Abstract
Central venous oxygen saturation (ScvO2) >70% or mixed venous oxygen saturation (SvO2) >65% is recommended for both septic and non-septic patients. Although it is the task of experts to suggest clear and simple guidelines, there is a risk of reducing critical care to these simple recommendations. This article reviews the basic physiological and pathological features as well as the metrological issues that provide clear evidence that SvO2 and ScvO2 are adaptative variables with large inter-patient variability. This variability is exemplified in a modeled population of 1,000 standard ICU patients and in a real population of 100 patients including 15,860 measurements. In these populations, it can be seen how optimizing one to three of the four S(c)vO2 components homogenized the patients and yields a clear dependency with the fourth one. This explains the discordant results observed in large studies where cardiac output was increased up to predetermined S(c)vO2 thresholds following arterial oxygen hemoglobin saturation, total body oxygen consumption needs and hemoglobin optimization. Although a systematic S(c)vO2 goal-oriented protocol can be statistically profitable before ICU admission, appropriate intensive care mandates determination of the best compromise between S(c)vO2 and its four components, taking into account the specific constraints of each individual patient.
Similar content being viewed by others
Introduction
A recent review of the literature concluded that `central venous oxygen saturation (ScvO2) is a very important measurement, which can be easily taken in a critical care environment by both medical and nursing staff. It provides an understanding of the patient's oxygen delivery, oxygen consumption and cardiac output. It has a key role within early goal-directed Cdecrease mortality when taken and analyzed appropriately' [1]. Indeed, ScvO2 > 70% or mixed venous oxygen saturation (SvO2) >65% is recommended for both septic and non-septic patients [2]-[4].
There is no debate that a major task of experts is to determine clear and simple rules for the early treatment of life-threatening disorders. As a consequence of the worldwide promotion of these recommendations, however, there is a risk of reducing intensive care to these simple protocols. The objective of this review is to highlight the basic physiological and pathological features as well as the metrological issues that provide clear evidence that, in reality, and for each specific patient, SvO2 and ScvO2 are complex dynamic variables that may not always provide an appropriate cutoff for all clinical settings [5]-[7]. This may explain that targeting unique S(c)vO2 thresholds may balance positive and negative effects and may produce hazardous results in large studies.
The fundamental equilibrium
The sine qua non condition for adequate energy supply is that the circulatory system transports to each cell enough oxygen (O2), nutrients, and chemicals to ensure their aerobic respiration [8],[9]. `Adequate' means that, at any time, the difference (gap) between the expected metabolic needs minus the real O2 consumption (VO2) must not exceed energy storage. This basic equilibrium can be conveniently formulated as:
For any cell, tissue, and organ, VO2 is the difference between arterial and venous O2 flows. For the whole body, if we ignore the O2 dissolved in the plasma water, which represents only a few percent of the total O2 blood content, if we consider that arterial and venous blood flows are represented by the cardiac output (CO), and if we assume that arterial and venous blood flow have a similar hemoglobin concentration (Hb), then we can write:
where VO2 is in ml/minute.m2, CO is in L/minute.m2, Hb is in g/L, and arterial oxygen hemoglobin saturation (SaO2) and SvO2 are the ratios of arterial and venous oxygenated Hb over the total Hb per blood unit and, therefore, dimensionless percentages. The constant 1.34 is the carrying capacity of the oxygenated Hb in milliliters of O2 per gram. This equation can be reformulated as a function of each variable, but its reformulation as a function of SvO2 is one of the most popular because SvO2 measurements are precise, accurate, time responsive and quite easy to monitor [10],[11]. Figure 1 shows that the relationships between SvO2 and its components are not equivalent and not necessarily linear. As a consequence, a large change in one variable may be compensated by a small change in another - for example, small changes in low CO that are compensated for by large changes in SvO2 and large changes in high CO that are compensated for by small changes in SvO2:
Relationships between mixed venous oxygen hemoglobin saturation and its components. To create these curves, we modeled a standard ICU population of 1,000 patients (Excel, Microsoft) with normal distribution of arterial oxygen hemoglobin saturation (SaO2; 0.95 ± 0.05 limited to 1) and normal distributions of total body oxygen consumption (VO2) needs (140 ± 30 ml/minute.m2), cardiac output (CO; 3.0 ± 0.5 L/minute.m2) and hemoglobin concentration (Hb; 100 ± 15 g/L). Only one of the four components was sequentially changed (Y-variables) to look at its specific relationship with mixed venous oxygen saturation (SvO2) (X-variable). When unchanged, variables were set to their mean value. The horizontal arrows indicate the fluctuations of the Y-variable around its mean value (±2 standard deviations). The vertical arrows show the corresponding fluctuations of SvO2. We can see that reference ranges (mean ±2SD) of SaO2, VO2 needs, CO, and Hb are compensated for by a 26%, 50%, 47%, and 40% change in SvO2, respectively. Thus, CO is not necessarily the predominant component of SvO2 except when low (left, flat part of the relationship).
If we replace the measured value of VO2 by its two hidden components seen in [1], we find:
The purpose of the circulatory system, eventually supported by intensive care, is to nullify the VO2 gap; at equilibrium, therefore, Equation 4 can be written:
where eSvO2 is the expected SvO2 to maintain the equilibrium.
In reality, the `two hands of equality' in Equation 5 fluctuate around the equilibrium. When SvO2 is superior to the right hand, a VO2 gap is created, and when below, the gap is restored. If we subtract Equation 5 from Equation 4, we can see that the difference SvO2 - eSvO2 (ΔSvO2) is related to the VO2 gap:
Physiological adaptation
Any change in metabolic needs triggers active neuro-hormonal regulation to enable the actual VO2 to equalize to the VO2 needs as soon as possible. Under basal metabolic conditions, VO2 needs depend mostly on age, gender, height and weight [12]-[14]. In the resting state, physiological changes in the basal metabolism are mostly due to digestion and body temperature. A normal meal usually increases the metabolic rate by 4 to 10% and each degree change in temperature over or under 37°C alters VO2 needs by 13% [8]. Consequently, the expected VO2 of resting patients may be easily computed or found from normative tables.
This VO2 adaptation to metabolic needs is primarily achieved by stimulus-induced catecholamine secretion modulating global CO and its distribution. SaO2 is maintained close to 1 by the ventilation drive triggered by brain receptors. When low, Hb is also improved, albeit slowly, by iron mobilization, [15] kidney secretion of erythropoietin, [16] and the release of young red blood cells [17],[18]. In contrast, no regulatory loop has been observed for maintaining the mixed venous oxygen partial pressure or SvO2 within specific ranges. Therefore, SvO2 seems to be a variable that passively follows the regulation of its components. For any change in VO2 needs, the tissue residual partial pressure of O2 represents the final adjustment between O2 delivery and uptake and determines the change in SvO2. The proportional contributions of CO and SvO2 to the changes in VO2 strongly depend on body position, blood volume, and the protocol for increasing the requirements. In the following, we will assume that in ICU patients, lying supine, with acceptable blood volume, two-thirds of the change in VO2 is achieved by a parallel change in CO and one-third by an anti-parallel change in SvO2[19]-[23]. This allows us to derive the expected adaptive values of SvO2 as a function of age, gender and temperature (Figure 2). The two-thirds to one-third balance, observed in cases of physiologic stress, should be seen as a pivotal value in critical situations. In case of limited CO for any reasons, necessary compensation would be reached by a proportional decrease in SvO2 and vice versa.
Mixed venous oxygen hemoglobin saturation adaptation to fluctuations of related variables. Mixed venous oxygen saturation (SvO2) changes were modeled in 1,000 patients using JMP (SAS Institute, Cary, North Carolina, USA). In both panels, we used a random uniform distribution of age (range 20 to 90 years) and temperature (range 34 to 41°C) and the normative tables as modeled by the Hemodyn software® [7],[26]-[29]. This generates a wide range of total body oxygen consumption (VO2) needs (70 to 290 ml/minute.m2) and their corresponding cardiac output values (2.28 to 4.22 L/minute.m2) from which individual values of needed SvO2 can be inferred from Equation 2 according to different values of hemoglobin concentration and arterial oxygen hemoglobin saturation. In the left-hand panel, only old and hyperthermic patients have an expected physiological SvO2 < 0.65. In the right-hand panel, most patients have an expected SvO2 < 0.65 in response to a combined mild decrease in SaO2 and hemoglobin concentration. These examples have been created assuming no VO2 gap. In case of hypoxia, SvO2 values exceed the modeled value, proportionally to the VO2 gap following Equation 6.
The adaptive physiological variability of SvO2 that maintains VO2 equal to needs can also be shown by its frequency distribution in large populations of steady-state patients (Figure 3). We can see that the expected SvO2 is often below 65% in both modeled and real anesthetized patients. In real, non-anesthetized patients, other physiological contributors to metabolic needs, such as digestion, pain, discomfort, stress, inflammation, increased work of breathing, and so on, additionally increase this heterogeneity.
Frequency distribution of mixed venous oxygen hemoglobin saturation in two populations of patients. Left: a modeled population of 1,000 patients (JMP, SAS Institute, Cary, North Carolina, USA) as seen in Figure 2 but mimicking a standard ICU population by computing random gender, normal distribution of age (60 ± 12 years), temperature (37.5 ± 1.2°C), hemoglobin concentration (100 ± 15 g/L) and semi-normal distribution of arterial oxygen hemoglobin saturation (1 to 0.05) and assuming no total body oxygen consumption (VO2) gap. Right: a real population of post-cardiosurgery unshocked steady state patients (assuming no VO2 gap) with a wide range of changes in mixed venous oxygen saturation (SvO2) components (15,860 measurements obtained from a previously published study) [64].
Pathological changes
When the VO2 gap exceeds the tissue O2 reserve, the cell moves from aerobic to anaerobic metabolism, leading to tissue hypoxia and dysoxia [24],[25]. This can be first observed when the right-hand side of Equation 5 is excessively low (low SaO2, high VO2 needs, low CO or low Hb), such that SvO2 cannot decrease proportionally to maintain the equilibrium and a difference occurs between limited SvO2 and very low eSvO2.
A second pathological situation is observed in the case of impaired tissue O2 convection between hemoglobin and mitochondria, such that the arterial blood flow is not sufficiently unloaded and SvO2 increases over eSvO2. This can be seen when the O2 gradient is low due to a deficit in utilization (for example, from mitochondrial blockage, cyanide poisoning, and so on) and/or when O2 tissue diffusion is impaired by an excessive distance or a reduced surface area (for example, in the presence of edema, inflammation, microclots, reduced capillary density, anatomical and/or functional shunts). In septic shock or in late stage shock caused by any mechanism, SvO2 cannot decrease sufficiently due to a combination of these elementary mechanisms [7],[26]-[29].
In both situations, the parallel changes in SvO2, CO and Hb predicted by Equation 3 may be lost since VO2 is expected to increase as well up to its needed value.
Except in experimental conditions, these two pathological situations are usually combined [30]. We can reasonably speculate that, depending on the initial mechanisms of shock, its magnitude, and the adaptive possibilities of each patient, SvO2 will cover a wide range of values and will not provide by itself clear indications for guiding therapy. The same considerations will also lead to significant discordance between different studies according to the heterogeneity of their populations for each of the elementary mechanisms described above [31].
Metrological considerations
The reference method for assessing SvO2 requires mixed venous blood sampling through a pulmonary artery catheter and direct measurement of hemoglobin saturation using a multi-wavelength spectrophotometer (co-oximeter) [32]. When the blood sampling procedure is correct and the sample is immediately analyzed using a properly calibrated co-oximeter, the SvO2 measurement is accurate (bias <0.5%), precise (2 standard deviations (SD)/mean =1.3%) and linear (R2 = 1) [33],[34]. Even with such good performance indices, however, the least significant change in a unique measurement (2√2 ± 2SD/mean) is 3.7%, meaning that a SvO2 value of 65% needs to change to >68.7% or <61.3% to have a 95% chance of being real.
Continuous monitoring of SvO2 using a fiber-optic sensor placed at the tip of a pulmonary catheter has acceptable accuracy (bias <1%) when properly calibrated and recalibrated using a co-oximeter [35]. The precision is necessarily lower (2SD/mean >5%) [10],[11], but is compensated by a very fast response (almost instantaneous) [36], allowing averaging of several elementary measurements (N) in a few milliseconds and decreasing the standard error of the mean (2SD/√N). Averaging 10 elementary measurements when continuously monitoring SvO2 allows the same least significant changes to be achieved as when analyzing a unique mixed venous blood sample.
At the turn of the century, it was suggested that ScvO2 should be used as a surrogate of SvO2, owing to the fact that it is easier and less invasive to insert a central line than a pulmonary catheter. ScvO2 is similar to SvO2 in normal patients, being about 2 to 3% lower because many of the vascular circuits that drain into the inferior vena cava may have non-oxidative phosphorylation (renal, portal, hepatic blood flows) and therefore extract less O2[37],[38]. However, several studies have shown that ScvO2 may not predict SvO2 in patients suffering shock, depending on the O2 flows and O2 extractions of the different tissue compartments, and where measurements are taken [39]-[43]. The coefficient of variation (2SD/mean) between ScvO2 and SvO2 may exceed ±20% [44],[45]. Even paired changes in ScvO2 and SvO2 are not necessarily parallel; they were only found in 55% of cases in one study [45]. It is only when considering trend lines that changes in ScvO2 and SvO2 become more consistent [46].
Clinical evidence
Finally, there is a huge body of evidence (often with a degree of mathematical evidence) that SvO2 values vary widely in ICU patients, either for physiological, pathological or metrological reasons. Therefore, the appropriate SvO2 for achieving an adequate body energy supply is specific to each individual patient and to its specific time-evolving situation. There is no basic evidence for targeting any clear-cut SvO2 value. From the considerations listed above, it seems more appropriate to tune a multivariate compromise represented by an acceptable range of the four SvO2 component trend lines with the objective of fulfilling global and local metabolic needs. This compromise must be assessed in terms of predicted benefit and risk of any change.
A variety of clinical evidence has provided us with a message in accordance with these fundamentals, showing no interest in targeting specific values of SvO2 and/or ScvO2 in large populations of patients [47]-[49]. However, other studies have presented indisputable evidence that targeting a specific value of SvO2/ScvO2 can be of interest for lactate clearance [50], morbidity [51], and mortality [52]. Accordingly, the Surviving Sepsis Campaign recommends maximizing mixed or central venous oxygen saturation [2]. The contradiction is apparent. As previously mentioned and detailed above, all results can be predicted by the homogeneity/heterogeneity of the patient population.
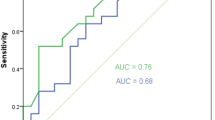
In the Rivers and colleagues' study [52], which is the main reference for the hemodynamic recommendations of the Surviving Sepsis Campaign, the population was homogenized as much as possible before targeting the ScvO2. The study included early septic shock before ICU admission, and thus compared patients at the same phase of pathological evolution. In addition, the therapeutic protocol, including sedation, mechanical ventilation and fraction of inspired oxygen adjustment, resulted in a decrease in VO2 needs and the maximization of SaO2. Hemoglobin was also increased when necessary by blood transfusion. Heart rate and central venous pressure were optimized, thus improving CO as much as possible. Under these conditions, if a low ScvO2 was found instead of an expected high value, even taking into consideration a possible discordance between ScvO2 and SvO2, the probability of insufficient CO was high and use of inotropes was consistent with the basic physiology. This is illustrated in Figure 4, where we used the same populations as shown in Figure 3 but with the distributions of the SvO2 components mimicking those of the study by Rivers and colleagues. In these homogenized populations, the SvO2 distribution is obviously narrower. If Hb, SaO2 and VO2 are homogenized, ScvO2 and/or SvO2 are necessarily more influenced by CO.
Frequency distribution of mixed venous oxygen hemoglobin saturation in two populations of `optimized' patients according to the protocol of Rivers and colleagues [[52]]. The left-hand panel represents the population of 1,000 patients as seen in Figure 3 but total body oxygen consumption needs and cardiac output (CO) were set at 120% and 130% of the expected values at basal metabolism for modeling septic conditions. Other variables were distributed as reported by Rivers and colleagues: age =67 ± 17.4 years, 50.8% male sex ratio, temperature =35.9 ± 3.2°C, hemoglobin concentration (Hb) >100 ± 15 g/L and arterial oxygen hemoglobin saturation (SaO2) >0.93. The right-hand panel represents the same real population of post-cardiosurgery patients as shown in Figure 3 but restricted to CO >1.3 basal values, Hb >100 ± 15 g/L and SaO2 > 0.93 (8,067 measurements). SvO2, mixed venous oxygen saturation.
From the modeled population seen in Figure 4, we can simulate the increase in CO required to reach a target SvO2 of >65% (presumably equivalent to ScvO2 > 70%). Such an increase would be required in 39.5% of the patients, up to 1.2 L/minute.m−2 (average 0.17 ± 0.16), which seems to be a reasonable objective.
However, the Surviving Sepsis Campaign recommended a target Hb of 70 to 90 g/L whereas in Rivers and colleagues' study the hematocrit was increased up to 30%, which represents an Hb >100 g/L. This has major consequences for SvO2. If we consider again the population modeled in Figure 4, reducing Hb from 100 to 90 g/L displaces the frequency distribution leftwards and it would be more difficult to target SvO2 to >65%. The simulation shows that an increase in CO would be necessary for 79.5% of the patients, up to 1.7 L/minute.m2, with an average increase of 0.39 ± 0.24. If targeting Hb to 70 g/L, an increase in CO would be necessary for 98.7% of the patients, up to 2.7 L/minute.m2 with a mean increase of 1.30 ± 0.44. All these estimations are derived with constant VO2 needs, ignoring the caloric effects of increasing CO [53]. Therefore, targeting the same SvO2 objective as Rivers and colleagues without targeting the same Hb has strong consequences for CO stimulation. Finally, SvO2 must be viewed as a compromise. Increasing Hb may have favorable [54] or detrimental effects [55]. Increasing CO may also have positive [56],[57] or negative results [58]-[61]. The final decision depends, therefore, on the specific conditions and limitations of each patient. This statement is reinforced by two recent reports. In the study of Jones and colleagues [62] management to increase lactate clearance was equivalent to targeting specific ScvO2 values in septic shock. Moreover, the ProCESS trial has shown that, in academic hospitals, the Rivers and colleagues' protocol was not superior to usual care despite significant increases in blood transfusion, dobutamine and vasopressor use [63]. The comparable mortality may only be explained by an absence of impact on mortality of these interventions, which seems unlikely, or by the fact that targeting a unique ScvO2 value in heterogeneous patients may balance positive and negative effects. Whether a unique SvO2 or ScvO2 goal would be beneficial or not depends, therefore, on the quality of care in the control group and on the inter-individual dispersion of the difference between the target and the optimal ScvO2 value allowing VO2 needs to be met. We have seen that this optimal value may be far from a fixed target. These results should not discourage us from monitoring SvO2 or ScvO2 but encourage us to include these variables in a multimodal analysis.
Conclusion
Basic physiology tells us that SvO2 is not a regulated variable but an adaptive variable depending on four elementary regulated components: VO2 needs, SaO2, Hb and CO. Consequently, SvO2 is widely fluctuating. There is no physiological argument for targeting particular values of SvO2 (or its surrogate ScvO2) by specific interventions except in homogenized populations, where optimizing one to three of the four SvO2 components may yield a clear dependency with the fourth one. This explains the apparently contradictory results observed in large studies where CO was increased up to specific SvO2 thresholds and confirms the basic physiology predicting large inter-patient variability. Although a systematic SvO2 goal-oriented protocol can be statistically profitable before ICU admission, one would expect from any trained intensivist a more sophisticated, multivariate approach and a determination of the best compromise between SvO2 and its components, taking into account the specific constraints of each individual patient.
Abbreviations
- CO:
-
Cardiac output
- eSvO2:
-
Expected SvO2
- Hb:
-
Hemoglobin concentration
- SaO2:
-
Arterial oxygen hemoglobin saturation
- ScvO2:
-
Central venous oxygen saturation
- SD:
-
Standard deviation
- SvO2:
-
Mixed venous oxygen saturation
- VO2:
-
Total body oxygen consumption
References
Reid M: Central venous oxygen saturation: analysis, clinical use and effects on mortality. Nurs Crit Care. 2013, 18: 245-250. 10.1111/nicc.12028.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R: Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013, 41: 580-637. 10.1097/CCM.0b013e31827e83af.
Carl M, Alms A, Braun J, Dongas A, Erb J, Goetz A, Göpfert M, Gogarten W, Grosse J, Heller A, Heringlake M, Kastrup M, Kröner A, Loer S, Marggraf G, Markewitz A, Reuter M, Schmitt DV, Schirmer U, Wiesenack C, Zwissler B, Spies C: Guidelines for intensive care in cardiac surgery patients: haemodynamic monitoring and cardio-circulatory treatment guidelines of the German Society for Thoracic and Cardiovascular Surgery and the German Society of Anaesthesiology and Intensive Care Medicine. Thorac Cardiovasc Surg. 2007, 55: 130-148. 10.1055/s-2007-964939.
Nieminen MS, Böhm M, Cowie MR, Drexler H, Filippatos GS, Jondeau G, Hasin Y, Lopez-Sendon J, Mebazaa A, Metra M, Rhodes A, Swedberg K, Priori SG, Garcia MA, Blanc JJ, Budaj A, Cowie MR, Dean V, Deckers J, Burgos EF, Lekakis J, Lindahl B, Mazzotta G, Morais J, Oto A, Smiseth OA, Garcia MA, Dickstein K, Albuquerque A, Conthe P, et al: Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology. Eur Heart J. 2005, 26: 384-416. 10.1093/eurheartj/ehi044.
Perel A: Bench-to-bedside review: the initial hemodynamic resuscitation of the septic patient according to Surviving Sepsis Campaign guidelines - does one size fit all?. Crit Care. 2008, 12: 223-10.1186/cc6979.
Bellomo R, Reade MC, Warrillow SJ: The pursuit of a high central venous oxygen saturation in sepsis: growing concerns. Crit Care. 2008, 12: 130-10.1186/cc6841.
Teboul JL, Hamzaoui O, Monnet X: SvO2 to monitor resuscitation of septic patients: let's just understand the basic physiology. Crit Care. 2011, 15: 1005-10.1186/cc10491.
Guyton A: Energetics and metabolic rate. Guyton and Hall Textbook of Medical Physiology. 2011, Saunders, Philadelpia, PA, 829-
Squara P: Matching total body oxygen consumption and delivery: a crucial objective?. Intensive Care Med. 2004, 30: 2170-2179. 10.1007/s00134-004-2449-4.
Bongard F, Lee TS, Leighton T, Liu SY: Simultaneous in vivo comparison of two-versus three-wavelength mixed venous (Svo2) oximetry catheters. J Clin Monit. 1995, 11: 329-334. 10.1007/BF01616992.
Armaganidis A, Dhainaut JF, Billard JL, Klouche K, Mira JP, Brunet F, Dinh-Xuan AT, Dall'Ava-Santucci J: Accuracy assessment for three fiberoptic pulmonary artery catheters for SvO2 monitoring. Intensive Care Med. 1994, 20: 484-488. 10.1007/BF01711900.
Harris JA, Benedict FG: A biometric study of human basal metabolism. Proc Natl Acad Sci U S A. 1918, 4: 370-373. 10.1073/pnas.4.12.370.
Roza AM, Shizgal HM: The Harris Benedict equation reevaluated: resting energy requirements and the body cell mass. Am J Clin Nutr. 1984, 40: 168-182.
Black AE, Coward WA, Cole TJ, Prentice AM: Human energy expenditure in affluent societies: an analysis of 574 doubly-labelled water measurements. Eur J Clin Nutr. 1996, 50: 72-92.
Meital V, Izak G, Rachmilewitz M: Changes in iron mobilization and utilization induced by acute haemorrhage. Br J Haematol. 1966, 12: 598-610. 10.1111/j.1365-2141.1966.tb00143.x.
Gleiter CH, Freudenthaler S, Delabar U, Eckardt KU, Muhlbauer B, Gundert-Remy U, Osswald H: Erythropoietin production in healthy volunteers subjected to controlled haemorrhage: evidence against a major role for adenosine. Br J Clin Pharmacol. 1996, 42: 729-735. 10.1046/j.1365-2125.1996.00484.x.
Robertson OH, Bock AV: Blood volume in wounded soldiers. 1. Blood volume and related blood changes after hemorrhage. J Exp Med. 1919, 29: 139-153. 10.1084/jem.29.2.139.
Gleiter CH, Becker T, Schreeb KH, Freudenthaler S, Gundert-Remy U: Fenoterol but not dobutamine increases erythropoietin production in humans. Clin Pharmacol Ther. 1997, 61: 669-676. 10.1016/S0009-9236(97)90102-8.
Guyton A, Jones C, Coleman T: Circulatory Physiology: Cardiac Output and Its Regulation. 1963, WB Saunders, Philadelphia
Martin WH, Montgomery J, Snell PG, Corbett JR, Sokolov JJ, Buckey JC, Maloney DA, Blomqvist CG: Cardiovascular adaptations to intense swim training in sedentary middle-aged men and women. Circulation. 1987, 75: 323-330. 10.1161/01.CIR.75.2.323.
De Cort SC, Innes JA, Barstow TJ, Guz A: Cardiac output, oxygen consumption and arteriovenous oxygen difference following a sudden rise in exercise level in humans. J Physiol. 1991, 441: 501-512.
Ridout SJ, Parker BA, Smithmyer SL, Gonzales JU, Beck KC, Proctor DN: Age and sex influence the balance between maximal cardiac output and peripheral vascular reserve. J Appl Physiol (1985). 2010, 108: 483-489. 10.1152/japplphysiol.00985.2009.
Abudiab MM, Redfield MM, Melenovsky V, Olson TP, Kass DA, Johnson BD, Borlaug BA: Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur J Heart Fail. 2013, 15: 776-785. 10.1093/eurjhf/hft026.
Pinsky M: Beyond global oxygen supply-demand relations: in search of measures of dysoxia. Intensive Care Med. 1994, 20: 1-3. 10.1007/BF02425045.
Robin ED: Of men and mitochondria: coping with hypoxic dysoxia. Am Rev Resp Dis. 1980, 122: 517-531.
Squara P, Journois D, Formela F, Dhainaut J, Sollet JP, Bleichner G: Value of elementary, calculated and modeled hemodynamic variables. J Crit Care. 1994, 9: 223-235. 10.1016/0883-9441(94)90002-7.
Krafft P, Steltzer H, Hiesmayr M, Klimscha W, Hammerle AF: Mixed venous oxygen saturation in critically ill septic shock patients. The role of defined events. Chest. 1993, 103: 900-906. 10.1378/chest.103.3.900.
Van Beest PA, Hofstra JJ, Schultz MJ, Boerma EC, Spronk PE, Kuiper MA: The incidence of low venous oxygen saturation on admission to the intensive care unit: a multi-center observational study in The Netherlands. Crit Care. 2008, 12: R33-10.1186/cc6811.
Textoris J, Fouche L, Wiramus S, Antonini F, Tho S, Martin C, Leone M: High central venous oxygen saturation in the latter stages of septic shock is associated with increased mortality. Crit Care. 2011, 15: R176-10.1186/cc10325.
Velissaris D, Pierrakos C, Scolletta S, De Backer D, Vincent JL: High mixed venous oxygen saturation levels do not exclude fluid responsiveness in critically ill septic patients. Crit Care. 2011, 15: R177-10.1186/10326.
Deep A, Goonasekera CD, Wang Y, Brierley J: Evolution of haemodynamics and outcome of fluid-refractory septic shock in children. Intensive Care Med. 2013, 39: 1602-1609. 10.1007/s00134-013-3003-z.
Nierman DM, Schechter CB: Mixed venous O2 saturation: measured by co-oximetry versus calculated from PVO2. J Clin Monit. 1994, 10: 39-44. 10.1007/BF01651465.
Zwart A, Buursma A, van Kampen EJ, Zijlstra WG: Multicomponent analysis of hemoglobin derivatives with reversed-optics spectrophotometer. Clin Chem. 1984, 30: 373-379.
Bailey SR, Russell EL, Martinez A: Evaluation of the AVOXimeter: precision, long-term stability, linearity, and use without heparin. J Clin Monit. 1997, 13: 191-198. 10.1023/A:1007308616686.
Baele PL, McMichan JC, Marsh HM, Sill JC, Southorn PA: Continuous monitoring of mixed venous oxygen saturation in critically ill patients. Anesth Analg. 1982, 61: 513-517. 10.1213/00000539-198206000-00007.
Nakamura M, Homma A, Tatsumi E, Uesho K, Taenaka Y, Masuzawa T, Nakamura T, Zhang B, Kakuta Y, Imada K, Nakatani T, Takano H: Mixed venous oxygen saturation as a promising parameter for physiologic control of total artificial heart. Asaio J. 2000, 46: 761-766. 10.1097/00002480-200011000-00020.
Bloos F, Reinhart K: Venous oximetry. Intensive Care Med. 2005, 31: 911-913. 10.1007/s00134-005-2670-9.
Reinhart K, Kuhn HJ, Hartog C, Bredle DL: Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004, 30: 1572-1578. 10.1007/s00134-004-2337-y.
Chawla LS, Zia H, Gutierrez G, Katz NM, Seneff MG, Shah M: Lack of equivalence between central and mixed venous oxygen saturation. Chest. 2004, 126: 1891-1896. 10.1378/chest.126.6.1891.
Van Beest PA, van Ingen J, Boerma EC, Holman ND, Groen H, Koopmans M, Spronk PE, Kuiper MA: No agreement of mixed venous and central venous saturation in sepsis, independent of sepsis origin. Crit Care. 2010, 14: R219-10.1186/cc9348.
Ho KM, Harding R, Chamberlain J, Bulsara M: A comparison of central and mixed venous oxygen saturation in circulatory failure. J Cardiothorac Vasc Anesth. 2010, 24: 434-439. 10.1053/j.jvca.2007.10.011.
Dahmani S, Paugam-Burtz C, Gauss T, Alves M, Le Bihan E, Necib S, Belghiti J, Mantz J: Comparison of central and mixed venous saturation during liver transplantation in cirrhotic patients: a pilot study. Eur J Anaesthesiol. 2010, 27: 714-719.
Lequeux PY, Bouckaert Y, Sekkat H, Van der Linden P, Stefanidis C, Huynh CH, Bejjani G, Bredas P: Continuous mixed venous and central venous oxygen saturation in cardiac surgery with cardiopulmonary bypass. Eur J Anaesthesiol. 2010, 27: 295-299. 10.1097/EJA.0b013e3283315ad0.
Martin C, Auffray JP, Badetti C, Perrin G, Papazian L, Gouin F: Monitoring of central venous oxygen saturation versus mixed venous oxygen saturation in critically ill patients. Intensive Care Med. 1992, 18: 101-104. 10.1007/BF01705041.
Varpula M, Karlsson S, Ruokonen E, Pettila V: Mixed venous oxygen saturation cannot be estimated by central venous oxygen saturation in septic shock. Intensive Care Med. 2006, 32: 1336-1343. 10.1007/s00134-006-0270-y.
Dueck MH, Klimek M, Appenrodt S, Weigand C, Boerner U: Trends but not individual values of central venous oxygen saturation agree with mixed venous oxygen saturation during varying hemodynamic conditions. Anesthesiology. 2005, 103: 249-257. 10.1097/00000542-200508000-00007.
Gattinoni L, Brazzi L, Pelozzi P: A trial of goal-oriented hemodynamic therapy in critically ill patients. N Engl J Med. 1995, 333: 1025-1032. 10.1056/NEJM199510193331601.
Ziegler DW, Wright JG, Choban PS, Flancbaum L: A prospective randomized trial of preoperative `optimization' of cardiac function in patients undergoing elective peripheral vascular surgery. Surgery. 1997, 122: 584-592. 10.1016/S0039-6060(97)90132-X.
Seymour CW, Cooke CR, Mikkelsen ME, Hylton J, Rea TD, Goss CH, Gaieski DF, Band RA: Out-of-hospital fluid in severe sepsis: effect on early resuscitation in the emergency department. Prehosp Emerg Care. 2010, 14: 145-152. 10.3109/10903120903524997.
Leone M, Boyadjiev I, Boulos E, Antonini F, Visintini P, Albanese J, Martin C: A reappraisal of isoproterenol in goal-directed therapy of septic shock. Shock. 2006, 26: 353-357. 10.1097/01.shk.0000226345.55657.66.
Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J: A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000, 90: 1052-1059. 10.1097/00000539-200005000-00010.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001, 345: 1368-1377. 10.1056/NEJMoa010307.
De Backer D, Moraine JJ, Berre J, Kahn RJ, Vincent JL: Effects of dobutamine on oxygen consumption in septic patients. Direct versus indirect determinations. Am J Respir Crit Care Med. 1994, 150: 95-100. 10.1164/ajrccm.150.1.8025780.
Wu WC, Rathore SS, Wang Y, Radford MJ, Krumholz HM: Blood transfusion in elderly patients with acute myocardial infarction. N Engl J Med. 2001, 345: 1230-1236. 10.1056/NEJMoa010615.
Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santaló M, Muñiz E, Guarner C: Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013, 368: 11-21. 10.1056/NEJMoa1211801.
Yu M, Levy MM, Smith P, Takiguchi SA, Miyasaki A, Myers SA: Effect of maximizing oxygen delivery on morbidity and mortality rates in critically ill patients: a prospective, randomized, controlled study. Crit Care Med. 1993, 21: 830-838. 10.1097/00003246-199306000-00009.
Lobo SM, Lobo FR, Polachini CA, Patini DS, Yamamoto AE, de Oliveira NE, Serrano P, Sanches HS, Spegiorin MA, Queiroz MM, Christiano AC, Savieiro EF, Alvarez PA, Teixeira SP, Cunrath GS: Prospective, randomized trial comparing fluids and dobutamine optimization of oxygen delivery in high-risk surgical patients [ISRCTN42445141]. Crit Care. 2006, 10: R72-10.1186/cc4913.
Schreiber T, Hueter L, Gaser E, Schmidt B, Schwarzkopf K, Karzai W: Effects of a catecholamine-induced increase in cardiac output on lung injury after experimental unilateral pulmonary acid instillation. Crit Care Med. 2007, 35: 1741-1748. 10.1097/01.CCM.0000269374.85160.BF.
Challand C, Struthers R, Sneyd JR, Erasmus PD, Mellor N, Hosie KB, Minto G: Randomized controlled trial of intraoperative goal-directed fluid therapy in aerobically fit and unfit patients having major colorectal surgery. Br J Anaesth. 2012, 108: 53-62. 10.1093/bja/aer273.
Drakos SG, Kfoury AG, Gilbert EM, Long JW, Stringham JC, Hammond EH, Jones KW, Bull DA, Hagan ME, Folsom JW, Horne BD, Renlund DG: Multivariate predictors of heart transplantation outcomes in the era of chronic mechanical circulatory support. Ann Thorac Surg. 2007, 83: 62-67. 10.1016/j.athoracsur.2006.07.050.
Hernandez G, Bruhn A, Luengo C, Regueira T, Kattan E, Fuentealba A, Florez J, Castro R, Aquevedo A, Pairumani R, McNab P, Ince C: Effects of dobutamine on systemic, regional and microcirculatory perfusion parameters in septic shock: a randomized, placebo-controlled, double-blind, crossover study. Intensive Care Med. 2013, 39: 1435-1443. 10.1007/s00134-013-2982-0.
Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA: Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010, 303: 739-746. 10.1001/jama.2010.158.
Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, Terndrup T, Wang HE, Hou PC, LoVecchio F, Filbin MR, Shapiro NI, Angus DC: A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014, 370: 1683-1693. 10.1056/NEJMoa1401602.
Squara P, Denjean D, Estagnasie P, Brusset A, Dib JC, Dubois C: Noninvasive cardiac output monitoring (NICOM): a clinical validation. Intensive Care Med. 2007, 33: 1191-1194. 10.1007/s00134-007-0640-0.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author declares that he has no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Squara, P. Central venous oxygenation: when physiology explains apparent discrepancies. Crit Care 18, 579 (2014). https://doi.org/10.1186/s13054-014-0579-9
Published:
DOI: https://doi.org/10.1186/s13054-014-0579-9