Abstract
Background
Transcranial direct current stimulation (tDCS) is a promising new technique to optimize the effect of regular Speech and Language Therapy (SLT) in the context of aphasia rehabilitation. The present study focuses on the effect of tDCS provided during SLT in the sub-acute stage after stroke. The primary aim is to evaluate the potential effect of tDCS on language functioning, specifically on word-finding, as well as generalization effects to verbal communication. The secondary aim is to evaluate its effect on social participation and quality of life, and its cost-effectiveness.
Methods
We strive to include 58 stroke patients with aphasia, enrolled in an inpatient or outpatient stroke rehabilitation program, in a multicenter, double-blind, randomized controlled trial with two parallel groups and 6 months’ follow-up. Patients will participate in two separate intervention weeks, with a pause of 2 weeks in between, in the context of their regular aphasia rehabilitation program. The two intervention weeks comprise daily 45-minute sessions of word-finding therapy, combined with either anodal tDCS over the left inferior frontal gyrus (1 mA, 20 minutes; experimental condition) or sham-tDCS over the same region (control condition). The primary outcome measure is word-finding. Secondary outcome measures are verbal communication, social participation, quality of life, and cost-effectiveness of the intervention.
Discussion
Our results will contribute to the discussion on whether tDCS should be implemented in regular aphasia rehabilitation programs for the sub-acute post-stroke population in terms of (cost-)effectiveness.
Trial registration
Nederlands Trail Register: NTR4364. Registered on 21 February 2014.
Similar content being viewed by others
Background
Aphasia is present in about 30 % of patients immediately after stroke [1]. In the first weeks and months, considerable recovery may occur; however, about 20 % are left with chronic deficits at 6 months post stroke [2, 3]. There is increasing support for the efficacy of Speech and Language Therapy (SLT) in order to diminish the language and communication deficits that people with aphasia encounter [4]; however, it remains a challenge to optimize the effect of aphasia therapy.
Transcranial direct current stimulation (tDCS) is a promising new technique to optimize the effect of regular SLT in the context of aphasia rehabilitation [5]. It is safe and easy to apply and has limited side effects [6]. tDCS modulates cortical excitability by delivering weak electric currents to the cortex via two electrodes applied to the skull [7]. The effect of tDCS depends on the polarity of the electrodes: anodal tDCS enhances neuronal excitability while cathodal tDCS diminishes neuronal excitability. This effect is related to a change in the resting membrane potential. Anodal tDCS leads to de-polarization, increasing the chance for an action potential, and cathodal tDCS leads to hyper-polarization [8, 9]. tDCS is also related to neuroplasticity. Specifically, processes like long-term potentiation and secretion of brain-derived neurotrophic factor (BDNF) are associated with tDCS application [10]. The potential benefits of tDCS applied during SLT have been described since 2008 [5, 11–17]. However, these studies have some methodological limitations such as small sample size and lack of randomization.
The application of tDCS to enhance the effect of SLT is associated with the notion that tDCS may have a role in rebalancing the activity of both hemispheres post stroke. Language processing is strongly lateralized to the left hemisphere (LH), at least in right-handed healthy individuals [18–21]. After LH damage and aphasia, the right hemisphere (RH), may show increased activity. Whether this increased activity in the RH is adaptive or maladaptive, is an unresolved issue [22–24]. However, most studies indicate that, in the long term, LH perilesional recruitment is associated with better aphasia recovery, while RH recruitment is related to incomplete recovery [25–27]. In line with these observations, most studies use tDCS as a tool to promote LH perilesional recruitment.
Across studies, different electrode configurations are used to promote LH perilesional recruitment. In some studies anodal tDCS [13, 15, 16] is applied either to the left inferior frontal gyrus (IFG: Broca’s area) or to the left superior temporal gyrus (Wernicke’s area), while other studies use cathodal tDCS to inhibit the RH homolog areas, so as to disinhibit the LH [14, 28]. Few studies use an individual approach for electrode configurations [11, 29]. Anodal tDCS to the left IFG, with the cathode placed on the contralateral supra-orbital region, is the most common configuration, which has been supported by studies investigating this further with functional magnetic resonance imaging (fMRI) [30, 31] and computer modeling [32]. Predominantly, tDCS studies choose word-finding therapy as the behavioral treatment component. Irrespective of electrode configurations, studies point to an additional effect of tDCS on language functioning, when combined with SLT [5, 11–17, 29].
Studies evaluating tDCS in sub-acute aphasia rehabilitation are limited [26]. Evaluating the potential of tDCS in patients with sub-acute aphasia is important, as the larger proportion of language treatment for stroke patients is provided in the sub-acute phase, during the first weeks and months post stroke. During these first months, the recovery rate is highest [33].
Therefore, the aim of the present study is to investigate the effect of tDCS in sub-acute stroke patients with aphasia who are enrolled in regular stroke rehabilitation services. In line with studies applying tDCS in the chronic stage, we use the most common electrode configuration, i.e., anodal tDCS over the left IFG as compared to sham-tDCS, in combination with disorder-oriented aphasia therapy, aimed at word-finding. The cathode is placed on the contralateral supra-orbital region.
Objective
The present study focuses on the effect of tDCS provided during SLT in the sub-acute stage after stroke. The primary aim is to evaluate the effect of tDCS on language functioning. The primary outcome measure is word-finding. Secondary outcome measures are verbal communication, social participation, quality of life, and the cost-effectiveness of the intervention.
Methods
Study design and procedure
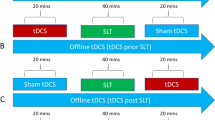
The study is a multicenter, double-blind, randomized controlled trial with two parallel groups and 6-month follow-up. Patients will participate in two separate intervention weeks, with a pause of 2 weeks in between, in the context of regular aphasia rehabilitation (see Fig. 1). During each intervention week, regular SLT sessions are replaced by daily 45-minute sessions of word-finding therapy, combined with either anodal tDCS over the left IFG (1 mA, 20 minutes; experimental condition) or sham-tDCS over the same region (control condition). The cathode is placed on the contralateral supra-orbital region. To our knowledge, a parallel design with two separate intervention weeks has not been used before in the tDCS literature. This design allows measurements before and after each intervention week, thus providing information on the recovery pattern over time within one subject.
All other therapies in the participant’s stroke rehabilitation program, such as physical therapy or occupational therapy remain unchanged and are offered following the stroke rehabilitation protocol of each participating rehabilitation center.
Setting and study population
Stroke patients with aphasia, who are receiving regular aphasia therapy, will be screened for eligibility and start the intervention between 3 weeks and 3 months after their stroke. These patients are enrolled in regular stroke rehabilitation (inpatient and outpatient services) in four rehabilitation centers in the Netherlands: Rijndam Rehabilitation (Rotterdam), Libra Rehabilitation (Tilburg and Eindhoven), Revant Rehabilitation (Breda) and De Hoogstraat Rehabilitation (Utrecht). Table 1 lists the inclusion and exclusion criteria. We strive to include 58 patients, based on a power analysis (see section Data analysis). Before inclusion, all participants need to sign the informed consent form. Patient information is provided orally as well as in written form, with extra versions in an aphasia-friendly format. This study has been approved by the Medical Ethics Committee (MEC) of the Erasmus MC, University Medical Center Rotterdam. The researcher will report serious adverse events (SAE) to the MEC and SAEs are handled according to the WMO (“Wet Medisch-wetenschappelijk Onderzoek”), the Dutch law for medical scientific research. tDCS is known to be a safe intervention with minimal side effects [6]. Participants who develop post-stroke epileptic seizures before the end of the 4-week intervention will be withdrawn from the intervention, but not from the study; all assessments will be completed (intention-to-treat analysis).
Randomization and blinding
Randomization is stratified per center of inclusion. To randomize participants to the experimental or control condition, we use a list of five-number codes, provided by the manufacturer of the stimulation device. Half of these codes activate the device to deliver anodal tDCS (experimental condition) and half of these codes deliver sham-tDCS (control condition). Codes are block randomized with a block size of four on the basis of a computer-generated sequence and then concealed in consecutively numbered, sealed, opaque envelopes. The envelope is opened at the start of the first intervention session. The participant’s unique five-number code is used to start the tDCS device, which then provides either real stimulation or sham as related to the code. The randomization and the preparation of the envelopes are done by a researcher (MH) of our research team, who is not involved in assessments and training of the patient. The key to the five-number codes is also kept by this researcher (MH). Consequently, the participants, their SLTs and the trial coordinator are blinded to treatment condition.
Intervention
In each intervention week, regular SLT sessions are replaced by daily 45-minute sessions of word-finding therapy, combined with either anodal tDCS over the left IFG (1 mA, 20 minutes; experimental condition) or sham-tDCS over the same region (control condition). Therapy is provided by speech and language therapists of the participating centers. The cathode is placed on the contralateral supra-orbital region. The intensity of 1 mA tDCS for 20 minutes and the frequency of five sessions per week is in line with most studies applying tDCS in the chronic stage [11, 13–16]. tDCS is combined with word-finding therapy, because most people with aphasia have word-finding difficulties [34]. The word-finding therapy protocol is based on Cueing Hierarchy Therapy [35]. The participant’s task is to name a picture and, based on the protocol, the therapist uses cueing techniques to help the participant to retrieve and produce the target word correctly. The cue of low stimulus power is presented first, followed by increasingly powerful cues until the correct word is retrieved and produced. Basically, the following cueing hierarchy is used: (1) “What is this?”(e.g., show picture of a tree), (2) “Can you write the word down?”, (3) graphemic cueing (e.g., provide the number of letters), (4) phonological cueing (e.g., provide the first sound, /t/), (5) semantic associations (e.g., “can you tell where you can find these”), (6) therapist says the word (e.g., “tree”), (7) repetition of the target word.
As the relative power of the cues differs across participants with aphasia, the exact cueing hierarchy is personalized. For each picture, even if the picture is named without cues, the participant is encouraged to write or copy the correct word form or, in case of inability to write, to perform an anagram task. The rationale for incorporating production of the written word, is the evidence that activating the written word has a beneficial effect on retrieving spoken words [36].
To ensure relevance of the training material for each participant, stimuli are selected on the basis of individual naming performance at baseline using the European Data Bank (EDB) for oral picture naming [37]. The first 68 items the participant is unable to name correctly within 20 s are selected. These items are divided in two sets of 34 items, matched for word length and word frequency: a therapy set, trained during the word-finding therapy, and a control set, to evaluate generalization effects to untrained items. In the first session 10 items are trained. Then, during each session new items are added, with eight new items in the second session; six new items in the third and fourth session, and four new items in the final session. For the second intervention week a new training set is selected in the same way.
tDCS
The DC Stimulator PLUS (produced by Eldith), certified as a medical device, class IIa, by the European Union Notified Body 0118 (CE 118), is used in the authorized form. Two electrodes (5 x 7 cm) are placed on the head and fixed with elastic tape; electrode placement is guided by the international 10-10 electroencephalogram (EEG) system and previous studies [15, 38, 39]. The anode is placed on the left IFG, localized as F5, and the cathode is placed on the contralateral supra-orbital region, localized as Fp2. Participants in the experimental condition receive active stimuli of 1 mA during 20 minutes. The stimulation is automatically activated with a fade in of 15 s and after 20 minutes the stimulation is automatically deactivated, with a fade out of 15 s. Participants in the control condition receive inactive stimulation (sham-tDCS), i.e., at first the stimulation is automatically activated with a fade in of 15 s, and then the stimulation is deactivated after 30 s, with a fade out of 15 s. Both the patient and the therapist are blinded for stimulation condition. The electrodes are not removed until completion of the 45-minute therapy session.
Measurement instruments
Table 2 gives an overview of the measurement instruments being used. The primary outcome measure is the score on the Boston Naming Test (BNT) [40], to assess picture-naming. Secondary outcome measures are chosen to evaluate generalization of treatment effects to verbal communication: the Aphasia Severity Rating Scale (ASRS) [41] to assess spontaneous speech and the Amsterdam Nijmegen Everyday Language Test (ANELT) [42] as a measure for verbal communication in everyday life. Other secondary outcome measures are chosen to evaluate quality of life (EuroQol-5D, [43]; Stroke and Aphasia Quality Of Life questionnaire (SAQOL), [44, 45]), social participation (Community Integration Questionnaire, [46]), and cost-effectiveness (Cost Analysis Questionnaire, [47–49]).
The primary outcome measure, BNT, is assessed before and after each intervention week (T1, T2, T3, T4) and at 6 months’ follow-up (T5); see Fig. 2. The secondary outcome measures are assessed before the first intervention week and after the second intervention week (T1, T4) and at 6 months (T5). The EuroQol-5D (EQ-5D) and the Cost Analysis Questionnaire are used to evaluate cost-effectiveness during the 4-week intervention period and during the follow-up period.
Baseline assessments (T1) include handedness (Edinburgh Handedness Inventory), aphasia severity (Shortened Token Test) [50] and overall functioning (Barthel Index) [51]. To register potential adverse effects, participants are asked to rate their discomfort immediately after each therapy session on the Wong-Baker Faces pain rating scale, a visual analog scale designed for patients with limited verbal skills [52].
To summarize the present study protocol, please see Additional file 1 for an overview of enrollment, intervention and measurement instruments, and see Additional file 2 for an overview of the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) checklist.
Sample size
The power calculation is based on the results of a randomized controlled trial by Baker et al. [11] including stroke patients in the chronic phase. In this study the group of aphasia patients trained with tDCS improved 2.1 points more than a sham-control group on a picture-naming test. Cohen’s d effect size was 0.22, which is equal to a Cohen’s f of 0.11. For the present study we calculated that, using a study design with two groups and four repeated measurements, a within-patient correlation of 0.75, an alpha of 0.05, a power of 0.80 and a Cohen’s f effect size of 0.11, we need a total group of 58 patients (29 patients in each treatment arm).
Data analysis
Once randomized, each patient will be analyzed in the group to which they were assigned, independent of potential drop-out or compliance to the protocol, according to the intention-to-treat principle. Potential baseline differences between the groups will be tested using independent t tests for continuous variables, the Mann-Whitney U test for ordinal variables, and chi-square tests for categorical variables.
Outcomes of the measures over time will be compared for the experimental condition versus the control condition using repeated measurements analysis. This analysis takes into account the correlation of repeated measurements within the same patients and it can handle missing data, assuming that data are missing at random. The dependent variable is the outcome measure and the independent variables are time and group assignment and the interaction between these variables. In these analyses, adjustments can be made for potentially confounding variables that could be unequally distributed over the groups despite the randomization procedure.
To evaluate cost-effectiveness, direct (para)medical costs and the total costs of all separate treatments by health care providers during the intervention period will be summed, as well as the costs of the facilities and materials used for these treatments. In addition, the non-medical costs, such as productivity loss, will be calculated. The incremental cost-effectiveness ratio will be calculated by dividing the difference in total costs by the difference in Quality-adjusted Life Years (QALYs), based on the EQ-5D. A net health-benefit analysis will be used to relate the costs to the benefit. We assume that the economic value of 1 life year in good health amounts to 25,000–50,000 €. The economic evaluation will be performed following the Dutch guidelines [53].
Discussion
The present study focuses on the effect of tDCS provided during SLT in the sub-acute stage after stroke. The primary aim is to evaluate the potential effect of tDCS on language functioning, specifically on word-finding, as well as generalization effects to verbal communication. The secondary aim is to evaluate its effect on social participation and quality of life, and to evaluate the cost-effectiveness of this intervention.
In line with studies applying tDCS in the chronic stage, we use the most common electrode configuration, i.e., anodal tDCS over the left IFG as compared to sham-tDCS, in combination with disorder-oriented aphasia therapy, aimed at word-finding. The application of tDCS (1 mA for 20 minutes) and the frequency is also chosen in line with studies applying tDCS in the chronic stage. However, the discussion of what may be the optimal electrode configuration and what the optimal stimulation intensity and frequency is, is still ongoing. Regarding the optimal electrode configuration, individual factors such as lesion size and the relative contribution of the RH and the LH and its relation to aphasia recovery, may lead to individual variability in response to tDCS. However, recent fMRI and computer modeling studies find that applying anodal tDCS on the left IFG [30–32] may be a suitable approach.
We expect that tDCS will enhance the speed of language recovery, resulting in improved communication, quality of life and participation – associated with decreased rehabilitation consumption and cost reduction. If we find that tDCS enhances the effect of SLT in an early phase provided that adverse effects are limited at this stage post stroke, and if it is found to be cost-effective, tDCS may be implemented in regular aphasia rehabilitation programs for the sub-acute post-stroke population.
Trial status
The inclusion of the study started on 17 April 2014 and on 2 May 2016 we had included 44 participants. We expect that the inclusion and the follow-up measurements will be completed in April 2017.
Abbreviations
ANELT, Amsterdam Nijmegen Everyday Language Test; ASRS, Aphasia Severity Rating Scale; BDNF, brain-derived neurotrophic factor; BNT, Boston Naming Test; CIQ, Communication Integration Questionnaire; EDB, European Data Bank; EQ-5D, EuroQol-5D; IFG, inferior frontal gyrus; LH, left hemisphere; QALYs, Quality-adjusted Life Years; RH, right hemisphere; SAQOL, Stroke and Aphasia Quality Of Life; SLT, Speech and Language Therapy; tDCS, transcranial direct current stimulation.
References
Engelter ST, Gostynski M, Papa S, Frei M, Born C, Ajdacic-Gross V, et al. Epidemiology of aphasia attributable to first ischemic stroke: incidence, severity, fluency, etiology, and thrombolysis. Stroke. 2006;37(6):1379–84.
Maas MB, Lev MH, Ay H, Singhal AB, Greer DM, Smith WS, et al. The prognosis for aphasia in stroke. J Stroke Cerebrovasc Dis. 2012;21(5):350–7.
El Hachioui H, Lingsma HF, van de Sandt-Koenderman ME, Dippel DW, Koudstaal PJ, Visch-Brink EG. Recovery of aphasia after stroke: a 1-year follow-up study. J Neurol. 2013;260(1):166–71.
Brady MC, Kelly H, Godwin J, Enderby P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev. 2012;5:CD000425.
Monti A, Ferrucci R, Fumagalli M, Mameli F, Cogiamanian F, Ardolino G, et al. Transcranial direct current stimulation (tDCS) and language. J Neurol Neurosurg Psychiatry. 2013;84(8):832–42.
Poreisz C, Boros K, Antal A, Paulus W. Safety aspects of transcranial direct current stimulation concerning healthy subjects and patients. Brain Res Bull. 2007;72(4-6):208–14.
Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527(Pt 3):633–9.
Antal A, Kincses TZ, Nitsche MA, Bartfai O, Paulus W. Excitability changes induced in the human primary visual cortex by transcranial direct current stimulation: direct electrophysiological evidence. Invest Ophthalmol Vis Sci. 2004;45(2):702–7.
Nitsche MA, Fricke K, Henschke U, Schlitterlau A, Liebetanz D, Lang N, et al. Pharmacological modulation of cortical excitability shifts induced by transcranial direct current stimulation in humans. J Physiol. 2003;553(Pt 1):293–301.
Fritsch B, Reis J, Martinowich K, Schambra HM, Ji Y, Cohen LG, et al. Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron. 2010;66(2):198–204.
Baker JM, Rorden C, Fridriksson J. Using transcranial direct-current stimulation to treat stroke patients with aphasia. Stroke. 2010;41(6):1229–36.
Floel A, Meinzer M, Kirstein R, Nijhof S, Deppe M, Knecht S, et al. Short-term anomia training and electrical brain stimulation. Stroke. 2011;42(7):2065–7.
Fridriksson J, Richardson JD, Baker JM, Rorden C. Transcranial direct current stimulation improves naming reaction time in fluent aphasia: a double-blind, sham-controlled study. Stroke. 2011;42(3):819–21.
Kang EK, Kim YK, Sohn HM, Cohen LG, Paik NJ. Improved picture naming in aphasia patients treated with cathodal tDCS to inhibit the right Broca’s homologue area. Restor Neurol Neurosci. 2011;29(3):141–52.
Marangolo P, Fiori V, Calpagnano MA, Campana S, Razzano C, Caltagirone C, et al. tDCS over the left inferior frontal cortex improves speech production in aphasia. Front Hum Neurosci. 2013;7:539.
Marangolo P, Fiori V, Campana S, Calpagnano MA, Razzano C, Caltagirone C, et al. Something to talk about: enhancement of linguistic cohesion through tdCS in chronic non fluent aphasia. Neuropsychologia. 2014;53:246–56.
Monti A, Cogiamanian F, Marceglia S, Ferrucci R, Mameli F, Mrakic-Sposta S, et al. Improved naming after transcranial direct current stimulation in aphasia. J Neurol Neurosurg Psychiatry. 2008;79(4):451–3.
Knecht S, Deppe M, Drager B, Bobe L, Lohmann H, Ringelstein E, et al. Language lateralization in healthy right-handers. Brain. 2000;123(Pt 1):74–81.
Knecht S, Drager B, Deppe M, Bobe L, Lohmann H, Floel A, et al. Handedness and hemispheric language dominance in healthy humans. Brain. 2000;123(Pt 12):2512–8.
Springer JA, Binder JR, Hammeke TA, Swanson SJ, Frost JA, Bellgowan PS, et al. Language dominance in neurologically normal and epilepsy subjects: a functional MRI study. Brain. 1999;122(Pt 11):2033–46.
Lurito JT, Dzemidzic M. Determination of cerebral hemisphere language dominance with functional magnetic resonance imaging. Neuroimaging Clin N Am. 2001;11(2):355–63. x.
de Aguiar V, Paolazzi CL, Miceli G. tDCS in post-stroke aphasia: the role of stimulation parameters, behavioral treatment and patient characteristics. Cortex. 2015;63:296–316.
Heiss WD, Karbe H, Weber-Luxenburger G, Herholz K, Kessler J, Pietrzyk U, et al. Speech-induced cerebral metabolic activation reflects recovery from aphasia. J Neurol Sci. 1997;145(2):213–7.
Anglade C, Thiel A, Ansaldo AI. The complementary role of the cerebral hemispheres in recovery from aphasia after stroke: a critical review of literature. Brain Inj. 2014;28(2):138–45.
Saur D, Lange R, Baumgaertner A, Schraknepper V, Willmes K, Rijntjes M, et al. Dynamics of language reorganization after stroke. Brain. 2006;129(Pt 6):1371–84.
Bonilha L, Gleichgerrcht E, Nesland T, Rorden C, Fridriksson J. Success of anomia treatment in aphasia is associated with preserved architecture of global and left temporal lobe structural networks. Neurorehabil Neural Repair. 2015;6:30(3).
Thiel A, Habedank B, Herholz K, Kessler J, Winhuisen L, Haupt WF, et al. From the left to the right: how the brain compensates progressive loss of language function. Brain Lang. 2006;98(1):57–65.
You DS, Kim DY, Chun MH, Jung SE, Park SJ. Cathodal transcranial direct current stimulation of the right Wernicke’s area improves comprehension in subacute stroke patients. Brain Lang. 2011;119(1):1–5.
Shah-Basak PP, Norise C, Garcia G, Torres J, Faseyitan O, Hamilton RH. Individualized treatment with transcranial direct current stimulation in patients with chronic non-fluent aphasia due to stroke. Front Hum Neurosci. 2015;9:201.
Holland R, Leff AP, Josephs O, Galea JM, Desikan M, Price CJ, et al. Speech facilitation by left inferior frontal cortex stimulation. Curr Biol. 2011;21(16):1403–7.
Meinzer M, Antonenko D, Lindenberg R, Hetzer S, Ulm L, Avirame K, et al. Electrical brain stimulation improves cognitive performance by modulating functional connectivity and task-specific activation. J Neurosci. 2012;32(5):1859–66.
Galletta EE, Cancelli A, Cottone C, Simonelli I, Tecchio F, Bikson M, et al. Use of computational modeling to inform tDCS electrode montages for the promotion of language recovery in post-stroke aphasia. Brain Stimul. 2015;8(6):1108–1115.
Mally J. Non-invasive brain stimulation (rTMS and tDCS) in patients with aphasia: mode of action at the cellular level. Brain Res Bull. 2013;98:30–5.
Kohn SE, Goodglass H. Picture-naming in aphasia. Brain Lang. 1985;24(2):266–83.
Linebaugh CW, Shisler RJ, Lehner L. Cueing hierarchies and word retrieval: A therapy program. Aphasiology. 2005;19:77–92.
Nickels LA. Therapy for naming disorders: revisiting, revising, and reviewing. Aphasiology. 2002;16:935–79.
Kremin H, Akhutina T, Basso A, Davidoff J, De Wilde M, Kitzing P, et al. A cross-linguistic data bank for oral picture naming in Dutch, English, German, French, Italian, Russian, Spanish, and Swedish (PEDOI). Brain Cogn. 2003;53(2):243–6.
Marangolo P, Fiori V, Caltagirone C, Marini A. How Conversational Therapy influences language recovery in chronic non-fluent aphasia. Neuropsychol Rehabil. 2013;23(5):715–31.
ldt. TCT. 10/20 positioning manual. 2012.
Kaplan EGH, Weintraub S. The Boston naming test. Philadelphia: Lea and Febiger; 1983.
Goodglass H, Kaplan E. The assessment of aphasia and related disorders. Philadelphia: Lea and Febiger; 1972.
Blomert L. Assessment and recovery of verbal communication in aphasia. PhD thesis. The Netherlands: Katholieke Universiteit Nijmegen; 1994.
Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72.
Hilari K, Byng S, Lamping DL, Smith SC. Stroke and Aphasia Quality of Life Scale-39 (SAQOL-39): evaluation of acceptability, reliability, and validity. Stroke. 2003;34(8):1944–50.
Hilari K, Lamping DL, Smith SC, Northcott S, Lamb A, Marshall J. Psychometric properties of the Stroke and Aphasia Quality of Life Scale (SAQOL-39) in a generic stroke population. Clin Rehabil. 2009;23(6):544–57.
Dalemans RJ, de Witte LP, Beurskens AJ, van den Heuvel WJ, Wade DT. Psychometric properties of the community integration questionnaire adjusted for people with aphasia. Arch Phys Med Rehabil. 2010;91(3):395–9.
Bouwmans C, Hakkaart-van Roijen L, Koopmanschap M, Krol M, Severens H, Brouwer W. Handleiding iMTA Medical Cost Questionnaire (iMCQ). Rotterdam: iMTA, Erasmus Universiteit Rotterdam; 2013.
Bouwmans C, Hakkaart-van Roijen L, Koopmanschap M, Krol M, Severens H, Brouwer W. Handleiding iMTA Productivity Cost Questionnaire (iPCQ). Rotterdam: iMTA, Erasmus Universiteit; 2013.
Bouwmans C, De Jong K, Timman R, Zijlstra-Vlasveld M, Van der Feltz-Cornelis C, Tan Swan S, et al. Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv Res. 2013;13:217.
De Renzi E, Faglioni P. Normative data and screening power of a shortened version of the Token Test. Cortex. 1978;14:41–9.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–5.
Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988;14(1):9–17.
Hakkaart-van Roijen L, Tan SS, Bouwmans CAM. Handleiding voor kostenonderzoek, methoden en standaard kostprijzen voor economische evaluaties in de gezondheidszorg. Diemen: College voor zorgverzekeringen; 2010.
Acknowledgements
This study is funded by the Erasmus MC, University Medical Center Rotterdam, and the “Hersenstichting.”
Authors’ contributions
KS is the study coordinator and will primarily acquire and analyze the data. The study design was conceived by MS, who is the principal investigator of the study. MH was involved in the statistical methods of the study design and will be involved in the statistical analysis. GR is the project leader and head of the department. All authors read and corrected the draft version of this manuscript, and approved the final version.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study has been approved by the Medical Ethics Committee of the Erasmus MC, University Medical Center Rotterdam.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1: Figure S1.
Schedule of enrollment, interventions, and assessments. (DOC 54 kb)
Additional file 2:
SPIRIT 2013 Checklist: recommended items to address in a clinical trial protocol and related documents. (DOC 121 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Spielmann, K., van de Sandt-Koenderman, W.M.E., Heijenbrok-Kal, M.H. et al. Transcranial direct current stimulation in post-stroke sub-acute aphasia: study protocol for a randomized controlled trial. Trials 17, 380 (2016). https://doi.org/10.1186/s13063-016-1505-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-016-1505-z