Abstract
Background
The production of peripheral platelet is mainly regulated by thrombopoietin, which is a glycoprotein hormone predominantly synthesized in the liver. Previously, many studies have reported that there was an inverse correlation between the degree of chronic viral hepatitis and the peripheral platelet count. However, the effect of nonalcoholic fatty liver disease (NAFLD) on the peripheral platelet counts remains unclear.
Methods
With 1303 participants from “The prevention of MS and multi-metabolic disorders in Jiangsu province of China (PMMJS)” cohort study, we investigated the associations between NAFLD and the risk of platelet counts reduction in Chinese adults. The paired-samples T test was used to explore the platelet counts changes between baseline and follow-up. Multivariate logistic regression was used to examine the association between presence of NAFLD and the risk of platelet reduction by calculating the odds ratios (ORs) and 95% confidence interval (CI).
Results
After five years of follow-up, platelet counts were markedly reduced from 220.6 ± 42.22 (109/L) at baseline to 208.41 ± 40.70 (109/L) at follow-up in NAFLD group (P < 0.0001). However, platelet counts were slightly lowered from 213.2 ± 43.26(109/L) at baseline to 211.8 ± 41.65 (109/L) at follow-up in non-NAFLD people (P = 0.2349). Meanwhile, there was a significant association between NAFLD and the risks of platelet count reduction, even after adjustment for confounding variables (OR: 1.68, 95% CI: 1.06–2.67). Additionally, among the participants with BMI ≤ 23 kg/m2 and SUA ≤ 344.3 μmol/L, the NAFLD participants have an increased risk of platelet count reduction compared to the persons in non-NAFLD group.
Conclusions
Our present results suggested that NAFLD individuals have an increased risk of platelet counts reduction.
Similar content being viewed by others
Background
Currently, nonalcoholic fatty liver disease (NAFLD) affected about 20–40% of population in Western countries, 5–40% of the general population across the Asia-Pacific region and 20% of adults in China [1, 2]. Therefore, NAFLD has become the most common chronic liver disease worldwide and is considered as one of the leading public health problems [3], although simple NAFLD is usually benign and the mechanism of the development and progression of the disease has not been fully understood.
The peripheral platelet production is mainly regulated by thrombopoietin, which is a glycoprotein hormone predominantly synthesized in the liver. Previously, a number of studies have reported that there was an inverse correlation between the degree of chronic hepatitis and the peripheral platelet count [4, 5]. Moreover, the platelet count itself and platelet-related index, such as AP index, APRI index and FIB4 index have been widely used to evaluate the severity of various liver diseases, especially in the patient with chronic hepatitis B or C virus infection [6, 7]. However, the effect of NAFLD on platelet count is debatable. The results from a Japanese study suggested that the platelet counts could be served as an ideal biomarker of the severity of fibrosis in NAFLD patients [8]. However, a more recent study in Iran reported that NAFLD has nothing to do with peripheral platelet counts [9].
In a community-based study, Dai et al. reported that platelet counts may start to fall earlier in course of HCV-induced liver diseases [10]. However, the study on the risk of platelet counts reduction at the early stage of NAFLD remains scarce. Considering the clinical syndrome of NAFLD is generally mild and most NAFLD cases do not progress to more advanced stages of liver disease [3, 11], we therefore performed the present study to analyze the prospective association between NAFLD and the reduced platelet counts based on 1303 Chinese adults from a PMMJS cohort study.
Methods
Study population
All of participants were recruited from the study of PMMJS, which was a prospective cohort study established at 2003–2004 and aimed to investigate the prevalence of metabolism syndrome in Jiangsu, China. The detailed design and protocol and sampling method of PMMJS have been described previously [12]. Briefly, total 5067 persons (aged 30–75 years) were selected by multi-stage sampling method and completed the standard questionnaire at baseline (February 2003-Augest 2003). Between February and August 2007, 4661 (406 lost) individuals were accepted the first follow-up and received the additional hepatic ultrasound examination for fatty liver disease diagnosis. In 2012, 4661 persons with hepatic ultrasound examination were invited to participate in additional follow-up survey and 4339 persons (322 lost) completed the follow-up examinations.
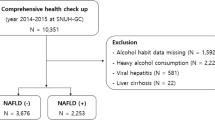
In the present study, we excluded subjects with any of the following reasons: excessive alcohol consumption (≥ 30 g/day in men or ≥ 20 g/day in women) (1048), liver cirrhosis or suspicion of malignancy (39), schistosomiasis infection history (29), HBsAg positive (355) and anti-HCV antibody positive [10]. We also ruled out subjects with abnormal platelet count (93) or the disease history of blood system (512) including anaemia (504) and leukaemia [8] at baseline. Moreover, we excluded the participants with hypertension (312) and diabetes (296) in order to avoid the effects of anti-hypertension and anti-diabetes medicines on the peripheral platelet counts. Additionally, 342 elder persons (age > 65 years, mean age: 73.49 ± 7.27) who could not provide blood samples at the 2012 follow-up were also excluded. Thus, a total of 1303 subjects (aged: 30–60 years at baseline) were included for analysis (Fig. 1).
Data collection and biomedical measurement
In the present study, the information collected in 2007 including the results of hepatic ultrasound examinations were used as baseline data. A standard questionnaire given to the participants contained the following: demographics (including age, gender, body weight, height and etc), smoking and drinking habits, disease history of hypertension and diabetes mellitus. Body mass index (BMI) was calculated by dividing weight in kilograms by height in meters squared. Blood pressure was measured three times using a mercury sphygmomanometer, with one minute interval between measurements after at least five minutes of rest in a seated position. The hepatic ultrasound examination was performed by an experienced radiologist, using a color ultrasound system (SoNoliNE Versa Plus, SIEMENS, German) with a 3.5-MHz probe.
A venous blood of 3 ml (ml) was collected in the morning after at least eight hours of fasting. Fasting plasma glucose (FPG), triglycerides (TG), total cholesterol (TC), LDL-cholesterol (LDL-C), HDL-cholesterol (HDL-C), serum uric-acid (SUA), serum creatinine (SCr), alanine aminotransferase (ALT), aspartate aminotransferase (AST) and γ-glutamyl transferase (GGT) were measured by using an autoanalyzer (Olympus AU640, Japan) with commercial reagents, respectively. The platelet count indices (PLT) were measured in EDTA-treated blood samples collected in 2–3 h, using an Advia 120 Hematology System (Bayer Corporation, Tarrytown, NY, USA) with commercial reagents.
Definitions
NAFLD diagnosis was assessed according to “Chinese Guideline on Diagnosis and Treatment of NAFLD (2006)” [13]. It was determined based on the presence of at least 2 of the following 3 abnormal findings: diffuse increased echogenicity of liver relative to kidney, ultrasound beam attenuation, and poor visualization of intrahepatic structures. In addition, the alcohol consumption should be less than 30 g/day in males and 20 g/day in females, respectively.
According to the results from previous study [14], we defined the persons with the risk of platelet reduction if their platelet counts in the following-up examination (2012) decreased by 20% or more of their initial platelet count at baseline (2007).
Statistical analysis
Data were analyzed using SAS 9.4 software (SAS Institute, Cary, NC, USA) and expressed as the mean ± standard deviation (SD), median or percentage as suitable. Comparisons between groups were analyzed by t-test or Mann–Whitney U-test for measurement data and Chi-square test for enumeration data. The incidence of platelet count reduction (decreased by more than 20%) was calculated for the NAFLD and non-NAFLD groups. Multivariate logistic regression was utilized to examine the association between presence of NAFLD and the risk of platelet count reduction by calculating the odds ratios (ORs) and 95% confidence interval (CI). In the multivariate models, some important confounders at baseline such as age, gender, smoking, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), FPG, TG, ALT, AST, LDL-C and HDL-C level were included as covariates. All reported P values are two-tailed, and those < 0.05 were considered statistically significant.
Results
Baseline characteristics of studied population
Totally, 946 males and 357 females were included in the present study, with a mean age of 49.64 ± 8.15 years and 48.87 ± 7.65 years, respectively. Among them, 454/946 males were diagnosed as NAFLD, which was significantly higher than those in females (73/357, χ2 = 27.97, P < 0.001). As the results shown, the mean platelet count in the NAFLD and non-NAFLD subjects was 220.6 ± 42.22 and 213.2 ± 43.26 (109/L) at baseline, respectively. There was a statistical difference between two groups (P = 0.0023). In addition, NAFLD and non-NAFLD subjects differed significantly in many parameters, such as BMI, ALT, AST, LDL-C, HDL-C and TG. Clinical and biochemical characteristics of study population were summarized in Table 1.
Associations between NAFLD and the risk of platelet reduction
As the results shown, platelet counts were markedly reduced from 220.6 ± 42.22 (109/L) at baseline to 208.41 ± 40.70 (109/L) at the follow-up in NAFLD group (P < 0.0001). However, platelet counts were only slightly lowered from 213.2 ± 43.26 (109/L) at baseline to 211.8 ± 41.65 (109/L) at the follow-up in non-NAFLD group (P = 0.2349).
As Fig. 2 shown, 203, 59, 13 NAFLD individuals and 272, 62, 17 non-NAFLD persons were determined with ≥10%, ≥ 20% and ≥ 30% of platelet counts reduction of their initial counts at baseline, respectively. When we defined the persons with the risk of platelet count reduction if their platelet counts in the following-up examination decreased by 20% or more of their initial count at baseline, 72 persons were determined with the risk of platelet reduction in NAFLD group, which was significantly higher than those in the non-NAFLD group (72/527 vs 79/776, P = 0.001).
In comparison with the individuals with non-NAFLD, NAFLD participants had an OR (95% CI) of 1.91 (1.31–2.78) for having an increased risk of platelet count reduction (≥20%) in unadjusted logistic models. As the results shown in Table 2, the significant association was not affected after adjustment for age, gender, BMI, FPG, SBP and DBP (model 1 and 2), and further adjustment for ALT and AST, SCr and SUA in model 3. Moreover, in fully adjusted models including HDL-C, LDL-C and TG, the results remained to show that the NAFLD significantly associated with the risk of platelet reduction (OR: 1.68, 95% CI: 1.06–2.67).
We further conducted stratified analyses to evaluate the effects of NAFLD on platelet count reduction. As the results shown in Table 3 and Additional file 1: Table S1, among the participants with BMI ≤ 23 kg/m2 and SUA ≤ 344.3 μmol/L, the NAFLD participants have an increased risk of platelet count reduction compared to the persons in non-NAFLD group (OR: 3.36, 95% CI: 1.20–9.45 for BMI, and OR: 3.69, 95% CI: 1.35–10.10 for SUA, respectively).
Discussion
Although the platelet-related index has been used to predict degrees of fibrosis in the persons with chronic hepatitis [15], the characteristic of platelet counts variation at the early stage of NAFLD has not yet been illustrated by prospective, community-based study. Moreover, most NAFLD cases simultaneously suffer from hypertension or hyperlipidemia and routinely take antiplatelet medicines. Therefore, it is rational to perform the present study to evaluate the association between NAFLD and the risk of platelet count reduction in Chinese adults. As the results shown, our present study revealed that platelet counts were markedly decreased in NAFLD individuals compared to those people without NAFLD. Furthermore, among the participants with lower levels of BMI and SUA, the NAFLD participants have an increased risk of the platelet count reduction compared to those subjects in non-NAFLD group. The mechanism of NAFLD causing platelet counts reduction is multifactorial. Several studies have reported that lower platelet count was not only negatively correlated with liver fibrosis, but also associated with the progression of chronic viral hepatitis or alcoholic hepatitis [16,17,18]. Additionally, the liver is an important organ for thrombopoietin producing. During the development and progression of NAFLD, excessive lipid deposition and oxidative stress could impair the mitochondrial functions through inflammatory mediators and then affected thrombopoietin synthesis [19,20,21]. Reduced platelet counts could happen in this process.
In a Korean cross-sectional study, Shin et al. have observed that the increased values of mean platelet volume (MPV) was significantly associated with the prevalence of non-alcoholic hepatic steatosis in obese population, even after adjustment for confounding variables [22]. In a recent meta-analysis, Madan et al. also reported that MPV is significantly higher in patients with NAFLD, indicating the presence of increased platelet activity in such patients [23]. Therefore, the previous and present findings implicated that the characteristics of the peripheral platelet in NAFLD individuals should be further investigated in future. Furthermore, considering some drugs like aspirin could decrease the peripheral platelet counts and was generally used in the NAFLD patients co-existed with chronic metabolic diseases such as hypertension and hyperlipidemia [24, 25], more larger studies are needed to establish whether a platelet examination including platelet counts, MPV and etc., should be routinely performed in all NAFLD individuals.
Although the present longitudinal follow-up, prospective study considerably enabled us to further understand the risk of platelet reduction in NAFLD persons, some limitations in the present study should be noted. First, the impacts of portal pressure or splenomegaly on the platelet counts were not investigated in the present study. Second, the inflammatory immune changes in NAFLD individuals were not analyzed, which has been considered as an important factor associated with the platelet count decline in chronic hepatitis B or C patients [26, 27]. Third, we did not analyze the association between platelet count and NAFLD-related fibrosis/cirrhosis because fibrosis or cirrhosis should be determined by liver biopsy, and we did not collect the markers of NAFLD fibrosis/cirrhosis at baseline. This concern should be further explored in future study.
Conclusions
Summary, our present study provided the evidence that NAFLD individuals have a significantly increased risk of platelet counts reduction compared to those without NAFLD. The results should be important for clinicians that the peripheral platelet counts need to be monitored in the NAFLD individuals, especially in the persons with antiplatelet medicines.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BMI:
-
body mass index
- DBP:
-
diastolic blood pressure
- FBG:
-
fasting blood glucose
- GGT:
-
glutamyltransferase
- Hb:
-
hemoglobin
- Hct:
-
hematocrit
- HDL-C:
-
high-density lipoprotein
- LDL-C:
-
low-density lipoprotein
- NAFLD:
-
nonalcoholic fatty liver disease
- PLT:
-
platelets
- PMMJS:
-
The prevention of MS and multi-metabolic disorders in Jiangsu province of China
- SBP:
-
systolic blood pressure
- SCr:
-
serum creatinine
- SUA:
-
serum uric-acid
- TG:
-
triglycerides
- WBC:
-
white blood cell count
References
Malhotra N, Beaton MD. Management of non-alcoholic fatty liver disease in 2015. World J Hepatol. 2015;7:2962–7.
Fan JG. Epidemiology of alcoholic and nonalcoholic fatty liver disease in China. J Gastroenterol Hepatol. 2013;28:11–7.
Mansoor S, Collyer E, Alkhouri N. A comprehensive review of noninvasive liver fibrosis tests in pediatric nonalcoholic fatty liver disease. Curr Gastroenterol Rep. 2015;17(23).
Murali AR, Attar BM, Katz A, Kotwal V, Clarke PM. Utility of platelet count for predicting cirrhosis in alcoholic liver disease: model for identifying cirrhosis in a US population. J Gen Intern Med. 2015;30:1112–7.
Riediger C, et al. Low postoperative platelet count is associated with negative outcome after liver resection for hepatocellular carcinoma. Hepato-Gastroenterology. 2014;61:1313–20.
Karasu Z, et al. Liver fibrosis is associated with decreased peripheral platelet count in patients with chronic hepatitis B and C. Dig Dis Sci. 2007;52:1535–9.
Testa R, et al. Noninvasive ratio indexes to evaluate fibrosis staging in chronic hepatitis C: role of platelet count/spleen diameter ratio index. J Intern Med. 2006;260:142–50.
Yoneda M, et al. Japan study Group of Nonalcoholic Fatty Liver Disease. Platelet count for predicting fibrosis in nonalcoholic fatty liver disease. J Gastroenterol. 2011;46:1300–6.
Garjani A, Safaeiyan A, Khoshbaten M. Association between platelet count as a noninvasive marker and ultrasonographic grading in patients with nonalcoholic fatty liver disease. Hepat Mon. 2015;15:e24449.
Dai C, et al. Hepatitis C virus viremia and low platelet count, a study in hepatitis B & C endemic area in Taiwan. J Hepatol. 2010;52:160–6.
Krishan S. Correlation between non-alcoholic fatty liver disease (NAFLD) and dyslipidemia in type 2 diabetes. Diabetes Metab Syndr. 2016;S1871-4021:30047–53.
Luo W, et al. A population association study of PPAR δ gene rs2016520 and rs9794 polymorphisms and haplotypes with body mass index and waist circumference in a Chinese population. Ann Hum Biol. 2016;43:67–72.
Fan JG. An introduction of strategies for the management of nonalcoholic fatty liver disease (NAFLD) recommended by Asia Pacific working party on NAFLD. Zhonghua Gan Zang Bing Za Zhi (Chinese). 2007;15(552–553).
Gallet R, et al. Effect of transcatheter (via femoral artery) aortic valve implantation on the platelet count and its consequences. Am J Cardiol. 2013;111:1619–24.
Gisondi P, Barba E, Girolomoni G. Non-alcoholic fatty liver disease fibrosis score in patients with psoriasis. J Eur Acad Dermatol Venereol. 2016;30:282–7.
Cui WJ, Zhu FQ, et al. Correlation between thrombocytopenia in chronic hepatitis B and chronic hepatitis B with liver cirrhosis. Journal of Xi’an Jiaotong University(Medical Sciences). 2011;32:85–8.
Karasu Z, Tekin F, Ersoz G, et al. Liver fibrosis is associated with decreased peripheral platelet count in patients with chronic hepatitis B and C. Digestive Diseases & Sciences. 2007;52:1535–9.
Loomba R, Abraham M, Unalp A, et al. Association between diabetes, family history of diabetes, and risk of nonalcoholic steatohepatitis and fibrosis. Hepatology. 2012;56:943.
Gressner AM. Mediators of hepatic fibrogenesis. Hepato Gastroenterol. 1996;43:92–103.
Adams LA, Lymp JF, Sauver JS, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–21.
Kawasaki T, Takeshita AK, Kobayashi Y, et al. Serum thrombopoietin levels in patients with chronic hepatitis and liver cirrhosis. Am J Gastroenterol. 1999;94:1918–22.
Shin WY, Jung DH, Shim JY, Lee HR. The association between non-alcoholic hepatic steatosis and mean platelet volume in an obese Korean population. Platelets. 2011;22:442–6.
Madan SA, John F, Pitchumoni CS. Nonalcoholic fatty liver disease and mean platelet volume: a systemic review and meta-analysis. J Clin Gastroenterol. 2016;50:69–74.
Ajjan RA, Grant PJ. The role of antiplatelets in hypertension and diabetes mellitus. J Clin Hypertens (Greenwich). 2011;13:305–13.
Sarbacker GB, Lusk KA, Flieller LA, Van Liew JR. Aspirin use for the primary prevention of cardiovascular disease in the elderly. Consult Pharm. 2016;31:24–32.
Wang Q, et al. The severity of liver fibrosis influences the prognostic value of inflammation-based scores in hepatitis B-associated hepatocellular carcinoma. Ann Surg Oncol. 2015;(Suppl 3):1125–32.
Aiolfi R, Sitia G. Chronic hepatitis B: role of anti-platelet therapy in inflammation control. Cell Mol Immunol. 2015;12:264–8.
Funding
This work was supported by the project-sponsored by SRF for ROCS, SEM (K513901814), the Soochow University high-level scientific research foundation for the introduction talent (Q413900612), Pre-research foundation for nature science of Soochow University (Q313904713), and Key technologies of prevention and control of diseases and infectious diseases in Suzhou City(Gwzx201506、Gwzx201605、 Gwzx201706).
Availability of data and materials
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: LC and HZ. Collected and analyzed data: ZG, CD, LY, YW, CL, JQ, YX, XL and YX. Wrote the paper: FL and LC. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All of participants were asked to provide informed consent and the study protocol was approved by the ethics committees of Soochow University. The methods were carried out in accordance with the ethical guidelines of the 1975 Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Stratified analysis of NAFLD and platelet count in different subgroup. (DOCX 27 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Liu, F., Zhou, H., Cao, L. et al. Risk of reduced platelet counts in patients with nonalcoholic fatty liver disease (NAFLD): a prospective cohort study. Lipids Health Dis 17, 221 (2018). https://doi.org/10.1186/s12944-018-0865-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-018-0865-7