Abstract
Background
Developing countries, such as India, are experiencing rapid urbanization, which may have a major impact on the environment: including worsening air and water quality, noise and the problems of waste disposal. We used health data from an ongoing cohort study based in southern India to examine the relationship between the urban environment and homeostasis model assessment of insulin resistance (HOMA-IR).
Methods
We utilized three metrics of urbanization: distance from urban center; population density in the India Census; and satellite-based land cover. Restricted to participants without diabetes (N = 6350); we built logistic regression models adjusted for traditional risk factors to test the association between urban environment and HOMA-IR.
Results
In adjusted models, residing within 0–20 km of the urban center was associated with an odds ratio for HOMA-IR of 1.79 (95% CI 1.39, 2.29) for females and 2.30 (95% CI 1.64, 3.22) for males compared to residing in the furthest 61–80 km distance group. Similar statistically significant results were identified using the other metrics.
Conclusions
We identified associations between urban environment and HOMA-IR in a cohort of adults. These associations were robust using various metrics of urbanization and adjustment for individual predictors. Our results are of public health concern due to the global movement of large numbers of people from rural to urban areas and the already large burden of diabetes.
Similar content being viewed by others
Background
Currently, 54% of the world’s population lives in urban areas, a proportion that is expected to increase to 66% by 2050 [1]. Most of the expected urban growth will take place in developing countries in Asia and Africa. Next to China, the world’s second largest urban population resides in India with approximately 410 million people and this number is projected to double by 2050 [1].
India had over 69.2 million people living with diabetes in 2015, and this number is expected to grow to 123.5 million by 2040 [2, 3]. In India, urban compared to rural populations have significantly higher diabetes prevalence [4, 5]. Studies have shown that urbanization in India is associated with increased consumption of energy-rich foods and a decrease in energy expenditure (through less physical activity) leading to obesity and increased risk of developing type 2 diabetes mellitus (diabetes) and other cardiometabolic conditions [5,6,7,8]. Rapid urbanization in India also often coincides with increased environmental pollution with potential harmful effects to health due to undesirable changes in the physical, chemical or biological characteristics of air, water or land [9]. Emerging epidemiologic data suggests that environmental pollutants could be a risk factor for diabetes [10, 11].
In a study in Chennai the overall diabetes prevalence increased from 11.6% in 1995 to 13.9% in 2000 [15]. Chennai, located in the rapidly urbanizing southern state of Tamil Nadu, is the fourth largest metropolitan city in India. Subsequent studies of adults over 20 years old in Chennai showed that the prevalence of diabetes increased from 14.3% in 2003–2004 to 18.6% in 2006 [3, 4]. In a more recent study (2010–2011) the age standardized prevalence of diabetes in Chennai was 22.8% (95% CI 21.5–24.1%) [12]. These results indicate a rapid increase in prevalence of diabetes in Chennai city in recent decades [3, 4, 12, 13]. In a comparative study, residents in Chennai had lower BMI and waist circumference (WC) measurements than Asian Indians living in the U.S., but still had a higher prevalence of diabetes even at normal levels of BMI [14]. Adjustment for age, sex, WC, and systolic blood pressure did not fully explain differences in the odds of diabetes between the two groups suggesting that factors besides age and central adiposity play a role in diabetes development.
There is minimal data on urban environmental degradation and risk for diabetes in developing countries such as India [9]. Insulin resistance, which is a reduction in the cellular response to endogenous insulin, is a powerful predictor of future development for diabetes [15]. Studies have shown links between insulin resistance and various chemicals, such as phthalates and bisphenol A (BPA), found in polluted environments [16,17,18]. Animal and recent epidemiological studies have reported that air pollutants, such as, nitrogen dioxide (NO2) and PM2.5 may affect insulin sensitivity [19,20,21]. Given the high levels of environmental pollutants in India, it is plausible that some of these pollutants could be factors within the urban environment contributing to increased diabetes risk [5].
In the current study, while controlling for traditional risk factors, we examine the cross sectional association between insulin resistance and measures of urban environment defined using the following metrics: (1) distance from urban center; (2) population density in the India Census; and (3) satellite-derived land cover type. We used health data from the Population Study of Urban, Rural, and Semi-urban Regions for the Detection of Endovascular Disease and Prevalence of Risk Factors and Holistic Intervention Study (PURSE-HIS) in a population recruited from Chennai and surrounding areas [22].
Methods
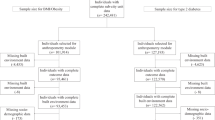
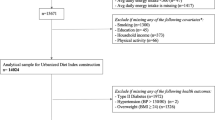
The PURSE-HIS was designed and implemented to understand the prevalence and progression of subclinical and overt cardiovascular disease (CVD) and its risk factors in urban, semi-urban, and rural communities in southern India. Detailed methodology has been published elsewhere [22]. Briefly, Chennai served as the primary location from which the urban study population was recruited. The semi-urban and rural areas were near Chennai in the Thiruvallur and Kanchipuram districts, respectively. A total of 8080 participants over 20 years of age were recruited between 2009 and 2011 from urban (N = 2221), semi-urban (N = 2821) and rural (N = 3038) areas. A two stage cluster sampling method was used to ensure adequate spatial variability amongst administrative divisions. After excluding participants with a previous history of diabetes or newly diagnosed diabetes (a fasting blood glucose ≥ 126 mg/dL or a 2-h oral glucose tolerance test (OGTT) ≥ 200 mg/dL) our sample size was 6350; which included 3670 females and 2680 males.
Questionnaire and clinical data collection
An interviewer-administered questionnaire was used to collect data on demographics, CVD and its risk factors [22]. Physical activity was measured by a physiotherapist using the Global Physical Activity Questionnaire [23] and a score was calculated. A clinical psychologist assessed the level of stress and anxiety levels using the Presumptive Stressful Life Event Scale [24]. A socioeconomic (SE) score was computed based on a revision of the Kuppussamy classification scale [25, 26]. Kuppuswamy’s SE score was originally proposed in 1976 and was built for the Indian population combining values for education, occupation, education and income to create a robust estimate of standard of living. Participants are categorized into lower, middle and upper classes. Energy (food) intake was assessed from a 24-h recall of meals and a food frequency questionnaire [27]. Body mass index (BMI) was calculated by dividing the participant’s measured weight in kilograms by the square of height in meters. Fasting blood specimens were collected and assayed for fasting blood sugar (FBS) and fasting insulin levels [22]. Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as fasting plasma insulin (mU/L) × FBS (mmol/L)/22.5. Since a diagnostic test for insulin resistance does not exist, insulin resistance was defined as a HOMA-IR level above the 75th percentile, as previously defined in multiple cohort and epidemiological studies [28].
Geo-location and creation of urbanization metrics
We defined urbanization using three different metrics: distance from urban center (Chennai), land cover type, and census community designation. Residential addresses of study participants were geolocated to the nearest road or intersection through manual assignment by a single researcher using Google Earth© over the study area that spanned a geographic region of approximately 80 km by 80 km (Fig. 1). For quality control purposes, the Google Earth© location identification process was repeated by a second researcher with 100 randomly selected participants to examine potential positional error. We found minimal error in the geolocation of participants. The average difference in distance for the randomly selected participants was 0.18 km with a minimum of 0.01 km and a maximum of 0.42 km.
For the first metric, the urban center of the study region was defined as the flag post on the ramparts of the Fort Saint George historic landmark in Chennai, in accordance with historical and local custom. Residential location KML files were imported into ArcGIS v10.1 (ESRI, Redlands, CA) to calculate the distance, in kilometers, and compass angle from the urban center for each participant using the Near Tool.
The second metric utilized land cover data (MCD12Q1, NASA) obtained through the online Data Pool at the NASA Land Processes Distributed Active Archive Center. The values were derived from Terra and Aqua-MODIS land cover data products which provided yearly averages [29]. The data presented are from the year 2010 and have 500 m × 500 m resolution. We based our groups on the 17 land cover classifications of the International Geosphere Biosphere Program Plant Functional Scheme, which together have 72–77% classification accuracy [30]. We mapped the classifications as five distinct groups, which included urban, trees/shrubs, grass, crops, and other (Fig. 1). (The figure also includes water for illustration; however, no participants resided in these grids.) We then aggregated all the non-urban land classifications into a single group, which we designated as rural and the remaining groups as urban.
The third metric, census community designation, was based on data from the 2011 India census. Participants residing in urban areas were those living in a municipality with a total population of at least 5000 and a population density of 400 persons/km2 or more. Those residing in municipalities with smaller populations or densities were designated as non-urban [31].
Statistical analyses
We first evaluated descriptive statistics for population characteristics according to urban designation and separated by gender. Analysis of variance was used to check for significant differences on mean scores in both genders between rural and urban residents. Analysis of variance was also used to test for significant differences in HOMA-IR scores according to categories of age (≤ 39 or ≥ 40), body mass index (non-obese [BMI ≤ 24.9] or obese [BMI ≥ 25]), physical activity (low, moderate or high), SE score (lower, middle or upper) and smoking (smoker or non-smoker). We ran logistic regression models to evaluate the association between each urbanization metric and the odds of having a HOMA-IR level in the fourth quartile of the distribution.
Logistic regression models were adjusted for age, BMI, physical activity, energy intake, SE score and smoking in separate models for males and females. However, no adjustment for smoking was made in the models for females due to the very low prevalence of smoking. We evaluated effect modification, in models with distance to urban center as the exposure, by stratifying on categories of age, smoking status, BMI and physical activity. Potential modifiers were removed as covariates in the model as appropriate when evaluating modification. The standardized coefficients and 95% confidence intervals were multiplied by the interquartile range (IQR) (i.e. 32.6 km). We also conducted a sensitivity analysis that substituted WC for BMI in adjusted regression models.
Results
Population characteristics are given in Table 1. The mean age for females was 40 years and for males was 45 years. In both females and males, when compared to the rural population, the urban population had a significantly higher energy intake, SE score, stress score, insulin level and HOMA-IR. The urban population also had a higher BMI and was less physically active. The prevalence of smoking was higher in rural males compared to urban males and despite an overall low prevalence, smoking was higher among urban females compared to rural females.
Table 2 shows HOMA-IR levels stratified by demographic and urbanization variables. The overall mean HOMA-IR levels were 1.98 ± 1.61 for females and 1.71 ± 1.39 for males. HOMA-IR levels in both females and males were significantly higher in sub-populations with low and moderate physical activity compared to high physical activity. HOMA-IR levels were significantly higher among non-smoking males compared to smoking males and also higher for participants who were obese. There were no statistically significant differences by age, however, mean HOMA-IR was slightly higher for older females and younger males. HOMA-IR levels were higher for residents of urban areas compared to non-urban. Mean HOMA-IR levels were 2.69 ± 2.44 for females and 2.39 ± 2.29 for males living within 0–20 km from city center. This was statistically significantly higher than their counterparts living at a greater distance. Urban designation compared to rural according to land area was statistically significantly higher among females and males. Similarly, census derived urban residence was statistically significantly higher for females and males compared to rural populations.
Results of unadjusted and adjusted logistic regression models of HOMA-IR are given in Table 3. Adjustment for potential confounders resulted in an attenuation of the effect in most cases. The OR for high HOMA-IR appeared to increase as distance to urban center decreased. In adjusted models, using distance from urban center, residing within 0–20 km was associated with an OR for high HOMA-IR of 1.79 (95% CI 1.39, 2.29) for females and 2.3 (95% CI 1.64, 3.22) for males compared to residing in the furthest 61–80 km group. Increased ORs ratios were also found for females living in the 20–40 km distance category (1.72 [95% CI 1.39, 2.29]) and for males living at distances of 20–40 km (1.59 [95% CI 1.11, 2.29]) and 41–60 km (1.77 [95% CI 1.19, 2.64]). Based on land cover, urban females (1.31 [95% CI 1.10, 1.50]) had significantly higher OR for HOMA-IR, while the effect for urban males was higher, but not statistically significant (1.20 [95% CI 0.98, 1.60]). Based on census community designation, the adjusted models showed that residing in an urban area resulted in a significantly higher OR in males (1.35 [95% CI 1.07, 1.72]), but not females (1.04 [95% CI 0.88, 1.24]).
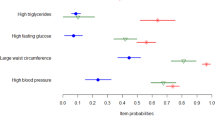
Changes in HOMA-IR are estimated for an IQR increase in distance to urban center (32.6 km). We also examined the modification of the association between distance to urban center and HOMA-IR by age, smoking, BMI, physical activity and energy intake in sex-stratified multivariate models (Additional file 2: Figure 1). Results show a significant increase in HOMA-IR the closer participants resided to the urban center of Chennai, with 0.19 mg/dL (95% CI 0.13, 0.25) and 0.16 mg/dL (95% CI 0.09, 0.22) increase in HOMA-IR per IQR increase in distance in females and males, respectively. The estimated change in HOMA-IR corresponding to a distance of 80 km from city center is 23% of the mean for females and males, 0.46 mg/dL and 0.39 mg/dL, respectively. The association was more pronounced in younger females who had a 0.25 mg/dL (95% CI 0.16, 0.35) increase in HOMA-IR for an IQR change in distance compared to 0.15 mg/dL (95% CI 0.03, 0.25) for older females. Closer proximity to the urban center was associated with a higher effect on HOMA-IR among obese males (0.28 mg/dL [95% CI 0.16, 0.43]) compared to non-obese males (0.09 mg/dL [95% CI 0.16, 0.43]). However, effects between obese and non-obese females were similar. In both males and females there was a greater effect of distance on HOMA-IR for participants reporting moderate and low physical activity compared to high physical activity, although there was a high degree of overlap in confidence intervals.
A sensitivity analysis was conducted that replaced BMI with WC in the adjusted logistic regression models (Additional file 1: Table 1). The models adjusting for WC had a significantly lower magnitude of association between an IQR distance from urban center in males (0.09 mg/dL [95% CI 0.16, − 0.013]) than in the models adjusting for BMI, but was not significantly different in females (− 0.16 mg/dL [95% CI − 0.22, − 0.09]).
Discussion
In a population-based representative sample of adults in India without diabetes we investigated the association between residing in an urban environment and insulin resistance, which is an important underlying metabolic condition predisposing the development of diabetes [32, 33]. After controlling for age, BMI, energy intake, SE score, physical activity, stress and smoking status, there were independent associations between multiple metrics of urban environment and HOMA-IR. Those residing in urban areas as defined by land cover and census category had higher HOMA-IR levels than those in rural or non-urban areas. The largest increase was found for participants living within 20 km of the city center.
In multivariate models there were gender-specific differences of the effect of age and obesity on the association between distance from the urban center and HOMA-IR such that the association was more pronounced in younger females and among obese males. Previous, studies in young populations suggest that girls are intrinsically more insulin resistant [34]. Further, reports show that type 2 diabetes in younger populations show a female preponderance [35,36,37]. However, at older ages with increases in BMI, there is a greater amounts of visceral and hepatic adipose tissue in males, when compared with females, which contributes to higher insulin resistance in males [38]. These findings are consistent with the greater effect modification of the relationship between distance from urban center and HOMA-IR among younger females and obese males that we found.
A small number of studies have evaluated the impact of urbanization on insulin resistance in varied locations across the globe. A higher prevalence of insulin resistance was identified in Floresian men (a specific ethnic group in Indonesia) that had moved to an urban center (Jakarta) compared to men than remained in the rural area [39]. Similarly, another study revealed statistically significant higher HOMA-IR in Ghanaian adults living in urban areas compared to rural areas [40].
Due to urbanization in India, environmental degradation has been occurring very rapidly resulting in poor water quality, air pollution, noise, dust and heat, as well as problems with disposal of solid and hazardous wastes [9]. Thirteen of the world’s 20 cities with the highest levels of particulate matter less than 2.5 μm in aerodynamic diameter (PM2.5) are located within India. Significant sources of air pollution in India include motor vehicles, electricity generation, manufacturing, construction and road dust, which have increased in India’s cities in recent years along with the rapid growth in industry, power and transportation [41]. Air pollution, specifically PM2.5 and nitrogen dioxide, have achieved recent attention given associations with diabetes and insulin resistance in multiple studies [10, 20, 42, 43]. Proposed mechanisms for these effects include oxidative stress; endothelial dysfunction; overactivity of the sympathetic nervous system; changes in immune response in visceral adipose tissues; and altered insulin sensitivity and glucose metabolism [42, 43]. Other chemicals such as persistent organic pollutants and endocrine disruptors have also been associated with diabetes [11]. These chemicals may act as antagonists or agonists to endogenous hormones necessary to maintain homeostasis or affect normal functioning of mitochondria [44]. However, it is important to note the spatial variation and temporality between increased pollution and this health effect, because there may be a lag between further degradation of the environment and diagnosis of adverse effects. Understanding the relationship between pollution and insulin resistance will require a more detailed analysis of these temporal trends.
Other contributors to this association are also possible including access to qualified medical care. Past research has found that although there is a greater concentration of medical workers in urban areas a large proportion of those practitioners are also unqualified [45]. Diet is a key factor in insulin resistance and evidence of differences comparing urban and rural populations is mixed. One study reported similar fruit and vegetable intake among both populations [46], another reported high intake of fruits and vegetables, along with higher intake of carbohydrates, meat and dairy for urban populations [47].
One of the strengths of our study is the use of three metrics to test the associations between urban environment and HOMA-IR. Land cover classification allowed us to reduce exposure misclassification by identifying smaller or developing urban enclaves outside of the city center. For example, we could identify a rapidly urbanizing municipality approximately 65 km southwest from the urban center (Fig. 1) that was classified as rural in the India Census data. Female participants residing in this second urban cluster had a mean HOMA-IR of 1.83 mg/dL (SD: 2.17 mg/dL), which was significantly higher than female participants residing in the same distance interval (60–80 km distance group), who had a mean HOMA-IR of 1.57 mg/dL (SD: 0.97 mg/dl). It is possible that the second urban cluster introduced exposure misclassification in the multivariate analysis based on Census classification resulting in a null effect (Table 3). However, examining three metrics reveals an overall commonality of the association between urban residence and higher HOMA-IR.
Our study also has several limitations. Although the land cover data are able to identify rapidly developing urban areas we must compare data for temporally close, but different, years. This will result in some error, which we have sought to address by gathering data on exposure before outcome. Also, the land cover classifications do not differentiate specific land uses within urban areas. There are likely to be differential exposures comparing residential versus industrial land use that may be important to the outcome. Another potential limitation is our geocoding method. Geocoding participant locations can be difficult in rapidly developing regions in India without reliable address network systems and Global Position System (GPS) ascertainment is not viable with large sample populations. Exposure misclassification from positional error could affect our analysis at the edges of our distance interval cut points, as well as with the 500 m × 500 m MODIS land cover grids. Nevertheless, in a subset of participants for whom we compared the geocoded location to the location recorded from a GPS, the mean difference was 0.19 km which is relatively small compared to the 20 km distance categories used in our main analysis. We would anticipate this error to be non-differential with respect to our outcome and therefore would be expected to bias results towards the null.
We found that adjustment for WC instead of BMI resulted in an attenuation of effects among males. This indicates possible residual confounding when using BMI as the measure for adiposity, which may not adequately account for fat distribution. Finally, the study design of our analysis was cross-sectional. We are therefore limited in our ability to evaluate temporality with regard to urban expansion and the effect of urbanization on HOMA-IR. Future work with this cohort may allow us to draw stronger conclusions about which aspects of the urban environment may be most important to the association with HOMA-IR and whether there is a causal association. Future analyses could consider ambient and household air pollution, which are often pervasive, persistent and exist at higher concentrations in urban areas of India [9].
Conclusion
We have identified independent associations between the urban environment and insulin resistance in a cohort of adults in Southern India. The association was robust using various matrices of urbanization and adjustment for individual predictors. Our results are of public health concern due to the movement of large numbers of people from rural to urban areas in many parts of the world and the already large burden of diabetes. Further research is needed including longitudinal follow-up, to assess the aspects within the urban environment that may be most important to the association with HOMA-IR in this cohort.
Abbreviations
- BMI:
-
body mass index
- CVD:
-
cardiovascular disease
- FBS:
-
fasting blood sugar
- GPS:
-
Global Position System
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- IQR:
-
interquartile range
- OR:
-
odds ratio
- PM2.5 :
-
particulate matter less than 2.5 μm in aerodynamic diameter
- PURSE-HIS:
-
Population Study of Urban, Rural, and Semi-urban Regions for the Detection of Endovascular Disease and Prevalence of Risk Factors and Holistic Intervention Study
- SE score:
-
socioeconomic score
- WC:
-
waist circumference
References
United Nations. World urbanization prospects: the 2014 revision (highlights). New York: United Nations Department of Economic and Social, 2014; Contract No.: ESA/P/WP/224.
Jayawardena R, Ranasinghe P, Byrne NM, Soares MJ, Katulanda P, Hills AP. Prevalence and trends of the diabetes epidemic in South Asia: a systematic review and meta-analysis. BMC Public Health. 2012;12:380.
Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: indian scenario. Indian J Med Res. 2007;125(3):217–30.
Ramachandran A, Mary S, Yamuna A, Murugesan N, Snehalatha C. High prevalence of diabetes and cardiovascular risk factors associated with urbanization in India. Diabetes Care. 2008;31(5):893–8.
Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54(12):3022–7.
Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746–53.
Vlahov D, Galea S. Urbanization, urbanicity, and health. J Urban Health. 2002;79(4 Suppl 1):S1–12.
Ebrahim S, Kinra S, Bowen L, Andersen E, Ben-Shlomo Y, Lyngdoh T, et al. The effect of rural-to-urban migration on obesity and diabetes in india: a cross-sectional study. PLOS Med. 2010;7(4):e1000268.
Maiti S, Agrawal P. Environmental degradation in the context of growing urbanization: a focus on the metropolitan cities of India. J Hum Ecol. 2005;17(4):277–87.
Balti EV, Echouffo-Tcheugui JB, Yako YY, Kengne AP. Air pollution and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2014;106(2):161–72.
Lee YM, Jacobs DR Jr, Lee DH. Persistent organic pollutants and type 2 diabetes: a critical review of review articles. Front Endocrinol. 2018;9:712.
Deepa M, Grace M, Binukumar B, Pradeepa R, Roopa S, Khan HM, et al. High burden of prediabetes and diabetes in three large cities in South Asia: the Center for cArdio-metabolic Risk Reduction in South Asia (CARRS) Study. Diabetes Res Clin Pract. 2015;110(2):172–82.
Ramachandran A, Snehalatha C, Vijay V. Temporal changes in prevalence of type 2 diabetes and impaired glucose tolerance in urban southern India. Diabetes Res Clin Pract. 2002;58(1):55–60.
Gujral UP, Narayan KM, Pradeepa RG, Deepa M, Ali MK, Anjana RM, et al. Comparing type 2 diabetes, prediabetes, and their associated risk factors in Asian Indians in India and in the U.S.: the CARRS and MASALA studies. Diabetes Care. 2015;38(7):1312–8.
Reaven GM. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595–607.
Lim S, Cho YM, Park KS, Lee HK. Persistent organic pollutants, mitochondrial dysfunction, and metabolic syndrome. Ann N Y Acad Sci. 2010;1201:166–76.
Polyzos SA, Kountouras J, Deretzi G, Zavos C, Mantzoros CS. The emerging role of endocrine disruptors in pathogenesis of insulin resistance: a concept implicating nonalcoholic fatty liver disease. Curr Mol Med. 2012;12(1):68–82.
Hectors TL, Vanparys C, Van Gaal LF, Jorens PG, Covaci A, Blust R. Insulin resistance and environmental pollutants: experimental evidence and future perspectives. Environ Health Perspect. 2013;121(11–12):1273–81.
Xu X, Liu C, Xu Z, Tzan K, Zhong M, Wang A, et al. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue. Toxicol Sci. 2011;124(1):88–98.
Chen Z, Salam MT, Toledo-Corral C, Watanabe RM, Xiang AH, Buchanan TA, et al. Ambient air pollutants have adverse effects on insulin and glucose homeostasis in Mexican Americans. Diabetes Care. 2016;39(4):547–54.
Thiering E, Markevych I, Bruske I, Fuertes E, Kratzsch J, Sugiri D, et al. Associations of residential long-term air pollution exposures and satellite-derived greenness with insulin resistance in German adolescents. Environ Health Perspect. 2016;124(8):1291–8.
Thanikachalam S, Harivanzan V, Mahadevan MV, Murthy JS, Anbarasi C, Saravanababu CS, et al. Population study of urban, rural, and semiurban regions for the detection of endovascular disease and prevalence of risk factors and holistic intervention study: rationale, study design, and baseline characteristics of PURSE-HIS. Global Heart. 2015;10(4):281–9.
World Health Organization. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance. 2005.
Chaturvedi SK. Presumptive stressful life event scale. Indian J Psychiatry. 1985;27(1):103.
Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy’s socioeconomic status scale-updating for 2007. Indian J Pediatr. 2007;74(12):1131–2.
Mishra D, Singh HP. Kuppuswamy’s socioeconomic status scale—a revision. Indian J Pediatr. 2003;70(3):273–4.
Schatzkin A, Kipnis V, Carroll RJ, Midthune D, Subar AF, Bingham S, et al. A comparison of a food frequency questionnaire with a 24-hour recall for use in an epidemiological cohort study: results from the biomarker-based Observing Protein and Energy Nutrition (OPEN) study. Int J Epidemiol. 2003;32(6):1054–62.
Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27(6):1487–95.
USGS. Land Cover Type Yearly L3 Global 500 m SIN Grid Sioux Falls, South Dakota: USGS Earth Resources Observation and Science (EROS) Center; 2010 [updated 01/19/2016]. https://lpdaac.usgs.gov.
Poulter B, Ciais P, Hodson E, Lischke H, Maignan F, Plummer S, et al. Plant functional type mapping for earth system models. Geosci Model Dev. 2011;4(4):993–1010.
Ministry of Home Affairs. Provisional population totals urban agglomerations and cities, Census of India 2011 (Data Highlights). Government of India, 2011.
Muoio DM, Newgard CB. Mechanisms of disease: molecular and metabolic mechanisms of insulin resistance and beta-cell failure in type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9(3):193–205.
Marx J. Unraveling the causes of diabetes. Science (New York, NY). 2002;296(5568):686–9.
Wilkin TJ, Murphy MJ. The gender insulin hypothesis: why girls are born lighter than boys, and the implications for insulin resistance. Int J Obes. 2006;30(7):1056–61.
Sinaiko AR, Jacobs DR Jr, Steinberger J, Moran A, Luepker R, Rocchini AP, et al. Insulin resistance syndrome in childhood: associations of the euglycemic insulin clamp and fasting insulin with fatness and other risk factors. J Pediatr. 2001;139(5):700–7.
Allard P, Delvin EE, Paradis G, Hanley JA, O’Loughlin J, Lavallee C, et al. Distribution of fasting plasma insulin, free fatty acids, and glucose concentrations and of homeostasis model assessment of insulin resistance in a representative sample of Quebec children and adolescents. Clin Chem. 2003;49(4):644–9.
Moran A, Jacobs DR Jr, Steinberger J, Hong CP, Prineas R, Luepker R, et al. Insulin resistance during puberty: results from clamp studies in 357 children. Diabetes. 1999;48(10):2039–44.
DECODE study group. Age- and sex-specific prevalences of diabetes and impaired glucose regulation in 13 European cohorts. Diabetes Care. 2003;26(1):61–9.
Tahapary DL, de Ruiter K, Kurniawan F, Djuardi Y, Wang Y, Nurdin SME, et al. Impact of rural-urban environment on metabolic profile and response to a 5-day high-fat diet. Sci Rep. 2018;8(1):8149.
Meeks KAC, Stronks K, Adeyemo A, Addo J, Bahendeka S, Beune E, et al. Peripheral insulin resistance rather than beta cell dysfunction accounts for geographical differences in impaired fasting blood glucose among sub-Saharan African individuals: findings from the RODAM study. Diabetologia. 2017;60(5):854–64.
Gordon T, Balakrishnan K, Dey S, Rajagopalan S, Thornburg J, Thurston G, et al. Air pollution health research priorities for India: perspectives of the Indo-U.S. Communities of researchers. Environ Int. 2018;119:100–8.
Eze IC, Hemkens LG, Bucher HC, Hoffmann B, Schindler C, Kunzli N, et al. Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect. 2015;123(5):381–9.
Thiering E, Cyrys J, Kratzsch J, Meisinger C, Hoffmann B, Berdel D, et al. Long-term exposure to traffic-related air pollution and insulin resistance in children: results from the GINIplus and LISAplus birth cohorts. Diabetologia. 2013;56(8):1696–704.
Lee DH, Porta M, Jacobs DR Jr, Vandenberg LN. Chlorinated persistent organic pollutants, obesity, and type 2 diabetes. Endocr Rev. 2014;35(4):557–601.
Rao KD, Shahrawat R, Bhatnagar A. Composition and distribution of the health workforce in India: estimates based on data from the National Sample Survey. WHO South-East Asia J Public Health. 2016;5(2):133–40.
Minocha S, Thomas T, Kurpad AV. Are ‘fruits and vegetables’ intake really what they seem in India? Eur J Clin Nutr. 2018;72(4):603–8.
Bowen L, Ebrahim S, De Stavola B, Ness A, Kinra S, Bharathi AV, et al. Dietary intake and rural-urban migration in India: a cross-sectional study. PLoS ONE. 2011;6(6):e14822.
Authors’ contributions
MT is a co-investigator on the project, directed the study and data analysis, and wrote text for the manuscript; CF assisted with interpretation of the analyses and contributed to the manuscript; KL assisted with interpretation of the analyses, created figures and contributed to the manuscript; JS conducted the data analyses; HV conducted the data analyses; DB contributed to the manuscript and interpretation; ST is the principal investigator of the PURSE-HIS and directed the study. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Please contact the corresponding author for data requests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All participants provided informed written consent. The study was approved by the Institutional Ethics Committee (IEC-06/53/47) at Sri Ramachandra University, Chennai, India, and was registered with the Clinical Trials Registry, India (CTRI/2011/04/001677).
Funding
The PURSE-HIS is funded by a Grant from the Drugs and Pharmaceutical Research Program under Technology Development and Transfer Division, Department of Science and Technology, Government of India (Project No. VI-D&P/151/06-07/TDT), MT and KL were supported by Public Health Institute and DB was supported by NIEHS (ES026980 and ES015462).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1.
Association between distance to urban center and HOMA-IR level comparing the inclusion of either of two measures of adiposity: body mass index (BMI) or waist circumference.
Additional file 2.
Effect modification of the relationship between distance to urban center and HOMA-IR.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Thanikachalam, M., Fuller, C.H., Lane, K.J. et al. Urban environment as an independent predictor of insulin resistance in a South Asian population. Int J Health Geogr 18, 5 (2019). https://doi.org/10.1186/s12942-019-0169-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12942-019-0169-9