Abstract
Background
The role of human papillomavirus (HPV) in orthokeratinized odontogenic cysts (OOCs) has rarely been studied. The objective is to describe the clinicopathological findings in a series of OOCs from a Spanish population that were investigated in relation to the possible presence of HPV.
Methods
A clinicopathological retrospective analysis followed by a molecular analysis of 28 high- and low-risk HPV genotypes was performed in OOC samples of patients seen during the last 15-years in a Spanish tertiary care center.
Results
Of 115 odontogenic cysts with keratinization, 16 cases of OOCs were confirmed and evaluated. OOCs occurred predominantly in the mandible of males (mean age 36.06 ± 13.16 years). Swelling of the jaw followed by pain were the most common clinical symptoms, and 56.5% of the OOC cases were associated with an unerupted tooth. After a mean post-cystectomy follow-up of 3.8 years, only one recurrent case was observed, resulting in a verrucous cystic lesion that was considered premalignant after immunohistological examination. DNA extraction was successful from 14 of the 16 OOC cases. None of the primary OCCs or the single recurrent OOC were positive for HPV in the molecular analysis.
Conclusions
OOCs show a very limited potential for recurrence. Our results suggest that neither high- or low-risk HPV subtypes are likely to play a role in the etiology or neoplastic transformation of OOC, at least in the Spanish population.
Similar content being viewed by others
Background
Orthokeratinized odontogenic cyst (OOC) is a rare intraosseous cyst characterized by an orthokeratinized epithelial lining and minimal clinical aggressiveness [1]. OOCs were first described in 1927 by Schultz [2] as a variant of odontogenic keratocysts, now known as keratocystic odontogenic tumours (KCOTs) [3]. It was not until 1981 that Wright [4] described their clinicopathological aspects, indicating that OOCs are a distinct entity from odontogenic keratocysts. Several series of OOCs have been reported, confirming that their distinctive clinical, histopathological and biological features differ substantially from those of odontogenic keratocysts, as well as demonstrating a better prognosis and lower recurrence rates [1, 5, 6].
Nonetheless, rare cases of bilateral [7], multiple [8] and recurrent [9] OOCs have been reported, and although OOCs are considered clinically to be minimally aggressive, both dysplastic and malignant transformation have been reported [10]. OOCs sometimes transform into an uncommon type of well-differentiated squamous carcinoma known as carcinoma cuniculatum [11].
Over the last two decades, keratinizing cysts from various sites have been evaluated to assess a possible role of human papillomavirus (HPV) in their development and malignant transformation [12]. Reports are also available on odontogenic keratocysts [13] as well as carcinoma cuniculatum [14], in which specific HPV subtypes have been detected.
In this study, we evaluated the clinicopathological profile of OOCs seen at our institution over the last 15 years and analysed the possible presence of HPV.
Methods
This study was approved by our institutional Ethics Committee for Biomedical Research (protocol no. 2013/0045). Files of the Department of Pathology at La Fe University Hospital (Valencia, Spain) from 2000 to 2015 were reviewed. A retrospective search of a pathological diagnosis database (Pat Win® v4.6.0), employing the search terms “keratocyst”, “primordial cyst”, “keratocystic odontogenic tumor”, “orthokeratinized odontogenic cyst”, and “keratinized cyst”, to reflect changes in terminology over time, identified 115 odontogenic cysts with keratinization.
Histological and clinical revision
Following a histological review of these 115 cases, 16 cases of OOC were selected based on the morphological criteria established by Wright [4]. Lesions in which all or a predominant portion of the epithelial lining showed non-corrugated orthokeratinization, with the presence of a granular layer, were included in this series. The presence of this orthokeratinization on the epithelial surface as well as of a granular layer in the thickness of the epithelium was clearly demonstrated with PAS staining in all selected cases. Likewise, we also included lesions in which basal and parabasal cells were not prominent and did not palisade or polarize. Cystic lesions containing only focal OOC areas or various skin appendages (i.e. hair follicles and sebaceous and sweat glands) were excluded.
Clinical data, including age, sex, lesion location (maxilla or mandible) (anterior, premolar or molar regions), radiologic features, surgical procedures, and information on recurrence (including optical and immunohistochemical data obtained from the recurrent OOC samples), were reviewed.
Immunohistochemistry
Our immunohistochemical study, performed on recurrent OOC samples included the analysis of two well-known markers (p53 and Ki67), both of which are implicated in tumorigenesis and cell proliferation [6]. Briefly, 5-μm sections were cut from the original paraffin-embedded blocks and mounted on poly-L-lysine-coated glass slides prior to immunohistochemical staining, performed using monoclonal antibodies: mouse antihuman p53 (clone DO-7, dilution 1:50, Dako®, Glostrup, Denmark) and antihuman Ki67 (clone MIB-1, dilution 1:100, Dako®, Glostrup, Denmark). Immunostaining was visualized using the high-pH EnVision FLEX system (Dako®, Glostrup, Denmark); hematoxylin was used for counterstaining and for both techniques tonsil sections with oropharyngeal epithelium were employed as positive staining controls and the negative controls were mock-stained test sections (the primary antibody was replaced with PBS).
Amplification and detection of HPV DNA
After histological and clinical revision, formalin-fixed, paraffin embedded (FFPE) blocks of all selected OOC cases, including the one recurrent OOC, were retrieved from the archives of the Department of Pathology. The FFPE blocks were cut into three 5-μm sections, and DNA extraction was performed using a MagCore® Super HF16 automated nucleic acid extractor (RBC Bioscience Corp., New Taipei City, Taiwan).
For HPV detection and genotyping, an Anyplex II HPV28 (CE-IVD) kit (Seegene, Seoul, South Korea) was used to identify 14 high-risk and 14 low-risk HPV genotypes in two PCR reactions: mixture A (types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66 and 68) and mixture B (types 6, 11, 26, 40, 42, 43, 44, 53, 54, 61, 69, 70, 73 and 82), respectively. This semi-quantitative multiplex real-time PCR Anyplex II HPV28 system uses both dual priming oligonucleotides and tagging oligonucleotide cleavage and extension technology that combines five dyes and seven different melting-curve temperatures to distinguish the 28 HPV genotypes. PCR reactions were performed on a CFX96 real-time thermocycler (Bio-Rad Laboratories, Hercules, CA, USA) using 5 μL DNA for both mixtures A and B.
As internal control, the L1 gene of HPV DNA was simultaneously co-amplified with the human beta-globin housekeeping gene in the same PCR reaction tube. In addition, two positive controls (high-risk and low-risk HPV genotypes) were included in each PCR run along with two negative controls (non-template control) from the DNA extraction step and PCR experiment. Finally, all data from the PCR runs were interpreted using Seegene viewer software supplied by the manufacturer (Seegene, Seoul, South Korea).
Results
Clinicopathological data
The histological review of 115 keratinizing jaw cysts detected only 16 OOCs (13.91%). The cases were accepted for inclusion as OOC if they fulfilled the criterion of a complete or predominant epithelial lining with non-corrugated orthokeratinization and the presence of a granular layer. Of these 16 patients, 10 were male and 6 were female (male-to-female ratio, 1.66:1). Age at diagnosis ranged from 13 to 65 years (average 36.06 ± 13.16 years), with a clear predilection for the fourth decade of life (50%) in both sexes (Fig. 1). The mandible was affected in 12 cases (75%) and the maxilla in 4 (25%). Molars (65%) and premolars (16%) were the most commonly affected regions. Only one case showed bilateral involvement of two mandibular cystic lesions, which were diagnosed simultaneously. Of the 16 OOCs, 9 (56.5%) were associated with an impacted tooth, of which 6 were interpreted clinically as dentigerous cysts.
Jaw swelling was the most common symptom (12 cases; 75%). Four (25%) patients also complained of pain. The evolution of the symptoms ranged from 20 days to 5 years (mean, 9 months), with 7 patients (43.75%) having an evolution of less than 3 months. Interestingly, a maxillary OOC manifesting with odontogenic sinusitis was initially considered clinically and radiologically to be a periapical inflammatory cyst.
Enucleation, with or without curettage, was performed in 13 of the OOC cases; 1 case required marsupialization followed by enucleation, and the remaining 2 cases underwent a peripheral ostectomy because of their relatively large size. Related follow-up data were available for all patients. The follow-up period ranged from 12 to 120 months, average 31.12 months, during which only one case (1/16; 6.25%) recurred. We describe this case in detail below.
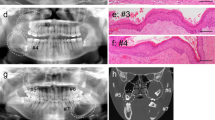
The only recurrence in our series was a teenage male (13 years old) who presented with a left mandibular radiolucent lesion measuring 30 mm, which displaced the roots of neighbouring molars without paresthesia, pain, or tooth mobility. Initially, an intra-oral double exodontia with cystectomy was performed. Histological examination revealed an odontogenic cyst lined by a stratified epithelium showing orthokeratotic keratinization on its surface as well as the presence of an evident layer of granular cells (Fig. 2a-c). Eight months after the cystectomy, the patient reported a painful swelling at the site of the operation. Panoramic radiography showed an increased radiolucent mandibular area with a poorly defined lower edge; new and wider curettage of the lesion was performed. Histological examination of the recurrent lesion revealed an OOC with features of verrucous hyperplasia. Distinct endophytic and “pushing” invasion together with a well-differentiated pattern of verrucous appearance showing dysplastic features with mild cellular atypia was observed, although there was no rupture of the basement membrane. Proliferative cellular activity (positive for Ki67) was not restricted to basal cells, and p53 expression was observed in all cell nuclei in the immunohistochemical analysis (Fig. 3a-f). These morphological changes were interpreted as early signs of malignization, although there was no evidence of invasive growth based on basement membrane integrity. After surgery, clinical and radiological long-term follow-up of the patient was planned. After 2 years of quarterly visits, there was no evidence of growth or new recurrence.
Recurrence of an OOC. Panoramic view showing the wall of a cystic lesion with large areas of hyperplastic verrucous growth with central filling by keratin (a), which is highlighted by PAS staining (b). Hyperplastic verrucous growth shows an endophytic and “pushing” well-differentiated pattern (c). Deeper portions showed epithelial nests with mild atypia and basement membrane integrity (d), which in the immunohistochemical analysis demonstrated proliferative cellular activity (Ki67 positivity) not restricted to the basal cell layer (e), as well as diffuse nuclear p53 reactivity (f)
Amplification and detection of HPV DNA
In total, 38 FFPE blocks from the 16 OOC cases (including the recurrent case 13) were used for DNA extraction. Two of the 16 OOCs (cases 5 and 7) were invalid for the Anyplex II HPV28 test due to lack of beta-globin amplification and were excluded from the study (see Table 1). For the remaining 14 cases, we performed HPV analysis in 32 FFPE blocks with good DNA quality, but observed no HPV positivity in any of the primary OOCs or the recurrent lesion.
Discussion
This study, complemented by molecular detection of HPV DNA, examined the largest series of OOCs affecting a Spanish population reported to date.
Of our odontogenic cysts with keratinization, 13.91% were identified as OOCs. This incidence agrees with those previously reported for OOCs (range 5.2–16.8%) among cases previously coded as KCOT [1, 5].
The average age at diagnosis of our patients was 36.06 ± 13.16 years with a tendency to occur during the fourth decade (50%). There was a male predominance, which is consistent with most published series [1, 4, 5, 9]. More than half our OOC cases were radiographically associated with an impacted tooth, a characteristic observed at varying rates in previous reports, with an average incidence of approximately 60.8% [1]. Of note in our series, a maxillary OOC that manifested clinically as odontogenic sinusitis was radiologically considered a periapical inflammatory cyst. Thus indicating that OOC should be included in the differential diagnosis of radiolucencies in the periapical region, especially considering that up to seven cases of an OOC resembling a radicular cyst have been described previously [15].
Regarding the evolution of OOCs, our study confirmed the low rate of recurrence of these cysts, with only one recurrence observed among 16 patients who were followed up after surgery for 12–120 months (average 31.12 months). This low recurrence rate is somewhat higher than the reported mean of 4%, based on pooled data from OOC series with adequate follow-up [9]; however, it is less than the overall rate reported for KCOTs (12–60%) [1]. This difference in the recurrence rate is important, since the morphological distinction of OOCs from KCOTs is supported mainly by studies that indicated a significantly lower rate of OOC recurrence following surgery [1, 4, 5].
Although rare, recurrence of OOC is possible, and may be indicative of malignant transformation. In our series, there was one recurrence observing hyperplastic verrucous changes in the lining of the OOC. These findings were histopathologically interpreted as atypical based on the overexpression of p53 as well as by the presence of proliferative activity in suprabasal cells. This case is unusual considering the young age of the patient, existence of a prior OOC, and the short period from the original OOC to recurrence; this supports the importance of performing additional microscopic studies of all resected cystic lesions in the jaws and the need for careful follow-up after their removal [10].
Previous studies have reported the appearance of verrucous proliferation in OOCs [16], as well as the possible emergence of squamous cell carcinomas (SCCs) from pre-existing OOCs [17]. Cysts with keratinization have a higher incidence of malignization than other OOCs [18], often presenting as highly differentiated SCCs [17], including cases of verrucous [19] or cuniculatum carcinoma [20], with some well-documented cases arising from OOCs [20,21,22,23]. Thus, although OOCs are considered clinically less aggressive lesions than KCOTs, the epithelial lining of OOCs may have neoplastic potential [21].
The pathogenesis of malignant transformation of OOC epithelia remains unclear [17]. Different hypotheses, such as long-standing chronic inflammation [17], genetic mutations in exon 6 of the TP53 gene [23] or oncogenic viral effects [13] have been suggested as predisposing factors, but the specific underlying mechanisms of this carcinogenesis remain unclear. It is thought that HPV may be associated with the pathogenesis of keratinizing OOC [13] and carcinoma cuniculatum [14], as well as some other carcinomas arising from epidermal cysts [12]. In addition, HPV may play a role in the development of verrucous proliferation in various sites, including oral locations [16, 24, 25]; however, this remains controversial [26].
In agreement with previous reports [16, 24, 27], we did not detect HPV genotypes in our molecular analysis of atypical verrucous hyperplasia in the recurrent case, suggesting that neither high- or low-risk HPV subtypes are likely to play a role in the pathogenesis of atypical verrucous changes that may develop into OOC recurrence. Moreover, molecular analysis did not detect HPV involvement in our series of primary OOC samples with successful DNA extraction. Thus, it is unlikely that HPV plays a role in the pathogenesis of OOCs, at least in the Spanish population. However, we cannot completely exclude that HPV is involved in OOCs in patients from other geographic areas, as commonly occurs in other virus-related disorders [28]. Additional epidemiological and molecular investigations in a large series of patients with OOCs of different ethnicities using molecular analysis of a broad spectrum of HPV types are required to confirm our results.
Conclusions
OOCs are a rare type of odontogenic cyst that show minimal clinical aggressiveness. Nonetheless, although very rare, recurrence is possible and can be a source of malignant transformation. Neither high- or low-risk HPV subtypes are likely to play a role, at least in the Spanish population, in the etiology of an OOC or in its neoplastic transformation.
Abbreviations
- FFPE:
-
Formalin-fixed, paraffin embedded
- HPV:
-
Human papillomavirus
- KCOT:
-
Keratocystic odontogenic tumour
- OOC:
-
Orthokeratinized odontogenic cyst
- PCR:
-
Polymerase chain reaction
- SCC:
-
Squamous cell carcinomas
References
Dong Q, Pan S, Sun L-S, Li T-J. Orthokeratinized odontogenic cyst. A clinicopathologic study of 61 cases. Arch Pathol Lab Med. 2010;134:271–5.
Schultz L. Cysts of the maxillae and mandibule. J Am Dent Assoc. 1927;14:1395–402.
Philipsen HP. Keratocystic odontogenic tumour in pathology and genetics of head and neck tumours. In: Barnes EL, Eveson JW, Reichart P, Sidransky D, editors. World Health Organization classification of Tumours. Lyon, France: IARC press; 2005. p. 306–7.
Wright JM. The odontogenic keratocyst: orthokeratinized variant. Oral Surg Oral Med Oral Pathol. 1981;51:609–18.
Crowley TE, Kaugars GE, Gunsolley JC. Odontogenic keratocysts: a clinical and histologic comparison of the parakeratin and orthokeratin variants. J Oral Maxillofac Surg. 1992;50:22–6.
Da Silva MJ, de Sousa SOM, Correa L, Carvalhosa AA, De Araujo VC. Immunohistochemical study of the orthokeratinized odontogenic cyst: a comparison with the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Radiol Endod. 2002;94:732–7.
Pimpalkar RD, Barpande SR, Bhavthankar ID, Mandale M. Bilateral orthokeratinized odontogenic cyst: a rare case report and review. Oral Maxillofac Pathol. 2014;18:262–6.
Cheng Y-SL, Liang H, Wright J, Teenier T. Multiple orthokeratinized odontogenic cysts. A case report. Head Neck Pathol. 2015;9:153–7.
MacDonald-Jankowski DS. Orthokeratinized odontogenic cyst: a systematic review. Dentomaxilloofacial Radiol. 2010;39:455–67.
Yoshida H, Onizawa R, Yusa H. Squamous cell carcinoma arising in association with an orthokeratinized odontogenic keratocyst. Report of a case. J Oral Maxillofac Surg. 1996;54:647–51.
Allon D, Kaplan I, Manor R, Calderon S. Carcinoma cuniculatum of the jaw: a rare variant of oral carcinoma. Oral Surg Oral Med Oral Pathol Radiol Endod. 2002;94:601–8.
Pusiol T, Zorzi MG, Piscioli F. Squamous cell carcinoma arising in epidermal and human papillomavirus associated cysts: report of three cases. Pathologica. 2010;102:88–92.
Cox M, Eveson J, Scully C. Human papillomavirus type 16 DNA in an odontogenic keratocyst. J Oral Pathol Med. 1991;20:143–5.
Knobler RM, Schneider S, Neumann RA, Bodemer W, Radlwimmer B, Aberer E, Söltz-Szöts J, Gebhart W. DNA dot-blot hybridization implicates human papillomavirus type 11-DNA in epithelioma cuniculatum. J Med Virol. 1989;29:33–7.
Servato JPS, Cardoso SV, Da Silva MCP, Cordeiro MS, Faria PR, Loyola AM. Orthokeratinized odontogenic cysts presenting as a periapical lesion: report of a case and literature review. J Endod. 2014;40:455–8.
Aldred MJ, Talacko AA, Allan PG, Shear M. Odontogenic cyst with verrucous proliferation. J Oral Pathol Med. 2002;31:500–3.
Bodner L, Manor E, Shear M, van der Waal I. Primary intraosseous squamous cell carcinoma arising in an odontogenic cyst – a clinicopathologic analysis of 116 reported cases. J Oral Pathol Med. 2011;40:733–8.
Brown RM, Gough NG. Malignant change in the epithelium lining odontogenic cysts. Cancer. 1972;29:1199–207.
Chaisuparat R, Coletti D, Kolokythas A, Ord RA, Nikitakis NG. Primary intraosseous odontogenic carcinoma arising in an odontogenic cyst or de novo: a clinicopathological study of six new cases. Oral Surg Oral Med Oral Pathol Radiol Endod. 2006;101:194–200.
Fonseca FP, Pontes HAR, Pontes FSC, Carvalho PL, Sena-Filho M, Jorge J, Santos-Silva AR, De Almeida OP. Oral carcinoma cuniculatum: two cases illustrative of a diagnostic challenge. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:457–63.
Shiar CH, Ng KH. Squamous cell carcinoma in an orthokeratinised odontogenic keratocyst. Int J Oral Maxillofac Surg. 1987;16:95–8.
Yoshida H, Onizawa K, Yusa H. Squamous cell carcinoma arising in association with an orthokeratinized odontogenic keratocyst. J Oral Maxillofac Surg. 1996;54:647–51.
Cox DP. P53 expression and mutation analysis of odontogenic cysts with and without dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:90–8.
Argyris PP, Nelson AC, Koutlas IG. Keratinizing odontogenic cyst with verrucous pattern featuring negative human papillomavirus status by polymerase chain reaction. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:e233–40.
Samman M, Wood H, Conway C, Berri S, Pentenero M, Gandolfo S, Cassenti A, Cassoni P, Al Ajlan A, Barrett AW, Chengot P, MacLennan K, High AS, Rabbitts P. Next-generation sequencing analysis for detecting human papillomavirus in oral verrucous carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:117–25.
Del Pino M, Bleeker MC, Quint WG, Snijders PJ, Meijer CJ, Steenbergen RD. Comprehensive analysis of human papillomavirus prevalence and the potential role of low-risk types in verrucous carcinoma. Mod Pathol. 2012;10:1354–63.
Lalla K, Mahomed F, Meer S. Keratinizing odontogenic cysts with a spectrum of verrucoid morphology: investigation of a potential role of human papillomavirus. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:625–30.
Hauck F, Oliveira-Silva M, Dreyer JH, Perrusi VJ, Arcuri RA, Hassan R, Bonvicino CR, Barros MH, Niedobitek G. Prevalence of HPV infection in head and neck carcinomas shows geographical variability: a comparative study from Brazil and Germany. Virchows Arch. 2015;466:685–93.
Funding
The authors of this article did not receive funding from any source for the design and realization of this study.
Availability of data and materials
The datasets used and/or analyzed supporting the conclusión of this article are available in the Service of Pathology (pathological diagnosis database platform Pat Win® v4.6.0) of La Fe University Hospital, Valencia, Spain, and may be provided by the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
FVS conceived the project, reviewed the process and drafted the manuscript. LFN made substantial contributions to the acquisition of clinical data. BVS and FVS performed the histological and immunohistochemical examination. LRM performed the HPV molecular analysis. LFN, LRM and BVS critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declares that they have no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee for Biomedical Research (protocol no. 2013/0045) of La Fe University Hospital, Valencia, Spain.
Consent for publication
Not applicable
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vera-Sirera, B., Rubio-Martínez, L., Forner-Navarro, L. et al. Orthokeratinized odontogenic cysts: a Spanish tertiary care centre study based on HPV DNA detection. Head Face Med 14, 10 (2018). https://doi.org/10.1186/s13005-018-0167-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13005-018-0167-3