Abstract
Background
The aim of the present analysis was to evaluate the recurrence pattern in patients with recurrent malignant glioma after re-irradiation in combination with bevacizumab as there is limited data on how to optimally choose dose, fractionation and delineation margins.
Methods
Thirty-one patients with recurrent malignant glioma treated with re-irradiation and bevacizumab after previous chemoradiotherapy (concurrent temozolomide 75 mg/m2/d according to the EORTC/NCIC trial) and [18 F]FET-PET and/or MRI confirmed recurrence were retrospectively analyzed. Bevacizumab was applied twice during fractionated re-irradiation (10 mg/kg, d1 + d15, median 36 Gy, conventionally fractionated). Recurrence patterns were assessed by means of [18 F]FET-PET and/or MRI.
Results
Median follow-up was 34.0 months for all patients [95%-CI, 27.7-40.3] and median post-recurrence survival 10.8 months [95%-CI, 9.2-12.4]. Concerning the recurrence patterns, 61.3% of these were located in-field (19 patients), 22.6% were marginal (7 patients) and 16.1% ex-field (5 patients). No influence on the recurrence pattern was observed according to sex, WHO grade, maintenance chemotherapy or MGMT methylation status whereas planning target volume (PTV) size had a significant influence on the recurrence pattern (p = 0.032). PTV sizes > 75 ml were associated with a higher in-field recurrence rate and lower median post-recurrence progression-free survival (8.5 vs. 4.9 months, p = 0.016).
Conclusions
After the administration of re-irradiation with bevacizumab the recurrence pattern seems to be mainly centrally located. The PTV size was the main predictor for a marginal/ex-field recurrence.
Similar content being viewed by others
Introduction
In patients with high-grade glioma (HGG) a high rate of local failures has been observed after multimodal therapy [1]. The addition of temozolomide (TMZ) increased local control and survival whereas the 2-year survival rate remained 27.2% [2].
In selected patients, a second course of radiotherapy (RT) might be a reasonable treatment option despite the relative lack of prospective randomized data [3]-[6]. Contrarily, conventional cytotoxic approaches were found to be not adequately effective [7]-[10] so molecularly targeted drugs either alone or in combination with cytotoxic agents are currently undergoing clinical testing.
Various groups have investigated the use of bevacizumab – a humanised monoclonal antibody against VEGF-A with an already established role in metastatic colon, breast, and lung cancer [11] – for patients with recurrent HGG [12] and several trials have documented its efficacy [13]-[17] which may be due to the presence of pronounced hypoxia as well as high levels of tumor driven angiogenesis in HGG [18].
Since the efficacy of radiation-based re-treatment is limited, it is reasonable to test how far the addition of a putative radiation response modulator would impact on the efficacy of re-treatment. In this regard, one group tested the sequential use of radiosurgery and bevacizumab with favorable outcome [19]. Alternatively, Gutin and co-workers determined the safety and efficacy of radiotherapy (RT) and concomitant bevacizumab – for the GBM cohort, progression-free survival at six months (PFS-6) was 65% [20]. In a previous retrospective study on 30 recurrent malignant glioma patients undergoing re-irradiation, 20 treated with bevacizumab and 10 without bevacizumab we showed that PFS-6 within the bevacizumab-treated cohort was 72% and survival was significantly enhanced [21]. With substantially longer follow-up and a higher patient number, the significant post-recurrence survival (PRS) benefit of bevacizumab could be confirmed within a second study describing a beneficial treatment with a low rate of side-effects [22]. Recent prospective phase III trials (AVAglio & RTOG 0825) were designed to prove the efficacy of TMZ based radio-chemotherapy with bevacizumab as first-line therapy but failed to show a survival benefit whereas significant and marginally significant progression-free survival benefits have been observed [23],[24].
In our study we retrospectively analyzed the pattern of re-recurrence in recurrent HGG patients undergoing re-irradiation with bevacizumab as there is limited data on how to choose proper safety margins during radiotherapy planning and furthermore, in how far the chosen fractionation schedule yielded adequate local control rates.
Material and Methods
Patient selection
Only patients with histologically and/or [18 F]FET-PET/MRI proven recurrence of high-grade gliomas (WHO grades III + IV) and macroscopic tumor (maximum diameter 6 cm, multifocality per se was not a contraindication) underwent re-irradiation, the interval between first radiotherapy and re-irradiation had to be 6 months at minimum. Another precondition was the absence of meaningful alternative treatment options, e. g. complete resection by re-surgery, interstitial brachytherapy or systemic chemotherapy.
Treatment schedule and follow-up
Before treatment, a gadolinium-enhanced brain MRI with gradient echo sequence and perfusion and/or a [18 F]FET-PET. Patients treated with bevacizumab received 10 mg/kg at days 1 and 15 during re-irradiation. If TMZ was applied concomitantly in patients who had no previous progression after TMZ pre-treatment a dosage of 75 mg/m2 daily was chosen.
Treatment outcome was evaluated on a regular basis (every three months) by brain MRI as described by [25] and/or [18 F]FET-PET.
Adjuvant chemotherapy was prescribed on an individual basis as no standard has been defined yet but was not defined as mandatory.
[18 F]FET-PET data acquisition and analysis
Dynamic PET scans were acquired on a Siemens ECAT EXACT HR+ scanner (Siemens/CTI, Knoxville, TN, USA) after intravenous injection of approximately 180 MBq [18 F]FET according to a standardized protocol [26]. Data were reconstructed by filtered back projection using a Hann filter, corrected for scatter and attenuation and afterwards transferred to a HERMES workstation (Hermes Medical Solutions, Sweden) for further data processing. PET-based evaluation of recurrence was performed by an experienced nuclear physician by assessment of the maximal standardized uptake value within the tumour corrected for the unspecific uptake in the background (SUVmax/BG > 1.6) in combination with a previously introduced dynamic analysis of [18 F]FET kinetic uptake behaviour [27]. Furthermore, the biological tumor volume was assessed, which was defined by semi-automatic threshold-based calculation of a volume of interest.
Radiotherapy
By analogy with Combs et al. [28] patients received a total dose of 36 Gy in 18 fractions (2 Gy single doses) employing 3D conformal radiotherapy or intensity-modulated radiotherapy (IMRT) if adjacent critical structures were present. Planning target volume (PTV) was defined as gross tumor volume (GTV) plus 10 mm margin at maximum. GTV included the contrast enhancing lesion in T1w + Gd MRI. To ensure reproducibility patients were immobilized with a thermoplastic mask system. Treatment planning was performed using the Oncentra® treatment planning system (OTP MasterPlan®, Elekta, Crawley, UK).
Analysis of recurrence pattern
Recurrences were defined as “in-field” if more than 80% of the tumour recurrence resided within the prescription 95% isodose surface, and “marginal” if 20% to 80% of the lesion was inside the 95% isodose surface. In all other cases, recurrences were defined as outside the radiation field (“ex-field”) according to the study of Lee et al. [29]; in case of a multifocal recurrence, the part lying most distant to the initial tumour site was taken as reference.
Statistics
Tumour progression was defined according RANO criteria [30] or by the appearance of new vital/progressive tumour lesions by means of dynamic [18 F]FET-PET. Post-recurrence progression-free (PR-PFS) and post-recurrence survival (PRS), measured from the beginning of re-irradiation to progression or death, respectively, or date of last follow-up, were analyzed using the Kaplan-Meier method; 95% CIs were calculated using the associated estimated standard errors. The log-rank test was used to test the significance of the following prognostic variables: MGMT promoter methylation status, age, surgery and pattern of disease recurrence. In view of their small number, patients with recurrence at RT margin were grouped with patients having an ex-field recurrence in the analysis of time to progression. A logistic regression analysis was performed to determine variables with significant influence on the recurrence pattern. Proportions were compared using Fisher’s exact test. A p-value ≤ 0.05 was considered significant.
The scientific use of retrospective data has been explicitly allowed by Bavarian federal law. Additionally, all patients agreed that their scientific data could be used. No experimental research on humans or animals has been performed or reported. The declaration of Helsinki has been obeyed in all points.
Results
Thirty-one patients with recurrent HGG were included into this retrospective analysis and treated at the Department of Radiation Oncology, University Hospital of Munich from 8/2008 until 7/2012, median age was 51 years (range, 18 – 67 years) and 74.2% of the patients were younger than 60 years.
Median radiotherapy dose was 36 Gy in 2 Gy single fractions and two applications of bevacizumab had been applied concomitantly.
MGMT methylation status was not available in 2 cases (6.5%), 11 of the remaining 29 patients were MGMT methylated (35.5%), for other patient characteristics see Table 1.
Median follow-up was 34.0 months for all patients [95%-CI, 27.7 - 40.3], median post-recurrence survival was 10.8 months [95%-CI, 9.2 - 12.4].
Concerning the recurrence patterns of the 31 patients, 61.3% of these were located in-field (19 patients), 22.6% were marginal (7 patients) and 16.1% ex-field (5 patients).
In view of the small numbers, we summarized both patients with marginal and ex-field recurrences as these were patients where a 10 mm PTV margin was probably too narrow (38.7%). Thus, marginal and ex-field recurrences were grouped and subsequent analyses were based on this precondition.
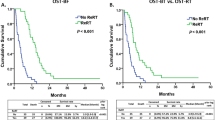
Concerning PRS and PR-PFS, no significant univariate factors could be obtained with an influence on latter endpoints including KPS, sex, age, WHO grade at relapse, MGMT methylation status, PTV size (continuous variable) or recurrence patterns.
Therefore, we further analyzed which factors would influence the pattern of recurrence.
Univariate testing was performed employing the same factors without the KPS - all could be identified to be non-significant except the PTV size with a hazard ratio of 0.986 (p = 0.032), see Table 2.
We performed an ROC analysis to determine the optimal threshold of the PTV to stratify between in-field and marginal/ex-field recurrences and determined 75 ml as optimal size (which is equal to the 25th quartile of all PTV sizes).
Fisher’s exact test showed a trend for a correlation between recurrence pattern and PTV size (as binary variable with 75 ml as threshold); 5 recurrences were marginal/ex-field compared to 2 in-field recurrences for PTV sizes smaller than 75 ml whereas larger PTV sizes were associated with a high in-field recurrence rate, 17 in-field vs. 7 ex-field recurrences (p = 0.078). This constructed binary variable showed a trend in predicting the type of recurrence (hazard ratio 0.17, p = 0.058).
Finally, we compared the PFS rates in both PTV size groups and obtained a significant difference (8.5 vs. 4.9 months, p = 0.016) which is shown in Figure 1. PRS was not significantly different in both groups (11.3 vs. 10.1 months, p = 0.276).
Discussion
For certain subgroups of recurrent high-grade glioma patients re-irradiation may be a strategy to prolong survival with acceptable toxicity. The aim of this study was to analyze the re-recurrence pattern after re-irradiation keeping in mind that this is the largest cohort to our knowledge uniformly treated with re-irradiation and bevacizumab in one center.
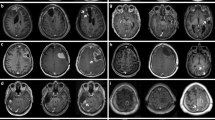
A mainstay in treatment follow-up is a reliable imaging modality: Whereas conventional magnetic-resonance-imaging (MRI) provides information on the size and localization of the tumor and delineates secondary phenomena such as haemorrhage, oedema, and mass effect, positron emission tomography (PET) with diverse radiolabelled compounds has been proposed to characterize the tumour on a metabolic and molecular level [31]. In particular, different radiolabelled amino acids like [11C]Methionine ([11C]MET) [32] as well as aromatic amino acid analogues like [18 F]Fluoroethyltyrosine ([18 F]FET) [33] were previously proposed to provide valuable additional information in patients with glioma [34],[35].
MRI was regularly performed as follow-up imaging - [18 F]FET-PET imaging was routinely performed (67.7%) or in case of a questionable progression (according to MRI), as it was proposed to reliably distinguish between post-therapeutic benign lesions and tumour recurrence after treatment of low- and high-grade gliomas [36],[37].
To our knowledge, the only group having also determined the recurrence pattern after re-irradiation with bevacizumab were Shapiro et al. [38] who derived 50% central recurrences. Their treatment strategy was built on a very tight margin with 5 mm to the contrast-enhancing lesion including 5 fractions with 6 Gy single doses, two fractions per week.
From our observation, 2/36 Gy is locally active in combination with bevacizumab, but recurrences mainly seem to be central which leaves us to speculate that a dose escalation could be warranted - especially due to the radioprotective potential of bevacizumab [39]. Other groups have tested 36 Gy in 2 Gy single fractions with adequate to very moderate activity, recent and several ongoing studies include rather higher single doses (2.4 Gy, 3 Gy, 3.5 Gy).
For smaller lesions, marginal and ex-field recurrences are more often observed which could generate the hypothesis that larger lesions display an increased radioresistant behavior, potentially due to hypoxic conditions and a larger number of tumor stem cells. These findings might lead to an adaption of planning margins according to the size of the lesion, e. g. with a central simultaneous boost technique in large tumor volumes which might be justified by the altogether dismal prognosis of this patient group. As target delineation is mainly based on contrast-enhanced MRI, the relatively higher rate of ex-field recurrences in smaller lesions could be explained by a tumor miss due to small margins (whereas 10 mm are at the higher end of the literature).
The discussion about the tumor size itself as prognostic parameter has not been resolved - despite its relevance on the recurrence pattern, there was no significant influence on survival - even the prognostic score defined by Combs et al. did not include the size itself as parameter but could itself not be validated in smaller cohorts up to now [40]-[42].
Other recurrence analyses in the primary setting have determined a relation with molecular genetics [1],[43] which could not be confirmed in the recurrence setting. Furthermore, no increase in distant failures could be observed such as in smaller series of primary glioblastoma patients after concurrent radiotherapy, bevacizumab and temozolomide [44]. Conversely, the low rate of in-field recurrences was not reproducible due to dose limitations during re-irradiation.
All in all, after the administration of re-irradiation with bevacizumab recurrences seem to be mainly centrally located. The PTV size was the main predictor for a marginal/ex-field recurrence. It would be valuable to have future studies evaluating the role of dose escalation to the central part of the tumor, e. g. as a stereotactic dose escalation or by means of a simultaneous integrated boost (SIB) as shown for many other sites [45]-[47].
References
Niyazi M, Schnell O, Suchorska B, Schwarz SB, Ganswindt U, Geisler J, Bartenstein P, Kreth FW, Tonn JC, Eigenbrod S, Belka C, la Fougere C: FET-PET assessed recurrence pattern after radio-chemotherapy in newly diagnosed patients with glioblastoma is influenced by MGMT methylation status. Radiother Oncol 2012, 104: 78-82. 10.1016/j.radonc.2012.04.022
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K, Hau P, Brandes AA, Gijtenbeek J, Marosi C, Vecht CJ, Mokhtari K, Wesseling P, Villa S, Eisenhauer E, Gorlia T, Weller M, Lacombe D, Cairncross JG, Mirimanoff RO: Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 2009, 10: 459-466. 10.1016/S1470-2045(09)70025-7
Henke G, Paulsen F, Steinbach JP, Ganswindt U, Isijanov H, Kortmann RD, Bamberg M, Belka C: Hypofractionated reirradiation for recurrent malignant glioma. Strahlenther Onkol 2009, 185: 113-119. 10.1007/s00066-009-1969-9
Vordermark D, Kolbl O, Ruprecht K, Vince GH, Bratengeier K, Flentje M: Hypofractionated stereotactic re-irradiation: treatment option in recurrent malignant glioma. BMC Cancer 2005, 5: 55. 10.1186/1471-2407-5-55
Niyazi M, Siefert A, Schwarz SB, Ganswindt U, Kreth FW, Tonn JC, Belka C: Therapeutic options for recurrent malignant glioma. Radiother Oncol 2010, 98: 1-14. 10.1016/j.radonc.2010.11.006
Niyazi M, Karin I, Sohn M, Nachbichler SB, Lang P, Belka C, Ganswindt U: Analysis of equivalent uniform dose (EUD) and conventional radiation treatment parameters after primary and re-irradiation of malignant glioma. Radiat Oncol 2013, 8: 287. 10.1186/1748-717X-8-287
Kappelle AC, Postma TJ, Taphoorn MJ, Groeneveld GJ, van den Bent MJ, van Groeningen CJ, Zonnenberg BA, Sneeuw KC, Heimans JJ: PCV chemotherapy for recurrent glioblastoma multiforme. Neurology 2001, 56: 118-120. 10.1212/WNL.56.1.118
Franceschi E, Cavallo G, Scopece L, Paioli A, Pession A, Magrini E, Conforti R, Palmerini E, Bartolini S, Rimondini S, Esposti RD, Crino L: Phase II trial of carboplatin and etoposide for patients with recurrent high-grade glioma. Br J Cancer 2004, 91: 1038-1044.
Pipas JM, Meyer LP, Rhodes CH, Cromwell LD, McDonnell CE, Kingman LS, Rigas JR, Fadul CE: A Phase II trial of paclitaxel and topotecan with filgrastim in patients with recurrent or refractory glioblastoma multiforme or anaplastic astrocytoma. J Neurooncol 2005, 71: 301-305. 10.1007/s11060-004-2026-2
Niyazi M, Siefert A, Schwarz SB, Ganswindt U, Kreth FW, Tonn JC, Belka C: Therapeutic options for recurrent malignant glioma. Radiother Oncol 2011, 98: 1-14. 10.1016/j.radonc.2010.11.006
Jenab-Wolcott J, Giantonio BJ: Bevacizumab: current indications and future development for management of solid tumors. Expert Opin Biol Ther 2009, 9: 507-517. 10.1517/14712590902817817
Beal K, Abrey LE, Gutin PH: Antiangiogenic agents in the treatment of recurrent or newly diagnosed glioblastoma: analysis of single-agent and combined modality approaches. Radiat Oncol 2011, 6: 2. 10.1186/1748-717X-6-2
Desjardins A, Vredenburgh JJ, Gururangan S, Peters KB, Friedman AH, Friedman H, Reardon DA: A PHASE II STUDY OF BEVACIZUMAB PLUS ETOPOSIDE AMONG RECURRENT MALIGNANT GLIOMA PATIENTS. Neuro Oncol 2009, 11: 633-633.
Desjardins A, Reardon DA, Coan A, Marcello J, Herndon JE 2nd, Bailey L, Peters KB, Friedman HS, Vredenburgh JJ: Bevacizumab and daily temozolomide for recurrent glioblastoma. Cancer 2011, 118: 1302-1312. 10.1002/cncr.26381
Reardon DA, Desjardins A, Peters K, Gururangan S, Sampson J, Rich JN, McLendon R, Herndon JE 2nd, Marcello J, Threatt S, Friedman AH, Vredenburgh JJ, Friedman HS: Phase II study of metronomic chemotherapy with bevacizumab for recurrent glioblastoma after progression on bevacizumab therapy. J Neurooncol 2011, 103: 371-379. 10.1007/s11060-010-0403-6
Reardon DA, Desjardins A, Peters KB, Gururangan S, Sampson JH, McLendon RE, Herndon JE 2nd, Bulusu A, Threatt S, Friedman AH, Vredenburgh JJ, Friedman HS: Phase II study of carboplatin, irinotecan, and bevacizumab for bevacizumab naive, recurrent glioblastoma. J Neurooncol 2012, 107: 155-164. 10.1007/s11060-011-0722-2
Vredenburgh JJ, Desjardins A, Herndon JE 2nd, Marcello J, Reardon DA, Quinn JA, Rich JN, Sathornsumetee S, Gururangan S, Sampson J, Wagner M, Bailey L, Bigner DD, Friedman AH, Friedman HS: Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol 2007, 25: 4722-4729. 10.1200/JCO.2007.12.2440
Jain RK, Di Tomaso E, Duda DG, Loeffler JS, Sorensen AG, Batchelor TT: Angiogenesis in brain tumours. Nat Rev Neurosci 2007, 8: 610-622. 10.1038/nrn2175
Cuneo KC, Vredenburgh JJ, Sampson JH, Reardon DA, Desjardins A, Peters KB, Friedman HS, Willett CG, Kirkpatrick JP: Safety and efficacy of stereotactic radiosurgery and adjuvant bevacizumab in patients with recurrent malignant gliomas. Int J Radiat Oncol Biol Phys 2011, 82: 2018-2024. 10.1016/j.ijrobp.2010.12.074
Gutin PH, Iwamoto FM, Beal K, Mohile NA, Karimi S, Hou BL, Lymberis S, Yamada Y, Chang J, Abrey LE: Safety and efficacy of bevacizumab with hypofractionated stereotactic irradiation for recurrent malignant gliomas. Int J Radiat Oncol Biol Phys 2009, 75: 156-163. 10.1016/j.ijrobp.2008.10.043
Niyazi M, Ganswindt U, Schwarz SB, Kreth FW, Tonn JC, Geisler J, la Fougere C, Ertl L, Linn J, Siefert A, Belka C: Irradiation and bevacizumab in high-grade glioma retreatment settings. Int J Radiat Oncol Biol Phys 2012, 82: 67-76. 10.1016/j.ijrobp.2010.09.002
Flieger M, Ganswindt U, Schwarz SB, Kreth FW, Tonn JC, la Fougere C, Ertl L, Linn J, Herrlinger U, Belka C, Niyazi M: Re-irradiation and bevacizumab in recurrent high-grade glioma: an effective treatment option. J Neurooncol 2014, 117: 337-345. 10.1007/s11060-014-1394-5
Chinot OL, de La Motte RT, Moore N, Zeaiter A, Das A, Phillips H, Modrusan Z, Cloughesy T: AVAglio: Phase 3 trial of bevacizumab plus temozolomide and radiotherapy in newly diagnosed glioblastoma multiforme. Adv Ther 2011, 28: 334-340. 10.1007/s12325-011-0007-3
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M, Jeraj R, Brown PD, Jaeckle KA, Schiff D, Stieber VW, Brachman DG, Werner-Wasik M, Tremont-Lukats IW, Sulman EP, Aldape KD, Curran WJ Jr, Mehta MP: A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 2014, 370: 699-708. 10.1056/NEJMoa1308573
Gallego Perez-Larraya J, Lahutte M, Petrirena G, Reyes-Botero G, Gonzalez-Aguilar A, Houillier C, Guillevin R, Sanson M, Hoang-Xuan K, Delattre JY: Response assessment in recurrent glioblastoma treated with irinotecan-bevacizumab: comparative analysis of the Macdonald, RECIST, RANO, and RECIST + F criteria. Neuro Oncol 2012, 14: 667-673. 10.1093/neuonc/nos070
Jansen NL, Suchorska B, Wenter V, Eigenbrod S, Schmid-Tannwald C, Zwergal A, Niyazi M, Drexler M, Bartenstein P, Schnell O, Tonn JC, Thon N, Kreth FW, la Fougere C: Dynamic 18 F-FET PET in newly diagnosed astrocytic low-grade glioma identifies high-risk patients. J Nucl Med 2014, 55: 198-203. 10.2967/jnumed.113.122333
Popperl G, Kreth FW, Herms J, Koch W, Mehrkens JH, Gildehaus FJ, Kretzschmar HA, Tonn JC, Tatsch K: Analysis of 18 F-FET PET for grading of recurrent gliomas: is evaluation of uptake kinetics superior to standard methods? J Nucl Med 2006, 47: 393-403.
Combs SE, Bischof M, Welzel T, Hof H, Oertel S, Debus J, Schulz-Ertner D: Radiochemotherapy with temozolomide as re-irradiation using high precision fractionated stereotactic radiotherapy (FSRT) in patients with recurrent gliomas. J Neurooncol 2008, 89: 205-210. 10.1007/s11060-008-9607-4
Lee SW, Fraass BA, Marsh LH, Herbort K, Gebarski SS, Martel MK, Radany EH, Lichter AS, Sandler HM: Patterns of failure following high-dose 3-D conformal radiotherapy for high-grade astrocytomas: a quantitative dosimetric study. Int J Radiat Oncol Biol Phys 1999, 43: 79-88. 10.1016/S0360-3016(98)00266-1
Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, Degroot J, Wick W, Gilbert MR, Lassman AB, Tsien C, Mikkelsen T, Wong ET, Chamberlain MC, Stupp R, Lamborn KR, Vogelbaum MA, van den Bent MJ, Chang SM: Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 2010, 28: 1963-1972. 10.1200/JCO.2009.26.3541
Gambhir SS: Molecular imaging of cancer with positron emission tomography. Nat Rev Cancer 2002, 2: 683-693. 10.1038/nrc882
Derlon JM, Bourdet C, Bustany P, Chatel M, Theron J, Darcel F, Syrota A: [11C]L-methionine uptake in gliomas. Neurosurgery 1989, 25: 720-728. 10.1227/00006123-198911000-00006
Wester HJ, Herz M, Weber W, Heiss P, Senekowitsch-Schmidtke R, Schwaiger M, Stocklin G: Synthesis and radiopharmacology of O-(2-[18 F]fluoroethyl)-L-tyrosine for tumor imaging. J Nucl Med 1999, 40: 205-212.
Niyazi M, Geisler J, Siefert A, Schwarz SB, Ganswindt U, Garny S, Schnell O, Suchorska B, Kreth FW, Tonn JC, Bartenstein P, la Fougere C, Belka C: FET-PET for malignant glioma treatment planning. Radiother Oncol 2011, 99: 44-48. 10.1016/j.radonc.2011.03.001
Niyazi M, Jansen N, Ganswindt U, Schwarz SB, Geisler J, Schnell O, Busing K, Eigenbrod S, la Fougere C, Belka C: Re-irradiation in recurrent malignant glioma: prognostic value of [18 F]FET-PET. J Neurooncol 2012, 110: 389-395. 10.1007/s11060-012-0980-7
Brandes AA, Tosoni A, Spagnolli F, Frezza G, Leonardi M, Calbucci F, Franceschi E: Disease progression or pseudoprogression after concomitant radiochemotherapy treatment: Pitfalls in neurooncology. Neuro Oncol 2008, 10: 361-367. 10.1215/15228517-2008-008
Jansen NL, Suchorska B, Schwarz SB, Eigenbrod S, Lutz J, Graute V, Bartenstein P, Belka C, Kreth FW, la Fougere C: [18 F]fluoroethyltyrosine-positron emission tomography-based therapy monitoring after stereotactic iodine-125 brachytherapy in patients with recurrent high-grade glioma. Mol Imaging 2013, 12: 137-147.
Shapiro LQ, Beal K, Goenka A, Karimi S, Iwamoto FM, Yamada Y, Zhang Z, Lassman AB, Abrey LE, Gutin PH: Patterns of failure after concurrent bevacizumab and hypofractionated stereotactic radiation therapy for recurrent high-grade glioma. Int J Radiat Oncol Biol Phys 2013, 85: 636-642. 10.1016/j.ijrobp.2012.05.031
Levin VA, Bidaut L, Hou P, Kumar AJ, Wefel JS, Bekele BN, Grewal J, Prabhu S, Loghin M, Gilbert MR, Jackson EF: Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. Int J Radiat Oncol Biol Phys 2011, 79: 1487-1495. 10.1016/j.ijrobp.2009.12.061
Scholtyssek F, Zwiener I, Schlamann A, Seidel C, Meixensberger J, Bauer M, Hoffmann KT, Combs SE, von Bueren AO, Kortmann RD, Muller K: Reirradiation in progressive high-grade gliomas: outcome, role of concurrent chemotherapy, prognostic factors and validation of a new prognostic score with an independent patient cohort. Radiat Oncol 2013, 8: 161. 10.1186/1748-717X-8-161
Combs SE, Edler L, Rausch R, Welzel T, Wick W, Debus J: Generation and validation of a prognostic score to predict outcome after re-irradiation of recurrent glioma. Acta Oncol 2013, 52: 147-152. 10.3109/0284186X.2012.692882
Niyazi M, Flieger M, Ganswindt U, Combs SE, Belka C: Validation of the prognostic Heidelberg re-irradiation score in an independent mono-institutional patient cohort. Radiat Oncol 2014, 9: 128. 10.1186/1748-717X-9-128
Brandes AA, Tosoni A, Franceschi E, Sotti G, Frezza G, Amista P, Morandi L, Spagnolli F, Ermani M: Recurrence pattern after temozolomide concomitant with and adjuvant to radiotherapy in newly diagnosed patients with glioblastoma: correlation With MGMT promoter methylation status. J Clin Oncol 2009, 27: 1275-1279. 10.1200/JCO.2008.19.4969
Shields LB, Kadner R, Vitaz TW, Spalding AC: Concurrent bevacizumab and temozolomide alter the patterns of failure in radiation treatment of glioblastoma multiforme. Radiat Oncol 2013, 8: 101. 10.1186/1748-717X-8-101
Hauswald H, Habl G, Krug D, Kehle D, Combs SE, Bermejo JL, Debus J, Sterzing F: Whole brain helical Tomotherapy with integrated boost for brain metastases in patients with malignant melanoma-a randomized trial. Radiat Oncol 2013, 8: 234. 10.1186/1748-717X-8-234
Aluwini S, van Rooij P, Hoogeman M, Kirkels W, Kolkman-Deurloo IK, Bangma C: Stereotactic body radiotherapy with a focal boost to the MRI-visible tumor as monotherapy for low- and intermediate-risk prostate cancer: early results. Radiat Oncol 2013, 8: 84. 10.1186/1748-717X-8-84
Awad R, Fogarty G, Hong A, Kelly P, Ng D, Santos D, Haydu L: Hippocampal avoidance with volumetric modulated arc therapy in melanoma brain metastases - the first Australian experience. Radiat Oncol 2013, 8: 62. 10.1186/1748-717X-8-62
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
The authors declare that they have no competing interest.
Authors’ contributions
MN planned, coordinated and conducted the retrospective analysis. NLJ performed PET imaging. MN & NLJ analyzed the PET and MRI imaging data as well as the treatment planning data. MR provided follow-up data. MN, NLJ, UG & CB prepared the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Niyazi, M., Jansen, N.L., Rottler, M. et al. Recurrence pattern analysis after re-irradiation with bevacizumab in recurrent malignant glioma patients. Radiat Oncol 9, 299 (2014). https://doi.org/10.1186/s13014-014-0299-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-014-0299-y