to return to the study site for the full schedule of follow-up visits
-
6.
Agree to provide the study staff with an address, phone number, name of a close relative, and/or other locator information while participating in the research study
We will exclude women if they meet any of the following criteria:
-
1.
Are pregnant
-
2.
Are between 8 and 42 days postpartum or postabortion
-
3.
Have a known allergy or sensitivity to lidocaine or other local anesthesia
-
4.
Take a medication that would be a contraindication for elective surgery, such as an anticoagulant or steroid
-
5.
Have had previous abdominal or pelvic surgery
-
6.
Have a local skin infection near the area where the incision will be made
-
7.
Have severe anemia (regardless of type or etiology), a coagulation disorder, hypertension (properly taken measurements: systolic pressure ≥ 160 mmHg or diastolic pressure ≥ 100 mmHg), acute deep venous thrombosis/pulmonary embolism, or current ischemic heart disease
-
8.
Have unexplained vaginal bleeding; malignant gestational trophoblastic disease; cervical, endometrial, and/or ovarian cancer; pelvic inflammatory disease (current or within the last 3 months); or current purulent cervicitis, chlamydial infection, and/or gonorrhea
-
9.
Have current symptomatic gallbladder disease, active viral hepatitis, tuberculosis of pelvic organs, acute bronchitis or pneumonia, or systematic infection or gastroenteritis
-
10.
Are currently participating in another biomedical research study
Generation of allocation sequence and random allocation
We used permuted blocks within the site for the randomization to ensure similarity of groups with regard to potential confounding factors. A researcher unaffiliated with the study generated by computer the random allocation sequence centrally at EngenderHealth headquarters in New York City. Randomization is in a 1:1 ratio (minilaparotomy conducted by a CO or minilaparotomy conducted by an AMO), stratified by study site, and restricted with randomly varying block sizes of four to eight within the strata. We will recruit participants at all study sites until the total sample size has been reached. A research assistant at each site will randomize participants after screening has been conducted, a woman’s eligibility for study participation has been confirmed, and just prior to start of the minilaparotomy procedure. We will achieve random allocation concealment by using a text message service (Sealed Envelope Ltd. [www.sealedenvelope.com], London, UK). Because of the nature of the services and low availability of clinical staff at study sites, it is not possible to mask participants, coinvestigators, those assessing outcomes, or other study staff to treatment allocation.
Rationale for the noninferiority hypothesis and sample size calculation
The primary objective of this study is to determine whether the rate of major AEs following tubal ligation by minilaparotomy conducted by trained COs is not worse by more than a minimal relevant difference than the AE rate following tubal ligation by minilaparotomy conducted by trained AMOs. This question lends itself to a noninferiority design. The choice of the noninferiority margin (i.e., the smallest clinical difference that is acceptable between the two treatments) is based on a combination of clinical judgment and statistical reasoning. In the case of major AEs following tubal ligation by minilaparotomy, data from prior trials (n = 12) suggest an average AE rate of 3.85% (95% CI 3.15–4.54%). After removing the one trial that is an outlier, in terms of both sample size and AE rate, we calculated the average as 1.59% (95% CI 0.90–2.28%) (Table 3).
These data suggest that an absolute rate of approximately 3% would be expected and that we would expect no greater than 5%, based on the upper limit of the 95% CI. In addition, in the clinical judgment of EngenderHealth staff and outside experts, we have determined that a noninferiority margin of 2% is appropriate because it implies that up to a 5% AE rate would be clinically acceptable. In other words, if the upper limit of the two-sided 95% CI for the difference in AE rates (CO minus AMO) lies fully to the left of the 2% noninferiority margin, we will have proved noninferiority of tubal ligation by minilaparotomy conducted by COs at a level of significance of α = 0.05.
Assuming a 3% major AE rate in the control group (AMOs), we will demonstrate noninferiority within the margin of 2% at a one-sided significance level of α = 0.05 and a power of 80% (calculated when AE rates in both arms are the same) with a sample size of 895 per arm (1790 women in total). Adjusting by 10% for loss to follow-up, protocol violations, and withdrawals, this would result in a total sample size of 1969 women, rounded to 1970.
Data collection procedures and participant pathway
Data will be collected for all women who consent to participate using electronic case report forms (eCRFs) we developed for the study and programmed with Open Data Kit Collect (University of Washington, Department of Computer Science and Engineering, Seattle, WA, USA; https://opendatakit.org/) on Tecno PhonePad 7II tablets (TECNO Mobile, Hong Kong, China; www.tecno-mobile.com). A summary of the schedule of enrollment, interventions, and assessments is shown in Table 4. We trained study staff on data collection using the eCRFs prior to the start of recruitment. We will routinely assess the data throughout the study for inconsistencies and common errors as well as to identify missing values or missing records. We will resolve missing data to the greatest extent possible.
After informed consent has been obtained by a research assistant, a study provider will evaluate each potential participant for clinical eligibility according to the study inclusion and exclusion criteria noted above. If eligible, a research assistant will randomize participants, and the minilaparotomy procedure will be done on the same visit in most cases (or, if not, within 7 days of screening). Providers will conduct tubal ligation procedures according to the GOT guidelines [21]. We have not placed any restrictions on clinical care that a provider deems necessary for the health and well-being of study participants, although we will collect data on all relevant concomitant care and interventions provided before or during the procedure, as well as during the follow-up period.
We will ask participants to return for three scheduled follow-up visits at 3, 7, and 42 days postsurgery. A research assistant will call or text participants the day before each scheduled visit to remind them to come for follow-up. If a participant misses a visit, a research assistant will attempt to contact the participant three times to encourage him/her to come for the visit. We will give participants 5000 Tanzanian shillings (approximately $2.25) to cover time and transport cost to/from the study site for each of the three scheduled follow-up visits. A provider may schedule additional visits if clinically necessary, and we will inform participants that they should return to the site at any time if they have problems or concerns related to the procedure.
We will collect data at three time points:
-
1.
Prior to the minilaparotomy procedure, we will record detailed information on sociodemographic characteristics, obstetric and family planning use history, and physical examination findings.
-
2.
At the time of surgery, we will gather details of the anesthesia and procedure, including problems encountered, assistance needed, and occurrence of AEs.
-
3.
We will record information on physical examination findings, AEs, and participants’ experience and satisfaction postsurgery; during recovery; and at 3, 7, and 42 days after surgery, as well as during any unscheduled follow-up visits.
-
4.
At the end of the study, we will collect information from the COs and AMOs on self-efficacy, including measures of general self-efficacy, and confidence and comfort conduting minilaparotomy.
Once an individual eCRF is completed, a research assistant will encrypt the data on the tablets and upload it through a secure connection to the database located on a server in EngenderHealth’s office in Dar es Salaam, Tanzania. Detailed procedures for the collection, management, and use of the data are outlined in a study data management plan.
Providers will assess participants for the presence of AEs during the minilaparotomy procedure and postoperative period, as well as at all scheduled and unscheduled follow-up visits, and provide treatment/referral and follow-up as clinically indicated. We will collect detailed data on AEs in the eCRFs, including type, severity, relatedness to the minilaparotomy procedure, treatment, and outcome. We will report serious AEs resulting in death to the institutional review boards (IRBs) within 24 h of when the principal investigator (PI) is notified and those resulting in hospitalization within 10 days of notification of the PI.
We will also monitor for social harm events (SHEs) such as loss of privacy, stigmatization, relationship difficulties, physical or verbal abuse, and interference with gainful employment. We will help participants address any reported SHEs or refer them to available support services appropriate for the SHE. We will report SHEs potentially related to study participation to the IRBs within 10 days of when the PI is notified. During the study, an independent clinical trial monitor will conduct periodic on-site monitoring visits as needed to ensure that the study is being conducted and informed consent is being obtained according to the approved protocol, good clinical practice standards, and applicable regulatory guidelines, as well as to monitor recruitment and data quality.
Statistical methods
We will develop a detailed analysis plan that covers both the final analysis and the planned interim analysis prior to initiation of the analysis. The primary outcome of the trial is major AEs within 42 days of the tubal ligation by minilaparotomy (i.e., the proportion of participants experiencing a major AE by day 42 postsurgery) in an intention-to-treat (ITT) analysis. We will conduct the primary analysis for the ITT population. The ITT population would include participants for whom the protocol is violated (i.e., participants who are randomized to have their procedure done by a CO but in fact have the procedure done by an AMO, or participants who are randomized to have their procedure done by an AMO but in fact have the procedure done by a CO) and withdrawals/discontinuations. We will also conduct a per-protocol analysis for the primary outcome if we have participants who do not receive the treatment to which they were randomly allocated.
Unlike a superiority trial, where the treatment effect is the primary parameter of interest, the interpretation of a noninferiority trial’s results depends on the location of the CI for the effect of the experimental treatment relative to the margin of noninferiority and a null effect [22]. The primary analysis will be interpreted as follows. If the whole 95% CI lies above the noninferiority margin of 2%, the experimental intervention will be declared “inferior.” If the whole 95% CI lies below the noninferiority margin, the intervention will be considered to be “noninferior” to the standard treatment. If the 95% CI includes the noninferiority margin, study results will be deemed inconclusive. Finally, if the entire 95% CI lies completely below zero, the new treatment may be considered superior to the standard treatment.
We will conduct other analyses on primary and secondary outcomes related to tubal ligation by minilaparotomy, including AE rates (overall and per time point), measures of performance (e.g., procedure times, difficulties performing the procedure, inability to complete the procedure), and participant satisfaction. We will analyze data on key demographic and reproductive variables (e.g., age, education level, marital status, occupation, ethnicity, parity) to generate a profile of study participants undergoing tubal ligation by minilaparotomy at study sites. We will analyze data on key provider-level variables to generate a profile of providers, disaggregated by provider type (CO and AMO). Methods of analysis for each secondary outcome are shown in Table 1 above.
We will include data in the analyses for all outcomes for participants who withdraw or are discontinued in the study through the time their study participation ends. We will not consider observations with missing data in the analyses and will not impute any missing data.
We have recruited a three-member data and safety monitoring board (DSMB) with no direct involvement in the study, including a surgeon experienced with tubal ligation by minilaparotomy, an epidemiologist, and a statistician. The role of the DSMB will be to deal with any ethical and safety issues that may arise during the trial and to review an interim analysis. We will conduct the interim analysis after approximately one-third of the sample has had the minilaparotomy procedure and completed the 7-day follow-up visit. At the time of the interim analyses, we will provide the DSMB with safety and study quality data (e.g., recruitment and follow-up rates, protocol violations), unmasked by treatment group.
We will ask the DSMB to give advice regarding stopping the trial if they have proof beyond doubt of an important advantage or disadvantage for one of the treatment groups and if they consider that the results are likely to affect clinical practice. For the primary outcome (i.e., major AEs), the following stopping guidelines have been proposed for the DSMB:
-
1.
At the time of the interim analysis, the DSMB may recommend stopping the study or temporarily halting recruitment if there are significantly more major AEs in one randomization group than in the other; a difference between the two treatment arms will be considered significant if the p value is < 0.001 [23].
-
2.
In the event that the interim analysis shows notably higher rates of major AEs in the study participants overall (i.e., both study arms) relative to the generally accepted AE rates following tubal ligation by minilaparotomy (e.g., a > 5% rate, which is the upper limit of the 95% CI in previously published studies), the DSMB may recommend stopping the study or temporarily halting recruitment.
-
3.
The DSMB may also recommend stopping the study, temporarily halting recruitment, or adjusting study sites if it seems that recruitment is not proceeding at rates that will allow the study to reach its target sample size within a reasonable time frame.
If the study is stopped temporarily or permanently for any reason, we will continue to follow participants already enrolled for the planned follow-up period (and longer, if necessary, based on clinical indications). We will continue to provide enrolled participants with clinical care as necessary. According to the charter agreed to by the DSMB members before the start of the trial, their role will be as advisors to the investigators; the latter will be responsible for making decisions regarding temporarily or permanently stopping recruitment.
The PI will have responsibility for informing relevant parties (e.g., other investigators, study site personnel, IRBs, trial participants, trial registries), or ensuring they are informed, of any important protocol modifications or other information pertinent to conduct of the trial via email or phone or in person in a timely fashion, depending on the nature and urgency of the information.
Discussion
If no major safety or other issues are identified, the data from this trial may facilitate changes in the GOT regulations, allowing appropriately trained COs to provide tubal ligation by minilaparotomy. We have reason to be optimistic that COs will be able to safely perform tubal ligations by minilaparotomy. As mentioned previously, two recent systematic reviews and results of two recent small-scale studies provide data supporting the safety of task-shifting tubal ligation by minilaparotomy to nonphysician clinicians [16,17,18,19]. Moreover, surgical task-shifting initiatives have been reported to be successful in various African countries, including Malawi [24], Mozambique [25,26,27], and Tanzania [28], with COs and nurses demonstrating success similar to that of their higher-level counterparts in performing cesarean deliveries and other major surgical procedures more complex than tubal ligation by minilaparotomy.
If our results demonstrate that tubal ligation by minilaparotomy provided by COs is noninferior to provision by AMOs, leading to revised guidelines by the GOT and training of COs to provide tubal ligation by minilaparotomy in Tanzania, access to a very effective permanent method of contraception would increase dramatically for thousands of women, given the more widespread availability of COs at health facilities around the country relative to physicians. Three-fourths of the population of Tanzania lives in rural areas; yet, only 31% of physicians are stationed in rural areas, in contrast to 72% of COs [29]. The need for female surgical contraceptive services in Tanzania is critically urgent. If current trends continue, the number of women of reproductive age (15–49 years old) choosing female sterilization by 2020 will be more than 65,000 annually, almost a doubling of demand since 2011 [30].
Positive findings may have broader implications; task shifting to provide long-term contraceptives, if proven safe, may be an effective approach to increasing contraceptive access in many low- and middle-income countries. The results of our large-scale RCT will provide definitive data to support or refute provision of tubal ligation by minilaparotomy conducted by nonphysician clinicians and may lead to changes in government regulations in a variety of countries.
Following completion of the study, we will submit a report to United States Agency for International Development/Tanzania and to the GOT. Additionally, we will prepare policy and technical briefs for dissemination to a wide audience, dependent on the outcome of the study. Regardless of study outcomes, the research team will hold dissemination meetings with key district, regional, and national stakeholders in Tanzania. Given the likely wide potential interest and importance of the results in the international family planning community, we will also disseminate the results in at least one publication in a peer-reviewed journal and at one or more international scientific conferences. We will follow the authorship guidelines of the International Committee of Medical Journal Editors, whereby each author is required to (1) have made substantial contributions to the conception or design of the work or to the acquisition, analysis, or interpretation of data for the work; (2) have made substantial contributions to drafting the work or revising it critically for important intellectual content; (3) approve the final version to be published; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. We do not intend to use professional writers.
We do not plan to disseminate the results among research participants, because the vast majority will not be returning to the facility after their final follow-up visit is complete. Moreover, the intervention being tested is a service delivery approach and is not related to participant behaviors; thus, the communities of interest for dissemination of results are government officials, policymakers, and family planning program managers and providers.
Trial status
Enrollment began on 6 December 2016 and was completed on 16 June 2017. Follow-up was completed on 28 July 2017.
Abbreviations
- AE:
-
Adverse event
- AMO:
-
Assistant medical officer
- CO:
-
Clinical officer
- DSMB:
-
Data and safety monitoring board
- eCRF:
-
Electronic case report form
- GOT:
-
Government of Tanzania
- IRB:
-
Institutional review board
- ITT:
-
Intention to treat
- MO:
-
Medical officer
- PI:
-
Principal investigator
- RCT:
-
Randomized controlled trial
- SHE:
-
Social harm event
- SPIRIT:
-
Standard Protocol Items: Recommendations for Interventional Trials
- WHO:
-
World Health Organization
References
Darroch JE. Trends in contraceptive use. Contraception. 2013;87:259–63.
World Health Organization (WHO). Female sterilization: a guide to provision of services. Geneva: WHO; 1992.
Kulier R, Boulvain M, Walker D, Candolle G, Campana A. Minilaparotomy and endoscopic techniques for tubal sterilisation. Cochrane Database Syst Rev. 2004;3:CD001328.
Cisse CT, Kerby K, Cisse ML, Diallo D, Faye EO, Moreira PM, et al. Complications of tubal sterilization by minilaparotomy under local anesthesia [in French]. Dakar Med. 1997;42:96–8.
Ruminjo J, Ngugi F. Safety issues in voluntary female surgical contraception: perioperative complications. J Obstet Gynaecol East Cent Africa. 1993;11:24–8.
Ruminjo J, Ngugi F. Early and medium-term morbidity of minilaparotomy female sterilisation in Kenya. East Afr Med J. 1992;69:636–9.
Doh A, Kamdom-Moyo J, Kouam L. Minilaparotomy tubal ligation in the immediate post-partum after vaginal delivery. A retrospective analysis of 253 cases in the maternity service of the Yaounde University Hospital Center (Cameroon). Contracept Fertil Sex. 1996;24:49–51.
Jack KE, Chao CR. Female voluntary surgical contraception via minilaparotomy under local anesthesia. Int J Gynaecol Obstet. 1992;39:111–6.
Kidan KG, Azeze B, Ismail S. Female sterilisation through mini-laparotomy at Gondar College of Medical Sciences. East Afr Med J. 2001;78:414–7.
Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania, Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF. Demographic and health survey and malaria indicator survey (TDHS-MIS) 2015–16. Dar es Salaam and Rockville: MoHCDGEC, MoH, NBS, OCGS, and ICF; 2016.
Ministry of Health and Social Welfare (MoHSW) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF International. Tanzania Service Provision Assessment Survey (TSPA) 2014–15. Dar es Salaam and Rockville: MoHSW, MoH, NBS, OCGS, and ICF International; 2015. https://dhsprogram.com/pubs/pdf/SPA22/SPA22.pdf.
Munga MA, Songstad NG, Blystad A, Maestad O. The decentralisation-centralisation dilemma: recruitment and distribution of health workers in remote districts of Tanzania. BMC Int Health Hum Rights. 2009;9:9.
World Health Organization (WHO). Task shifting to tackle health worker shortages. Geneva: WHO; 2007.
World Health Organization (WHO). Treat, train, retain: task shifting global recommendations and guidelines. Geneva: WHO; 2008.
Hounton SH, Newlands D, Meda N, De Brouwere V. A cost-effectiveness study of caesarean-section deliveries by clinical officers, general practitioners and obstetricians in Burkina Faso. Hum Resour Health. 2009;7:34.
Polus S, Lewin S, Glenton C, Lerberg PM, Rehfuess E, Gülmezoglu AM. Optimizing the delivery of contraceptives in low- and middle-income countries through task shifting: a systematic review of effectiveness and safety. Reprod Health. 2015;12:27.
Rodriguez MI, Gordon-Maclean C. The safety, efficacy and acceptability of task sharing tubal sterilization to midlevel providers: a systematic review. Contraception. 2014;89:504–11.
Gordon-Maclean C, Nantayi LK, Quinn H, Ngo TD. Safety and acceptability of tubal ligation procedures performed by trained clinical officers in rural Uganda. Int J Gynaecol Obstet. 2014;124:34–7.
Chipeta-Khonje A, Ghosh S, Corby N, Ngo T. Marie Stopes ligations: complication rates and client satisfaction in Malawi. London: Marie Stopes International; 2009.
World Health Organization (WHO). Optimizing health worker roles to improve access to key maternal and newborn health interventions through task shifting. Geneva: WHO; 2012.
Tanzania Ministry of Health and Social Welfare, Reproductive and Child Health Section. National family planning training curriculum. Fourth edition. Module 3: Voluntary surgical contraception. Dar es Salaam: Ministry of Health and Social Welfare, Reproductive and Child Health Section; 2010.
Piaggio G, Elbourne DR, Pocock SJ, Evans SJW, Altman DG, CONSORT Group. Reporting of noninferiority and equivalence randomized trials. JAMA. 2012;308:2594–604.
O’Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics. 1979;35:549–56.
Fenton PM, Whitty CJ, Reynolds F. Caesarean section in Malawi: prospective study of early maternal and perinatal mortality. BMJ. 2003;327:587.
Kruk ME, Pereira C, Vaz F, Bergström S, Galea S. Economic evaluation of surgically trained assistant medical officers in performing major obstetric surgery in Mozambique. BJOG. 2007;114:1253–9.
Vaz F, Bergström S, Vaz MDL, Langa J, Bugalho A. Training medical assistants for surgery. Bull World Health Organ. 1999;77:688–91.
Pereira C, Bugalho A, Bergström S, Vaz F, Cotiro M. A comparative study of caesarean deliveries by assistant medical officers and obstetricians in Mozambique. Br J Obstet Gynaecol. 1996;103:508–12.
Beard JH, Oresanya LB, Akoko L, Mwanga A, Mkony CA, Dicker RA. Surgical task-shifting in a low-resource setting: outcomes after major surgery performed by nonphysician clinicians in Tanzania. World J Surg. 2014;38:1398–404.
Tanzania Ministry of Health and Social Welfare. Human resource for health country profile 2012/2013. Dar es Salaam: Tanzania Ministry of Health and Social Welfare; 2013.
EngenderHealth. Reality check: a planning and advocacy tool for strengthening family planning programs. Version 3. https://www.engenderhealth.org/pubs/family-planning/reality-check.php.
Chowdhury S, Chowdhury Z. Tubectomy by paraprofessional surgeons in rural Bangladesh. Lancet. 1975;2:162–3.
Fongsri A, McDaniel E. Use of nurse-midwives for minilap sterilization. Concern (Anaheim). 1979;15:13–5.
Dusitsin N, Chalapati S, Varakamin S, Boonsiri B, Ningsanon P, Gray RH. Post-partum tubal ligation by nurse-midwives and doctors in Thailand. Lancet. 1980;1:638–9.
Koetsawang S, Varakamin S, Satayapan S, Srisupandit S, Apimas SJ. Postpartum sterilization by operating-room nurses in Thailand. Int J Gynaecol Obstet. 1981;19:201–4.
Satyapan S, Varakamin S, Suwannus P, Chalapati S, Onthuam Y, Dusitsin N. Postpartum tubal ligation by nurse-midwives in Thailand: a field trial. Stud Fam Plann. 1983;14:115–8.
Kanchanasinith K, Piyapinyo P, Pitaktepsombati P, Vibulsresth S, Gates DS, Janowitz B, Robbins M. Postpartum sterilization by nurse-midwives in Thailand. Int Fam Plan Perspect. 2015;16:55–8.
Acknowledgements
The authors thank Ghazaleh Samandari for her contributions to development of the protocol; Annette Almeida, Eugene Hugho, Rehema Kahando, Makunda Kassongo, Richard Killian, Irene Mnzava, Daniel Ouma, Denis Swai, and other RESPOND Tanzania Project staff for their support in the planning and implementation of the study; the AMOs, COs, research assistants, and other staff at the study sites for their hard work that is making the study possible; and the Tanzanian women who are participating in the trial.
Funding
This study is made possible by the generous support of the American people through the United States Agency for International Development (USAID) under the terms of the RESPOND Tanzania Project (RTP), Associate Cooperative Agreement AID-621-LA-13-00001. The information provided in this protocol does not necessarily reflect the views or positions of USAID or the U.S. government. USAID had no role in the design of the study or in the writing of the manuscript.
Availability of data and materials
The full protocol, participant-level dataset, and statistical code, as well as blank copies of the informed consent and data collection forms, are available on request from the corresponding author.
Trial sponsors
United States Agency for International Development, Tanzania
-
686 Old Bagamoyo Road, Msasani, P.O. Box 9130
-
Dar es Salaam, Tanzania
-
Phone: +255 22 229 4490
RESPOND Tanzania Project, EngenderHealth
-
Plot No. 254, Mwai Kibaki Road/Kiko Avenue
-
P.O. Box 78167
-
Dar es Salaam, Tanzania
-
Phone: +255 754 005070
Tanzania Ministry of Health, Community Development, Gender, Elders, and Children
-
6 Samora Machel Avenue
-
11478 Dar es Salaam, Tanzania
-
Phone: +255 22 2342000/5
Author information
Authors and Affiliations
Contributions
MAB contributed to the design of the study, drafted the study protocol, and drafted the manuscript. ZM contributed to the design of the study, provided input into the study protocol, and critically reviewed the manuscript. JOA contributed to the design of the study, provided input into the study protocol, and critically reviewed the manuscript. CC contributed to the design of the study, provided input into the study protocol, and critically reviewed the manuscript. JK contributed to the design of the study, provided input into the study protocol, and critically reviewed the manuscript. PSM contributed to the design of the study, provided input into the study protocol, and critically reviewed the manuscript. JM contributed to the design of the study, provided input into the study protocol, and critically reviewed the manuscript. CS contributed to the design of the study, provided input into the study protocol, and critically reviewed the manuscript. LT contributed to the design of the study, provided input into the study protocol, and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial protocol (version 1, 25 September 2016) was reviewed and approved by the National Institute for Medical Research, Tanzania, Dar es Salaam, Tanzania (NIMR/HQ/R.8a/Vol.IX/2198, 16 May 2016) and the Western Institutional Review Board, Puyallup, WA, USA (study 1163682, 27 September 2016). The two ethical approvals listed above cover all seven study sites. All participants will undergo informed consent procedures, and no participant will be enrolled until the study staff has obtained legally effective (signed or witnessed) informed consent. All medical procedures in this trial are under the oversight of the Tanzania Ministry of Health, Community Development, Gender, Elderly, and Children.
Consent for publication
Consent for publication is not applicable. All participants will be assigned a trial participant number. Participants will not be identified by name on any documents or in connection with any data that leave the study sites, nor will they be reported by name in any report or publication resulting from data collected in this study.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) checklist. (DOC 124 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Barone, M.A., Mbuguni, Z., Achola, J.O. et al. Safety of tubal ligation by minilaparotomy provided by clinical officers versus assistant medical officers: study protocol for a noninferiority randomized controlled trial in Tanzanian women. Trials 18, 499 (2017). https://doi.org/10.1186/s13063-017-2235-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-017-2235-6