Expanded abstract
Citation
ProCESS Investigators, Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, Terndrup T, Wang HE, Hou PC, LoVecchio F, Filbin MR, Shapiro NI, Angus DC. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014; 370:1683–93.
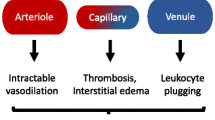
Background
In a single-center study published more than a decade ago involving patients presenting to the emergency department with severe sepsis and septic shock, mortality was markedly lower among those who were treated according to a 6-h protocol of early goal-directed therapy (EGDT), in which intravenous fluids, vasopressors, inotropes, and blood transfusions were adjusted to reach central hemodynamic targets including central venous pressure, central venous oxygen saturation, and indirect estimates of cardiac output, than among those receiving usual care.
Methods
Objective: The objective was to determine whether these EGDT findings were generalizable and whether all aspects of the EGDT protocol were necessary to achieve those outcomes.
Design: A multicenter randomized three-arm controlled trial.
Setting: Thirty-one academic emergency departments in the United States.
Subjects: Patients older than 18 years of age presenting to the emergency department with septic shock.
Intervention: Patients were assigned to one of three groups for 6 h of resuscitation: protocol-based EGDT as defined by River and colleagues; protocol-based standard therapy that did not require the placement of a central venous catheter, administration of inotropes, or blood transfusions; and usual care which mandated no specific monitoring or management approaches.
Outcomes: The primary end point was 60-day in-hospital mortality. Also tested sequentially was whether protocol-based care (EGDT and standard therapy groups combined) was superior to usual care and whether protocol-based EGDT was superior to protocol-based standard therapy. Secondary outcomes included longer-term mortality and the need for organ support.
Results
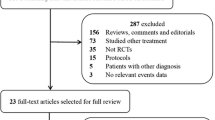
A total of 1,351 patients were enrolled, of whom 1,341 were evaluable due to patient/family request: 439 were randomly assigned to protocol-based EGDT, 446 to protocol-based standard therapy, and 456 to usual care. Resuscitation strategies differed significantly with respect to the monitoring of central venous pressure and central venous oxygen and the use of intravenous fluids, vasopressors, inotropes, and blood transfusions. By 60 days, there were 92 deaths in the protocol-based EGDT group (21.0 %), 81 in the protocol-based standard therapy group (18.2 %), and 86 in the usual care group (18.9 %) (relative risk with protocol-based therapy versus usual care, 1.04; 95 % confidence interval, 0.82 to 1.31; P = 0.83; relative risk with protocol-based EGDT versus protocol-based standard therapy, 1.15; 95 % CI, 0.88 to 1.51; P = 0.31). There were no significant differences in 90-day mortality, 1-year mortality, or the need for organ support.
Conclusions
In a multicenter trial conducted in the tertiary care setting, protocol-based resuscitation of patients in whom septic shock was diagnosed in the emergency department did not improve outcomes.
Similar content being viewed by others
Abbreviations
- CVC:
-
Central venous catheter
- EGDT:
-
Early goal-directed therapy
- ScvO2 :
-
Central venous oxygen saturation
References
Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013;41:1167–74.
Brun-Buisson C, Meshaka P, Pinton P, Vallet B, EPISEPSIS Study Group. EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004;30:580–8.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10.
Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–51.
Wang HE, Shapiro NI, Angus DC, Yealy DM. National estimates of severe sepsis in United States emergency departments. Crit Care Med. 2007;35:1928–36.
Kaukonen K, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA. 2014;311:1308–16.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Peake SL, Delaney A, Bailey M, Bellomo R, Cameron PA, Cooper DJ, et al. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014;371:1496–506.
Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015;372:1301–11.
Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303:739–46.
Acknowledgements
The work was the sole academic product of the authors without any external contributions review or input from members of the Department of Critical Care, University of Pittsburgh involved in the ProCESS trial.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
University of Pittsburgh Department of Critical Care Medicine: Evidence-Based Medicine Journal Club, edited by Sachin Yende
Rights and permissions
About this article
Cite this article
Cabrera, J.L., Pinsky, M.R. Management of septic shock: a protocol-less approach. Crit Care 19, 260 (2015). https://doi.org/10.1186/s13054-015-0968-8
Published:
DOI: https://doi.org/10.1186/s13054-015-0968-8