Abstract
Morbidly adherent placenta (MAP), which includes accreta, increta, and percreta, is a condition characterized by the invasion of the uterine wall by placental tissue. The condition is associated with higher odds of massive post-partum hemorrhage. Several interventions have been developed to improve hemorrhage-related outcomes in these patients; however, there is no evidence to prefer any intervention over another. Resuscitative endovascular balloon occlusion of the aorta (REBOA) is an endovascular intervention that may be useful and effective to reduce hemorrhage and transfusions in MAP patients. The objective of this narrative review is to summarize the evidence for REBOA in patients with MAP. We posit that acute care surgeons can perform REBOA for patients with MAP.
Similar content being viewed by others
Background
Morbidly adherent placenta (MAP), which includes placenta accreta, increta, and percreta, is characterized by the abnormal invasion of the uterine wall by placental tissue [1]. MAP occurs in 1 per 333 to 533 deliveries and is a leading cause of post-partum hemorrhage (PPH) and maternal mortality worldwide [2, 3]. MAP may manifest at the moment of delivery when the invasive placenta does not readily detach from the uterus, precipitating potentially life-threatening PPH [1, 3].
The optimal management strategy for patients with MAP has been the subject of considerable debate [3,4,5]. Although several interventions have proven useful and effective for the management of abnormal placentation-associated PPH [1, 3, 6], early identification of patients at risk for catastrophic hemorrhage and aggressive multidisciplinary management is key for improving outcomes [4, 7]. Recent evidence suggests that resuscitative endovascular balloon occlusion of the aorta (REBOA) is a safe and effective intervention to improve hemorrhage-related outcomes in patients with MAP [8,9,10,11]. Acute care surgeons have increasing experience in performing REBOA in trauma patients and are optimally suited to, as part of a multidisciplinary team, perform REBOA in women with MAP undergoing either planned or emergent cesarean delivery.
Given the preventable nature of death from PPH, the active participation of acute care surgeons in providing the endovascular (REBOA) care to patients with MAP and at risk of massive hemorrhage could be a cornerstone of effective maternal mortality reduction worldwide, especially in low- to middle-income countries where 99% of all world PPH-related deaths occur [12].
The objective of this narrative review is to summarize the evidence for REBOA in patients with MAP. We posit that acute care surgeons can perform REBOA for women with MAP.
Morbidly adherent placenta
MAP is the global term encompassing the constellation of conditions resulting from varying levels of abnormal implantation of the placenta: placenta accreta, increta, and percreta. Placenta accreta occurs when the placenta becomes abnormally adherent to the uterine wall. Placenta increta is characterized by further invasion of the abnormal placental tissue into the myometrium. Placenta percreta results when the placenta penetrates the uterine serosa or surrounding tissues [1].
There are well-described risk factors for the development of MAP [1, 3]. The most common and relevant is previous cesarean delivery. Risk for MAP increases with each additional C-section as additional scar tissue develops [13]. The increasing incidence of MAP over the last 60 years has been attributed to increasing C-section rates. Recent estimates are that MAP occurs in 1 in every 300 to 500 pregnancies [2]. MAP thus accounts for a significant proportion of maternal morbidity and mortality cases as it carries a higher risk of catastrophic post-partum hemorrhage, especially in cases of placenta percreta with its deeper penetration [1,2,3, 14,15,16].
The primary peril with MAP occurs at the moment of delivery when the abnormally implanted placenta can result in major hemorrhage. Ninety percent of these patients will require transfusion of blood products, and at least 50% will receive a massive transfusion [3, 16, 17]. Despite prenatal surgical planning and perioperative resuscitation, maternal death may still occur in some cases [2, 3, 15].
The current recommendation for the surgical management of MAP at the moment of delivery is to perform a cesarean hysterectomy with the placenta left in situ [3, 5, 18]. Endovascular adjuvant strategies (i.e., prophylactic occlusion balloon catheters in both internal iliac arteries, uterine artery embolization) [19, 20] may be used to prevent and treat bleeding during cesarean hysterectomy. Although these interventions can prove life-saving, a considerable proportion of patients with MAP still end up requiring massive transfusion and post-op obstetrical critical care support. Furthermore, there is no evidence from randomized clinical trials to prefer any surgical intervention over another. Therefore, there is an urgent need for innovation and development of effective strategies to achieve expeditious hemorrhage arrest and prevent the occurrence of massive life-threatening bleeding.
Resuscitative endovascular balloon occlusion of the aorta in patients with MAP
REBOA is a minimally invasive procedure that introduces a balloon occlusion catheter via a percutaneous groin puncture or cutdown of the femoral artery into the aorta to obtain endovascular aortic occlusion [21, 22]. The physiologic rationale behind the use of REBOA is that it provides proximal control of bleeding and causes volume redistribution from the lower to the proximal vascular beds. These phenomena are hypothesized to ensure an adequate circulating volume and avoid the collapse of systemic circulation.
The use of REBOA in patients with MAP is not new: in 1995, a multidisciplinary team prophylactically deployed an aortic occlusion catheter in a patient with placenta percreta at 34 weeks’ gestation undergoing a planned cesarean delivery. Neither massive transfusion nor admission to the intensive care unit was required, and the patient was discharged 1 week after C-section without any complications [23]. Since that initial case report, additional single cases [24, 25] and uncontrolled case series [10, 26, 27] of MAP patients undergoing C-section combined with temporary aortic balloon occlusion were published. In these reports, REBOA was used either as a rescue maneuver to stop the bleeding during an emergency peripartum hysterectomy [10, 24, 25] or as a prophylactic hemodynamic adjunct in elective cases [26, 27].
Data from retrospective comparative studies suggest that, compared to traditional planned cesarean delivery, planned C-section with the use of REBOA results in better maternal hemorrhage-related outcomes [8, 28,29,30]. Cui et al. [28] found that intraoperative blood loss was lower in women with placenta previa that underwent planned C-section plus REBOA, compared with patients that underwent C-section alone. These results were consistent with other studies [29, 30] which found that MAP patients benefited from REBOA in terms of average blood loss and transfusions. Moreover, a recent meta-analysis of observational data added additional validation to the finding that the prophylactic use of REBOA during elective C-section results in lower overall blood loss and fewer transfusions [9]. Thus, it seems reasonable to deploy REBOA in emergency and appropriate elective situations in patients with MAP [9].
Despite promising evidence of the potential effectiveness of REBOA in MAP [8, 9], this approach has not been routinely adopted likely due to the required involvement, time, and effort from multidisciplinary teams, including interventional radiologists or trained acute care surgeons, and because of the technical dexterity required.
REBOA deployed by acute care surgeons in pregnant women with MAP: is this feasible?
Within the field of trauma and emergency surgery, acute care surgeons have typically used REBOA in victims of traumatic truncal hemorrhage who present with hemodynamic instability [31,32,33]. Trauma surgeons are critical care providers and surgical rescuers [34]; hence, their role in REBOA applicable clinical scenarios has been limited only to those unstable patients who require urgent life-saving surgical interventions. There are, however, other clinical scenarios (i.e., elective care of abnormal placentation) where REBOA has proven feasible, safe, and effective [9], where acute care surgeons could play an active and integral role in the multidisciplinary care of pregnant women affected by MAP [9].
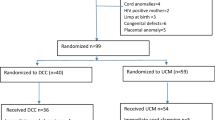
To date, three reports have shown that trauma and acute care surgeons can safely deploy a REBOA in pregnant women with MAP (Table 1) [9, 11, 35]. In these reports, pregnant women with MAP underwent a cesarean delivery with intraoperative REBOA deployment with the goal of either arresting ongoing bleeding [11] or preventing the onset of major hemorrhage [9, 35]. The REBOAs were deployed by acute care surgeons in hybrid suites or conventional operating rooms. No REBOA-related complications were reported, and all patients survived to discharge. Although these reports are case studies without a comparison group, they provide a glimpse into the potential benefits of REBOA in decreasing hemorrhage-related complications by having acute care surgeons be in charge of delivering the endovascular intervention. For example, our group [9] has previously described a case series of 12 pregnant women with a prenatal diagnosis of MAP scheduled for elective cesarean delivery with a multidisciplinary team in which a trauma surgeon was in charge of inserting, deploying, and removing the REBOA (Table 1). In this study, all patients survived, none required either massive transfusion or post-op obstetrical critical care, and no complications relating to REBOA use were noted. This compares with studies of MAP patients which found that they, on average, have blood loss of 3 to 5 l and a significant proportion require massive transfusion [3].
Traditionally, MAP patients have received endovascular care from interventional radiologists. Interventional radiologists are trained to deploy endovascular balloon occlusion catheters in the iliac arteries [19] or the aorta [8] and to perform selective arterial embolization when required. Although interventional radiologists’ input in the multidisciplinary care of MAP patients has been remarkable, their participation and skill set demand the availability of modern interventional radiology suites. This infrastructure requirement is available in few well-equipped centers and is scarce in low- and middle-income countries, where PPH continues to be a leading cause of maternal death. In contrast, well-trained and qualified trauma and acute care surgeons can safely deploy a REBOA in a conventional operating room setting [9, 11]. Therefore, acute care surgeons with endovascular training and skills can be consulted either to rescue a pregnant patient who is dying in the operating room due to massive bleeding or to prophylactically deploy and inflate a REBOA in patients undergoing a planned C-section.
With the advent of smaller diameter catheters, REBOA may become more accessible for use in low-resource settings where neither interventional radiology suites nor blood supplies are available. In these scenarios, trauma surgeons with the ability to monitor all stages of REBOA technique may play a crucial role during the multidisciplinary surgical management of patients with MAP by providing the endovascular care which, in turn, could improve morbidity and mortality in these patients.
The REBOA procedure: how we do it
Previous research has established that the multidisciplinary team management of pregnant women with MAP is associated with a lower likelihood of prolonged maternal admission to the intensive care unit, less large-volume blood transfusion, decreased coagulopathy, fewer ureteral injuries, and less risk for early reoperation [7]. Therefore, in our institution, a multidisciplinary team composed of an obstetrician with training in critical care obstetrics, a urologist, an anesthesiologist, and a trauma and acute care surgeon manages the care of pregnant women with MAP.
With the goal of delivering appropriate care, a defined protocol for planned cesarean hysterectomy with simultaneous REBOA deployment has been established in our institution.
Pregnant women referred to our center with suspicion of MAP are initially evaluated by the obstetrician who makes a diagnosis based on findings from the ultrasonography and the MRI. If prenatal diagnosis of MAP is made, then the patient is scheduled for a planned cesarean delivery. At the time of C-section, the patients are taken to a conventional operating room equipped with a mobile C-arm and an ultrasound machine.
Regarding anesthesia, most centers would place an epidural catheter or use a combined spinal–epidural technique. Although neuraxial anesthesia would allow anesthesia for painless insertion of the REBOA, general anesthesia may be a better option for patients who are predicted to become hemodynamically unstable and require massive resuscitation [36].
After the induction of anesthesia and tracheal intubation, the assisting urologist inserts bilateral ureteral stents with cystoscopic guidance, and the acute care surgeon obtains endovascular access via the common femoral artery for REBOA deployment. Arterial access is obtained via the right groin under ultrasound guidance. The common femoral artery is punctured, and a guidewire is inserted and secured. A sheath (7 Fr) is then passed over the guidewire into the lumen. Finally, the guidewire is withdrawn leaving the introducer sheath in place through which 7 Fr catheter REBOA can be introduced. The depth of REBOA advancement is determined by external landmarks, and C-arm fluoroscopy confirms correct positioning (aortic zone III). With REBOA in place and deflated, the obstetric team starts the cesarean hysterectomy.
The preferred abdominal entry technique is via midline vertical incision, and the hysterotomy is made away from the placenta. After fetal delivery and umbilical cord clamping, the placenta is left in place and the hysterotomy closed using a continuous suture, and a typical cesarean hysterectomy is performed. REBOA can be inflated either at the moment of umbilical cord clamping or when the obstetrician starts dissecting the most vascularized area [9]. We prefer, however, to inflate the REBOA immediately after umbilical cord clamping to provide a less bloody surgical field which in turn may accelerate the hysterectomy. With hysterectomy completed, the REBOA is deflated and removed along with the sheath with manual digital pressure applied to the groin puncture site for hemostasis.
There is currently no standard of care guideline regarding the appropriate care of pregnant women in the REBOA post-catheterization period. However, we recommend close monitoring for at least the first 24 h post-procedure. Examinations should be done every 15 min in the first 2 h post-REBOA and then every hour in the following 6 h. The surgeon in charge should examine the access site and assess extremity color, temperature, and pulses and must be aware of swelling and pain at the vascular access site, as well as of weak or absent distal pulses. Close monitoring during the first hours post-catheterization with the active participation of the bedside nurse is paramount for early identification and management of complications post-REBOA.
The role of acute care surgeons in MAP surgical protocols: beyond surgical rescue
Acute care surgeons can successfully be integrated into a multidisciplinary team responsible for the elective surgical care of otherwise healthy patients. Traditionally, acute care surgeons have been responsible for patients requiring emergency surgical care. However, with the growth of specific surgical fields, the scope of acute care surgeons has been reduced to simple surgical procedures. For example, Pottenger et al. [37] showed that among the ten procedures that trauma surgeons performed most frequently per year, seven could be performed at the bedside. It is clear that the field of acute care surgery requires expansion of horizons to survive the predominant model of excessive surgical specialization. In that sense, our proposal complements the five pillars of acute care surgery described by Pietzman and colleagues [34] as acute care surgeons can be consulted to rescue pregnant women with ongoing PPH or to provide elective endovascular care to patients at risk of catastrophic PPH.
Conclusion
REBOA is a feasible and safe surgical intervention that has proven effective in reducing the volume of blood loss and transfusions in pregnant women with morbidly adherent placenta undergoing cesarean delivery. This intervention can be safely delivered by acute care surgeons with endovascular training and experience in a conventional operating room. As PPH secondary to MAP continues to be a leading cause of maternal morbidity and mortality, we believe that our protocol could reduce the burden of mortality attributable to MAP worldwide.
Abbreviations
- MAP:
-
Morbidly adherent placenta
- PPH:
-
Post-partum hemorrhage
- REBOA:
-
Resuscitative endovascular balloon occlusion of the aorta
References
Bauer ST, Bonanno C. Abnormal placentation. Semin Perinatol. 2009;33:88–96.
Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol. 2005;192:1458–61.
Committee opinion no. 529: placenta accreta. Obstet Gynecol. 2012;120:207–11.
Silver RM, Fox KA, Barton JR, Abuhamad AZ, Simhan H, Huls CK, et al. Center of excellence for placenta accreta. Am J Obstet Gynecol. 2015;212:561–8.
AG E, TF P, Soisson P, RM S. Optimal management strategies for placenta accreta. BJOG An Int J Obstet Gynaecol. 2009;116:648–54.
Dahlke JD, Mendez-Figueroa H, Maggio L, Hauspurg AK, Sperling JD, Chauhan SP, et al. Prevention and management of postpartum hemorrhage: a comparison of 4 national guidelines. Am J Obstet Gynecol. 2018;213:76 e1–76.e10.
Eller AG, Bennett MA, Sharshiner M, Masheter C, Soisson AP, Dodson M, et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet Gynecol. 2011;117:331–7.
Manzano-Nunez R, Escobar-Vidarte MF, Naranjo MP, Rodriguez F, Ferrada P, Casallas JD, et al. Expanding the field of acute care surgery: a systematic review of the use of resuscitative endovascular balloon occlusion of the aorta (REBOA) in cases of morbidly adherent placenta. Eur J Trauma Emerg Surg. 2018;44:519–26.
Ordoñez CA, Manzano-Nunez R, Parra MW, Rasmussen TE, Nieto AJ, Herrera-Escobar JP, et al. Prophylactic use of resuscitative endovascular balloon occlusion of the aorta in women with abnormal placentation: a systematic review, meta-analysis and case series. J Trauma Acute Care Surg. 2018;84:809–18.
Stensaeth KH, Sovik E, Haig INY, Skomedal E, Jorgensen A. Fluoroscopy-free resuscitative endovascular balloon occlusion of the aorta (REBOA) for controlling life threatening postpartum hemorrhage. PLoS One. 2017;12:e0174520.
Parra MW, Ordonez CA, Herrera-Escobar JP, Gonzalez-Garcia A, Guben J. Resuscitative endovascular balloon occlusion of the aorta for placenta percreta/previa. J Trauma Acute Care Surg. 2018;82:403–5.
Haeri S, Dildy GA. Maternal mortality from hemorrhage. Semin Perinatol. 2012;36:48–55.
Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107:1226–32.
Eshkoli T, Weintraub AY, Sergienko R, Sheiner E. Placenta accreta: risk factors, perinatal outcomes, and consequences for subsequent births. Am J Obstet Gynecol. 2013;208:219.e1–7.
Hudon L, Belfort MA, Broome DR. Diagnosis and management of placenta percreta: a review. Obstet Gynecol Surv. 1999;54:509–17.
Brookfield KF, Goodnough LT, Lyell DJ, Butwick AJ. Perioperative and transfusion outcomes in women undergoing cesarean hysterectomy for abnormal placentation. Transfusion. 2014;54:1530–6.
Stotler B, Padmanabhan A, Devine P, Wright J, Spitalnik SL, Schwartz J. Transfusion requirements in obstetric patients with placenta accreta. Transfusion. 2011;51:2627–33.
Warshak CR, Ramos GA, Eskander R, Benirschke K, Saenz CC, Kelly TF, et al. Effect of predelivery diagnosis in 99 consecutive cases of placenta accreta. Obstet Gynecol. 2010;115:65–9.
Shrivastava V, Nageotte M, Major C, Haydon M, Wing D. Case-control comparison of cesarean hysterectomy with and without prophylactic placement of intravascular balloon catheters for placenta accreta. Am J Obstet Gynecol. 2007;197:1–5.
Gonsalves M, Belli A. The role of interventional radiology in obstetric hemorrhage. Cardiovasc Intervent Radiol. 2010;33:887–95.
Biffl WL, Fox CJ, Moore EE. The role of REBOA in the control of exsanguinating torso hemorrhage. J Trauma Acute Care Surg. 2015;78:1054–8.
Ordoñez CA, Manzano-Nunez R, del Valle AM, Rodriguez F, Burbano P, Naranjo MP, et al. Current use of resuscitative endovascular balloon occlusion of the aorta (REBOA) in trauma. Colomb J Anesthesiol. 2017;45:30–8.
Paull JD, Smith J, Williams L, Davison G, Devine T, Holt M. Balloon occlusion of the abdominal aorta during caesarean hysterectomy for placenta percreta. Anaesth Intensive Care. 1995;23:731–4.
Usman N, Noblet J, Low D, Thangaratinam S. Intra-aortic balloon occlusion without fluoroscopy for severe postpartum haemorrhage secondary to placenta percreta. Int J Obstet Anesth. 2014;23:91–3.
Bell-Thomas SM, Penketh RJ, Lord RH, Davies NJ, Collis R. Emergency use of a transfemoral aortic occlusion catheter to control massive haemorrhage at caesarean hysterectomy. BJOG An Int J Obstet Gynaecol. 2003;110:1120–2.
Duan X-H, Wang Y-L, Han X-W, Chen Z-M, Chu Q-J, Wang L, et al. Caesarean section combined with temporary aortic balloon occlusion followed by uterine artery embolisation for the management of placenta accreta. Clin Radiol. 2015;70:932–7.
Wei X, Zhang J, Chu Q, Du Y, Xing N, Xu X, et al. Prophylactic abdominal aorta balloon occlusion during caesarean section: a retrospective case series. Int J Obstet Anaesth. 2016;27:10–5.
Cui S, Zhi Y, Cheng G, Zhang K, Zhang L, Shen L. Retrospective analysis of placenta previa with abnormal placentation with and without prophylactic use of abdominal aorta balloon occlusion. Int J Gynecol Obstet. 2017;137:265–70.
Wu Q, Liu Z, Zhao X, Liu C, Wang Y, Chu Q, et al. Outcome of pregnancies after balloon occlusion of the infrarenal abdominal aorta during caesarean in 230 patients with placenta praevia accreta. Cardiovasc Intervent Radiol. 2016;39:1573–9.
Xie L, Wang Y, Luo F-Y, Man Y-C, Zhao X-L. Prophylactic use of an infrarenal abdominal aorta balloon catheter in pregnancies complicated by placenta accreta. J Obstet Gynaecol (Lahore). 2017;37:557–61.
Morrison JJ, Galgon RE, Jansen JO, Cannon JW, Rasmussen TE, Eliason JL, et al. A systematic review of the use of resuscitative endovascular balloon occlusion of the aorta in the management of hemorrhagic shock. J Trauma Acute Care Surg. 2016;80:324–34.
Joseph JD, Thomas MS, Megan B, Dimitra S, Kenji I, Jeremy C, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg. 2016;81:409–19.
Ordoñez CA, Parra MW, Manzano-Nunez R, Herrera-Escobar JP, Serna JJ, Rodriguez-Ossa P, et al. Intra-operative combination of resuscitative endovascular balloon occlusion of the aorta and a median sternotomy in hemodynamically unstable patients’ with penetrating chest trauma: is this feasible? J Trauma Acute Care Surg. 2018;84:752–7.
Kutcher ME, Sperry JL, Rosengart MR, Mohan D, Hoffman MK, Neal MD, et al. Surgical rescue: the next pillar of acute care surgery. J Trauma Acute Care Surg. 2017;82:280–6.
Russo RM, Girda E, Kennedy V, Humphries MD. Two lives, one REBOA: hemorrhage control for urgent cesarean hysterectomy in a Jehovah’s Witness with placenta percreta. J Trauma Acute Care Surg. 2017;83:551–3.
Lilker S, Meyer R, Downey K, Macarthur A. Anesthetic considerations for placenta accreta. Int J Obstet Anesth. 2011;20:288–92.
Pottenger BC, Galante JM, Wisner DH. The modern acute care surgeon: characterization of an evolving surgical niche. J Trauma Acute Care Surg. 2015;78:120–5.
Acknowledgements
RMN, JPH, and CPO would like to express their gratitude to Dr. Carlos A. Ordoñez who not only have been a fantastic mentor but also taught them how to mentor other people. All the authors want to thank Dr. Fernando Rosso from the Clinical Research Center at La Fundacion Valle del Lili Hospital for his constant support.
Author information
Authors and Affiliations
Contributions
Only authors who made substantive intellectual contributions were listed as authors. RMN, CPO, JPHE, SMG, JJM, AJN, NP, JCM, MFE, and CAO contributed equally to this work. CAO and RMN conceived the idea. CPO, JJM, and RMN performed the literature search. All authors wrote the report, made critical revisions to the manuscript, and approved the final version for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Manzano-Nunez, R., Escobar-Vidarte, M.F., Orlas, C.P. et al. Resuscitative endovascular balloon occlusion of the aorta deployed by acute care surgeons in patients with morbidly adherent placenta: a feasible solution for two lives in peril. World J Emerg Surg 13, 44 (2018). https://doi.org/10.1186/s13017-018-0205-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-018-0205-2