Abstract
Background
Delayed epidural hematoma (DEH) following evacuation of traumatic acute subdural hematoma (ASDH) or acute epidural hematoma (EDH) is a rare but devastating complication, especially when it occurs sequentially in a single patient.
Case presentation
A 19-year-old man who developed contralateral DEH following craniotomy for evacuation of a traumatic right-side ASDH and then developed a left-side DEH of the posterior cranial fossa after craniotomy for evacuation of the contralateral DEH. He was immediately returned to the operating room for additional surgeries and his neurological outcome was satisfactory.
Conclusions
Although DEH occurring after evacuation of ASDH or acute EDH is a rare event, timely recognition is critical to prognosis.
Similar content being viewed by others
Background
Although delayed epidural hematoma (DEH) is an uncommon complication following evacuation of intracranial hematomas, it is devastating nevertheless, especially following the evacuation of traumatic acute subdural hematoma (ASDH). A previous study reported the incidence of delayed postoperative epidural hematoma (EDH) to be 1.0% [1]. A total of 38 cases of such DEH were found in literature (Table 1). We report a case involving a Chinese man who developed contralateral DEH following decompressive surgery for right-side ASDH, and then developed an additional remote DEH following decompressive surgery for the contralateral DEH.
Case presentation
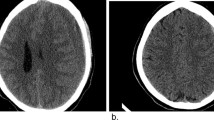
A 19-year-old Chinese man involved in a motor vehicle accident was admitted to the emergency department presenting with a Glasgow Coma Scale (GCS) of 3 and right eye mydriasis. A computed tomography (CT) scan of his brain revealed right-side ASDH and a midline shift of 14.5 mm with severe brain swelling (Figs. 1 and 3). He was hemodynamically stable, with no clotting dysfunction according laboratory tests. He was subsequently transferred to the operating room and underwent a right decompressive craniectomy. The ASDH was caused by a ruptured lateral fissure vein. The brain exhibited slowly progressing swelling after the hematoma and inactivated brain tissue were evacuated. Consequently, immediate augmentation duraplasty using artificial dura mater was performed. On examination, the patient exhibited bilateral mydriasis. Given the slowly progressing brain swelling, this was possibly due to delayed contralateral ASDH or EDH. A CT scan of the brain was performed immediately thereafter, which revealed the emergence of contralateral DEH (Fig. 2). Owing to a mass effect from the DEH and severe brain swelling, the patient was immediately taken to the operating room to undergo a left hematoma evacuation and decompressive craniectomy. During surgery, it was determined that the DEH was caused by the rupture of the middle meningeal artery branch, with temporal and occipital bone fractures (Fig. 3a). Following surgery, the patient was transferred to the neurological intensive care unit, where the left and right pupil sizes were measured to be 2.0 mm and 5.0 mm, respectively.
On postoperative day 1, approximately 5 h after the second surgery, the primary nurse found that the size of the patient’s left pupil gradually increased from 2.0 mm to 3.5 mm. An immediate brain CT scan revealed evidence of left-side DEH of the posterior cranial fossa (Fig. 4). Owing to mass effect of the DEH, a third surgery was offered. He underwent left posterior cranial fossa hematoma evacuation and decompressive craniectomy. During the third surgery, it was determined that the DEH was caused by a ruptured transverse sinus. A brain CT following the third surgery was performed (Fig. 5). The patient recovered to a GCS of 7 within 40 days after surgery, and was transferred to the rehabilitation hospital. He was ultimately discharged from the rehabilitation hospital with a Glasgow Outcome Score of 4. He underwent cranioplasty 1 year later and has since recovered well.
Discussion and conclusion
Traumatic brain injury (TBI) is the leading cause of morbidity and mortality in adults in highly developed countries, with the highest incidence in men aged 15–24 years [2]. Approximately one-third of patients with severe TBI are diagnosed with ASDH [3]. According to the guidelines for severe TBIs, ASDH causing brain herniation should be immediately evacuated with or without bone flap removal and duraplasty [4]. DEH following decompressive surgery for ASDH or acute EDH is an extremely uncommon occurrence, with only dozens of cases in the medical literature published in English (Table 1); nevertheless, it is a devastating complication [5,6,7,8]. To our knowledge, our report is the first to document two occurrences of DEH in different areas following decompressive craniectomy for traumatic ASDH in a single patient, who developed DEH sequentially following decompressive surgery for ASDH and DEH.
There were some signs that alerted us to the possibility of DEH following evacuation of the ASDH or acute EDH, including a skull fracture, intraoperative brain swelling, pupillary dilation, an unmanageable elevated intracranial pressure (ICP) [9], a large volume of intraoperative blood loss, long duration of craniotomy, and a large craniotomy area [10]. During the first surgery in this case, the brain exhibited slowly progressing swelling, with bilateral mydriasis after the hematoma and inactivated brain tissue were evacuated. A subsequent CT scan revealed a large contralateral DEH. On postoperative day 1 after the second surgery, the size of the patient’s left pupil gradually increased from 2.0 mm to 3.5 mm, with a CT scan revealing a large posterior fossa DEH. When these alarm signs presented, we need an immediate brain CT scan to exclude remote DEH.
There are many explanations for the pathogenesis of DEH following evacuation of ASDH or acute EDH, including loss of tamponade effect, abnormal vasomotor mechanisms, and acute coagulopathy [11]. The main cause, however, appears to be a disruption of the equilibrium in damaged vessels and reactive intracranial hypertension [12]. Sources of bleeding include a ruptured meningeal arterial branch or a skull fracture [13, 14]. We believe that the primary mechanism of DEH in this case was the loss of the tamponade effect with the rupture of the meningeal arterial branch and transverse sinus, and skull fractures. Thus, if there is a possibility of remote DEH after surgery, a CT scan of the brain is necessary. In this case, the brain exhibited slowly progressive swelling during the first surgery with the left temporal and occipital bone fractures, a postoperative brain CT would been taken immediately to exclude the possibility of delayed hematoma; meanwhile, the patient’s family were struggling financially, and the imported ICP monitor was cost prohibitive. Consequently, an ICP monitor was not implanted. But if it was feasible, implantation of a continuous ICP monitor during the first surgery would have helped us to recognize the DEH in a timely manner [15].
This case suggests that DEH following craniotomy for evacuation of traumatic ASDH or acute EDH should always be considered a possibility, especially in cases of intra-operative brain swelling and skull fractures, even though CT may provide no evidence of remote skull fractures. Cautious observation and early postoperative radiological evaluation may facilitate timely recognition of these remote DEHs and contribute to improved patient outcomes.
Abbreviations
- ASDH:
-
Acute subdural hematoma
- CT:
-
Computed tomography
- DEH:
-
Delayed epidural hematoma
- EDH:
-
Epidural hematoma
- GCS:
-
Glasgow coma scale
- GOS:
-
Glasgow outcome scale
- ICP:
-
intracranial pressure
- TBI:
-
Traumatic brain injury
References
Fukamachi A, Koizumi H, Nagaseki Y, Nukui H. Postoperative extradural hematomas: computed tomographic survey of 1105 intracranial operations. Neurosurgery. 1986;19(4):589–93.
Shumskaya E, Andriessen TM, Norris DG, Vos PE. Abnormal whole-brain functional networks in homogeneous acute mild traumatic brain injury. Neurology. 2012;79(2):175–82.
Vilcinis R, Bunevicius A, Tamasauskas A. The association of surgical method with outcomes of acute subdural hematoma patients: experience with 643 consecutive patients. World Neurosurg. 2017;
Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, Bratton SL, Chesnut R, Harris OA, Kissoon N, et al. Guidelines for the Management of Severe Traumatic Brain Injury, fourth edition. Neurosurgery. 2016;
Saberi H, Meybodi AT, Meybodi KT, Habibi Z, Mirsadeghi SM. Delayed post-operative contralateral epidural hematoma in a patient with right-sided acute subdural hematoma: a case report. Cases J. 2009;2:6282.
Tomycz ND, Germanwala AV, Walter KA. Contralateral acute subdural hematoma after surgical evacuation of acute subdural hematoma. J Trauma. 2010;68(1):E11–2.
Takeuchi S, Takasato Y. Contralateral acute subdural hematoma after surgical evacuation of the initial hematoma: two case reports and review of the literature. Turk Neurosurg. 2013;23(2):294–7.
Solomiichuk VO, Drizhdov KI. Contralateral delayed epidural hematoma following intracerebral hematoma surgery. Surg Neurol Int. 2013;4:134.
TM S, Lee TH, Chen WF, Lee TC, Cheng CH. Contralateral acute epidural hematoma after decompressive surgery of acute subdural hematoma: clinical features and outcome. J Trauma. 2008;65(6):1298–302.
Kim SH, Lee JH, Joo W, Chough CK, Park HK, Lee KJ, Rha HK. Analysis of the risk factors for development of post-operative extradural hematoma after intracranial surgery. Br J Neurosurg. 2015;29(2):243–8.
Mohindra S, Mukherjee KK, Gupta R, Chhabra R, Gupta SK, Khosla VK. Decompressive surgery for acute subdural haematoma leading to contralateral extradural haematoma: a report of two cases and review of literature. Br J Neurosurg. 2005;19(6):490–4.
Lesoin F, Viaud C, Pruvo J, Redford H, Jomin M. Traumatic and alternating delayed intracranial hematomas. Neuroradiology. 1984;26(6):515–6.
Boviatsis EJ, Korfias S, Kouyialis AT, Sakas DE. Epidural haematoma after evacuation of contralateral subdural haematoma. Ir J Med Sci. 2004;173(4):217–8.
Talbott JF, Gean A, Yuh EL, Stiver SI. Calvarial fracture patterns on CT imaging predict risk of a delayed epidural hematoma following decompressive craniectomy for traumatic brain injury. AJNR Am J Neuroradiol. 2014;35(10):1930–5.
Meguins LC, Sampaio GB, Abib EC, Adry RA, Ellakkis RF, Ribeiro FW, Maset AL, de Morais DF. Contralateral extradural hematoma following decompressive craniectomy for acute subdural hematoma (the value of intracranial pressure monitoring): a case report. J Med Case Rep. 2014;8:153.
GZ X, Wang MD, Liu KG, Bai YA. A rare remote epidural hematoma secondary to decompressive craniectomy. J Craniofac Surg. 2014;25(1):e17–9.
Nadig AS, King AT. Traumatic extradural haematoma revealed after contralateral decompressive craniectomy. Br J Neurosurg. 2012;26(6):877–9.
Shen J, Pan JW, Fan ZX, Zhou YQ, Chen Z, Zhan RY. Surgery for contralateral acute epidural hematoma following acute subdural hematoma evacuation: five new cases and a short literature review. Acta Neurochir. 2013;155(2):335–41.
Cohen JE, Rajz G, Itshayek E, Umansky F. Bilateral acute epidural hematoma after evacuation of acute subdural hematoma: brain shift and the dynamics of extraaxial collections. Neurol Res. 2004;26(7):763–6.
Matsuno A, Katayama H, Wada H, Morikawa K, Tanaka K, Tanaka H, Murakami M, Fuke N, Nagashima T. Significance of consecutive bilateral surgeries for patients with acute subdural hematoma who develop contralateral acute epi- or subdural hematoma. Surg Neurol. 2003;60(1):23–30. discussion 30
Feuerman T, Wackym PA, Gade GF, Lanman T, Becker D. Intraoperative development of contralateral epidural hematoma during evacuation of traumatic extraaxial hematoma. Neurosurgery. 1988;23(4):480–4.
Meguro K, Kobayashi E, Maki Y. Acute brain swelling during evacuation of subdural hematoma caused by delayed contralateral extradural hematoma: report of two cases. Neurosurgery. 1987;20(2):326–8.
Borovich B, Braun J, Guilburd JN, Zaaroor M, Michich M, Levy L, Lemberger A, Grushkiewicz I, Feinsod M, Schachter I. Delayed onset of traumatic extradural hematoma. J Neurosurg. 1985;63(1):30–4.
Piepmeier JM, Wagner FC Jr. Delayed post-traumatic extracerebral hematomas. J Trauma. 1982;22(6):455–60.
Acknowledgements
Not applicable.
Funding
No funding.
Availability of data and materials
All patient data and clinical approaches adopted are contained in the medical files of The Third Affiliated Hospital of Soochow University. The bibliographic data of reference are available on PubMed and the conclusions are based on the opinion of the expert involved in this case. The data supporting the conclusions of this article are included within the article and its figures.
Author information
Authors and Affiliations
Contributions
All authors participated in the management of the patient in this case report. JS and JC collected patient data. RW performed literature review and drafted the manuscript. BD and YM revised the paper and gave the final approval of the definitive version of the article. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient’s father for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wu, R., Shi, J., Cao, J. et al. Two occurrences of delayed epidural hematoma in different areas following decompressive craniectomy for acute subdural hematoma in a single patient: a case report. BMC Surg 17, 123 (2017). https://doi.org/10.1186/s12893-017-0303-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-017-0303-1