Abstract
Background
Majority of musculoskeletal cross-sectional imaging requests have a non-revealing and non-specific clinical history of pain. However, the location of pain is very relevant towards arriving at a specific orthopedic diagnosis. The purpose of this research was to study the impact of skin marker placement and training of technologists prior to knee MRI in detection of clinically important findings.
Methods
Total 200 consecutive left knee MRIs were evaluated before and after technologist training with regards to marker placement at the site of clinical symptoms or palpable finding. Marker location in relation to the knee was recorded and important findings were classified as correlated important finding, non-correlated important finding, other compartment important finding in non-correlated cases, and diffuse abnormality, i.e. tri-compartmental cartilage defects in both correlated and non-correlated cases. Differences among scans before and after technologist training were analyzed.
Results
The marker placement was observed in higher proportion of patients in post-training scans (78% vs 60%, p = 0.00). The most common location of the marker was in anterior or anterolateral knee (32% and 34% cases, respectively). The marker-important finding correlation was also higher post training, but not statistically significant (53% versus 38%, p = 0.57). Important findings correlated with the marker in more than 50% of the scans in the post-training set.
Conclusion
Marker placement can aid in detection of clinically important imaging finding and technologist training aids in increased rates of marker placement and improved correlation.
Similar content being viewed by others
Background
In our tertiary care practice, majority of orthopedic cross-sectional study orders have a non-revealing and non-specific (in terms of location) history of pain. However, it is well known that site of pain e.g. joint line tenderness is quiet relevant in arriving at diagnosis of orthopaedic conditions, such as meniscus tear [1, 2]. Similarly, many joint diagnoses based on history and examinations reflect the site of patient’s symptoms. Musculoskeletal radiologists reading these joint MRIs and particularly those using a structured reporting template find many related and unrelated findings with respect to the patient’s presentation. The radiologist may not have access to the patient’s chart during study readout or even with chart access, extracting relevant history and examination takes time and reduces the efficiency of the radiologist in busy practice environments.
In majority of radiology practices, the radiologist often does not see the patient, and the only point of contact for the patient is the technologist. The practice of communicating patient’s clinical information from the technologist to the radiologist vary from onsite documentation of patient history in the chart, attaching the referring physician’s note to the patient images, to direct site marking by the technologist before the examination. The musculoskeletal department at our institution adopted the policy of onsite marker placement at the site of concern, i.e. “most painful or only painful site” and/or palpable swelling. The purpose of this study was:
-
1.
To evaluate the correlation of skin marker placement by the technologist to an important clinical finding, and
-
2.
Study the impact of re-training of technologists on frequency of marker placement and correlation of marker site post-training with the underlying pathology.
Methods
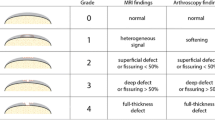
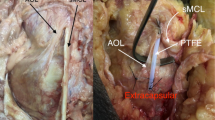
Institutional board review approved retrospective study was performed and informed consent was waived for this HIPAA compliant quality improvement (QI) project. 200 consecutive knee MRIs in patients were evaluated in two groups - before and after technologist training with regards to skin marker (MR-SPOT, 5.0 cm, Beekley Medical Corporation, Fig. 1) placement before the Knee MRI. Both pre-and post-training groups encompassed 100 scans each. Only left knee MRIs were included in the study to maintain consistency. The MRIs were evaluated for the frequency of marker placement by a musculoskeletal radiology fellow. The marker location in relation to the knee was categorized as: anterior, posterior, anterolateral, anteromedial, medial and lateral. The important imaging findings evaluated included: medial or lateral meniscus tear, medial or lateral collateral ligament tear, anterior or posterior cruciate ligament tear, high grade or full-thickness cartilage defects and moderate-large effusion. Patient demographics, presenting complaint and post-imaging treatment were also recorded. The imaging findings were classified as follows:
-
corroborative and important, i.e. finding correlated with location of the skin marker. e.g. a medial meniscus tear in the setting of a medial marker.
-
non-corroborative important, i.e. finding did not correlate with location of the skin marker, e.g. a lateral meniscus tear in the setting of a medial marker.
-
other compartment important finding in corroborative cases, i.e. lateral and medial meniscus tears in a medial marker.
-
diffuse abnormality, i.e. tricompartmental cartilage defects in both corroborative and –non-corroborative cases.
Differences among scans before and after the technologist training were assessed using chi-square test for categorical variables and t-test for continuous variables.
Results
The results are summarized in Table 1. The patient demographics in both groups of scans were not statistically different (age p = 0.2 and sex p = 0.3). Chief complaint in majority of patients in both groups was non-specific pain (75% in pre-training group, 83% in post-training group, p = 0.16). Marker was observed in higher number of scans in the post training group (78% vs 60%, p = 0.00). Most common location of the marker was in anterior or anterolateral sites (32% and 34% cases, respectively). Corroborative and important findings were found to be higher, but not statistically different, in the post-training group (53% vs 38%; p = 0.57) (Figs. 2, 3 and 4). However, diffuse abnormalities were more prevalent in post-training group (31% vs 14%, p = 0.04), which may partially explain the statistical non-significance. Other associated findings in pre- and post-training groups (14% vs 13%) included medial meniscus tears (3 vs 7), lateral meniscus tears (3 vs 2), ACL tears (5 vs 1), MCL tear (1 vs 0), PCL tear (0 vs 1), and other compartment arthritis (2 vs 1). Majority of patients received conservative management (90%).
Discussion
MRI-compatible skin markers have been used as a preoperative guidance tool for neurosurgeons in brain and spinal surgeries [3]. Fischer et al. described use of a special skin marker and inserted a nonmagnetic wire into the breast to achieve MRI-guided localization of suspected breast lesions. Repeat diagnostic MRI was performed to document the position of the wire tip relative to the lesion, to allow successful excision [4]. Besides commercially available markers, fish oil capsules have been used as MRI localization devices as a cost-effective alternative [5]. However, pre-scan application of skin marker in musculoskeletal settings has not been scientifically studied yet.
The present study shows that skin marker location highly correlates with important clinical findings, i.e. in upto 53% cases and thus, placement before knee MRI can potentially help the radiologist in producing clinically relevant reports. In routine reading of high volume of knee MRI studies and using structured template reporting, one may detect a number of imaging findings which could be unrelated to the patient’s symptoms, and may divert the attention of the radiologist from the area of interest. The clinical indication presented to the radiologist for joint MRI is usually non-specific (non-localizing) pain, as observed in the majority of cases in present study as well. Since there is limited clinical information available to the radiologist, skin markers can help in identification of pathology with increased confidence. Finding clinically correlated important internal knee derangement lesions in more than 50% cases by just using an external marker is a diagnostically relevant result. It should also be noted that in 47% cases, there were other findings, such as cruciate ligament injuries and non-correlated other compartment derangements. Therefore, comprehensive evaluation is still warranted during knee MRI reporting. However, the marker placement may help the radiologist rank the impressions more relevant to the clinical scenario and presentation.
Our study also shows that training of the technologists in application of knee markers at the area of interest, i.e. point of maximum pain or swelling, increases the frequency of marker placement. This cements the fact that, indirectly, active intervention of radiologist can keep up the interest of the technologists in quality improvement of imaging. Furthermore, the correlation of marker-important finding is also improved with technologist training and they become better at marking the clinically important site of abnormality.
We also found important imaging finding in 13–14% cases unrelated to the marked site. Therefore, although marking seems important and correlated finding should be put as the first impression, interrogation of all compartments of the joint remains essential.
There are some limitations to our study. First, this was a retrospective study and not a prospectively derived cohort. Second, we did not obtain inter-observer performance since formal reports were available for all the studies and this is the 1st exploratory study in this domain.
In future, similar studies in other joints, such as wrist, ankle, shoulder and hip could be performed to further validate the usefulness of marker placement. Time of imaging evaluation can be assessed with and without marker in detection of clinically important finding. A similar concept can be expanded to other imaging modalities, such as abdominal CTs, which are performed on a large scale, especially on call. It might help the reader to detect the important imaging finding quickly and consistently.
Conclusion
Skin marker placement can aid in detection of clinically important imaging finding and technologist training aids in increased rates of marker placement and improved correlation. Therefore, marker placement can potentially improve the clinical relevance of knee MRI reports.
Abbreviations
- MRI:
-
Magnetic Resonance Imaging
- QI:
-
Quality Improvement
References
Eren OT. The accuracy of joint line tenderness by physical examination in the diagnosis of meniscal tears. Arthroscopy. 2003;19(8):850–4.
Hing W, White S, Reid D, Marshall R. Validity of the McMurray's test and modified versions of the test: a systematic literature review. J Man Manip Ther. 2009;17(1):22–35.
Rosahl SK, Gharabaghi A, Liebig T, Feste CD, Tatagiba M, Samii M. Skin markers for surgical planning for intradural lesions of the thoracic spine. Technical note. Surg Neurol. 2002;58(5):346–8.
Fischer U, Vosshenrich R, Bruhn H, Keating D, Raab BW, Oestmann JW. MR-guided localization of suspected breast lesions detected exclusively by postcontrast MRI. J Comput Assist Tomogr. 1995;19(1):63–6.
Gilbert JW, Wheeler GR, Richardson GB, Herder SL, Mick GE, Gyarteng-Dakwa K, et al. Guidance of magnetic resonance imaging and placement of skin-marker localization devices. J Neurosurg Sci. 2011;55(2):85–8.
Acknowledgements
None
Funding
No funding was obtained for this study.
Availability of data and materials
Data is available upon request via email.
Disclosures
Avneesh Chhabra serves as a consultant with Siemens for MSK CAD group and ICON medical. He also receives royalties from Jaypee and Wolters Kluwer.
All authors report no conflict of interest.
Author information
Authors and Affiliations
Contributions
VW: study concepts and design, literature search, manuscript preparation. EW: study concepts and design, manuscript preparation. DH: study concepts and design, manuscript editing. YX: statistical analysis, manuscript editing. AC: guarantor of integrity of the entire study, study concepts and design, manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board of UT Southwestern approved this for this HIPAA compliant quality improvement (QI) project and informed consent was waived due to its retrospective nature.
Consent for publication
Not Applicable
Competing interests
Dr. Avneesh Chhabra and Dr. Daichi Hayashi serve as members of editorial board of BMC Musculoskeletal Disorders.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wadhwa, V., Weissman, E., Hayashi, D. et al. Skin marker placement by technologist prior to knee MRI helps identify clinically relevant pathologies. BMC Musculoskelet Disord 18, 530 (2017). https://doi.org/10.1186/s12891-017-1876-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-017-1876-7