Abstract
Background
Hyaline cartilage calcification (CC) is associated with osteoarthritis (OA) in hip and knee joints. The first metatarsophalangeal joint (1stMTPJ) is frequently affected by OA, but it is unclear if CC occurs in the 1stMTPJ. The aim of the present study was to analyze the prevalence of CC of the 1stMTPJ in the general population by high-resolution digital contact radiography (DCR) and to determine its association with histological OA severity, age and body mass index (BMI).
Methods
168 metatarsal heads of 84 donors (n = 47 male, n = 37 female; mean age 62.73 years, SD ±18.8, range 20–93) were analyzed by DCR for the presence of CC. Histological OA grade (hOA) by OARSI was analyzed in the central load-bearing zone of the first metatarsal head (1st MH). Structural equation modeling (SEM) was performed to analyze the interrelationship between CC, hOA, age and BMI.
Results
The prevalence of CC of 1stMH was 48.8 % (41/84) (95 %-CI [37.7 %, 60.0 %]), independent of the affected side (p = 0.42), gender (p = 0.41) and BMI (p = 0.51). The mean amount of CC of one MH correlated significantly with that of the contralateral side (rs = 0.4, 95 %-CI [0.26, 0.52], p < 0.001). The mean amount of CC (in % of total cartilage area) of the MH correlated significantly with the severity of hOA (rs = 0.51, 95 %-CI [0.32, 0.65], p < 0.001). SEM revealed significant associations between CC and hOA (r = 0.74, p < 0.001) and between hOA and age (β = 0.62, p = 0.001), but not between CC and age (p = 0.15). There was no significant influence of BMI on either CC (p = 0.37) or hOA (p = 0.16).
Conclusion
The observation that CC of the 1stMH is significantly associated with the severity of OA but independent of age and BMI, suggests an intimate relationship between CC and the pathogenesis of OA, the exact nature of which will have to be explored by future studies.
Similar content being viewed by others
Background
Foot pain is a frequent clinical concern. One reason for foot pain is osteoarthritis (OA) [1–3], in particular of the first metatarsophalangeal joint (1st MTPJ) [4, 5]. The prevalence of radiographic OA of the 1st MTPJ in middle-aged and older adults in the general population has been described to vary between 12 and 42.4 % [6–8]. Although there are risk factors for OA of the 1st MTPJ, namely anatomic variations [4, 9–11], altered biomechanics [4, 12, 13], trauma [14–16] and metabolic or chronic inflammatory disorders such as rheumatoid arthritis and gout [17, 18], until today, the etiology of OA of the 1st MTPJ remains unknown in the majority of cases.
Tissue calcification in humans is a complex but incompletely understood process and occurs exclusively in hard tissues (bone, growth plate, teeth) under physiological conditions [19]. Any deposition of mineral calcium-phosphate compounds outside these hard tissues is considered to be a pathological process and is called ectopic calcification [20]. The calcification of articular cartilage is also known as chondrocalcinosis [21].
The visualization of articular cartilage calcification is technically difficult and the sensitivity of detection strongly depends on the applied imaging method [22, 23]. Until today, published data of joint calcification at various sites (knee, hip, hand, wrist and symphysis pubis) [24–30] is mostly based on low-resolution imaging techniques, i.e. standard X-ray, CT or MRI. The detection of hyaline cartilage calcification with these methods is insufficient for the visualization of small initial calcification stages [31–33]. The reported prevalence of articular cartilage calcification in the literature is almost exclusively based on plain radiographs and therefore is likely to underestimate the real prevalence [34, 35]. The most sensitive method to detect cartilage calcification is digital contact radiography (DCR) [23]. Work from our group has previously demonstrated deposition of cartilage calcification in 100 % of severely osteoarthritic hip and knee joints [22, 31]. Since in these studies there was a significant correlation between the amount of cartilage calcification and the clinical severity of hip and knee OA [22, 31], the clinical relevance of cartilage calcification in OA appears to be evident. Nonetheless, the relationship between cartilage calcification and OA is not fully understood, nor is the interrelationship between age, OA and cartilage calcification. In particular, it remains unclear whether cartilage calcification represents a simple epiphenomenon of ageing or whether there is a causal relationship between cartilage calcification and OA [36].
Regarding the 1st MTPJ, only periarticular but not intra-articular calcification has been visualized and described so far [37–39]. To the best of our knowledge, there is no data in the literature about calcification of the articular hyaline cartilage of the 1st MTPJ.
Here we analyzed for the first time the prevalence of articular cartilage calcification of the 1st MTPJ in a post-mortem cohort of the general population by DCR and examined the relationship between cartilage calcification and histological OA grade, age and BMI.
Methods
This cross-sectional study was approved by the local Ethics Committee of the Medical Association Hamburg, Germany (Ärztekammer Hamburg, PV: 4570) and was carried out according to existing rules and regulations of the University Medical Center Hamburg-Eppendorf. 168 first metatarsophalangeal joints (1st MTPJ) were obtained from 84 donors at the Department of Legal Medicine, University Medical Center Hamburg-Eppendorf. Only donors with intact metatarsophalangeal joints without any signs of disease other than OA were included in this study. Donors, which had evidence for previous surgical intervention or fractures of the metatarsophalangeal joint, or any rheumatic or oncologic disease were excluded from the study population.
Sample preparation
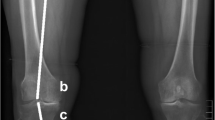
After removal of soft tissue a standardized 4 mm cartilage-bone slab was cut in the central axial plane from each metatarsal head (MH) (Additional file 1: Figure S1). To avoid potential contamination with sawing dust the slabs were cleaned in physiological saline solution and the residual bone debris was removed.
Digital contact radiography (DCR)
Standardized radiographs (25 kV, 3.8 mAs, film focus distance 8 cm) were taken from each cartilage-bone slab of the MH using a high-resolution digital radiography device (Faxitron X-Ray, Illinois, USA). In these radiographs, calcifications of the hyaline cartilage could be detected as radiopaque spots within the surrounding cartilage matrix. The mean amount of total cartilage calcification in % of total cartilage area for each MH was measured by image-analysis software (ImageJ 1.46, National Institutes of Health, Bethesda, USA) as described previously [22, 40].
Histological examination
Histological assessment was performed of the main load-bearing zone of each MH (central zone, directly adjacent to the central axial slab plane). A specimen of full thickness hyaline cartilage was cut to the subchondral bone plate of the load-bearing zone.
All specimens were fixed in 4 % PFA for 24 h, dehydrated in 80 % alcohol and embedded in paraffin. Four micrometer sections were cut and stained as shown in Additional file 2: Figure S2 with
-
1)
Safranin Orange (1 %) - to evaluate the histological OA grade according to the osteoarthritis cartilage histopathology assessment system (grade 0–6) (OARSI) [41].
-
2)
von Kossa (counterstained with Light Green) - to confirm the deposition of calcium-phosphate-crystals in the hyaline cartilage.
Statistical analysis
The biometric characteristics of donors are reported as mean values ± standard deviations (SD). For descriptive analysis, mean cartilage calcification values for each side were used. Fisher’s and McNemar’s exact test were used for categorical data. Spearman’s rank correlation coefficient was calculated to report associations between continuous variables. To analyze the correlation between the mean amount of cartilage calcification and histological degeneration grade, respectively age, the mean value of the left and right metatarsal head (MH) were calculated for each person. Structural equation modeling (SEM) [42] was used to investigate relationships between cartilage calcification, histological OA grade, age and BMI. The histological OA grade and cartilage calcification were included as latent variables, age and BMI as manifest variables. SEM accounts for intraclass correlation and allows to combine factor, multiple regression and covariance analysis simultaneously to describe interrelated relationships, as well as the representation of unobserved theoretical constructs (latent variables), while directly accounting for measurement error in the estimation [43]. Diagonally weighted least squares (DWLS) estimation was used. To assess model fit Chi-squared statistic and Root Mean Square Error of Approximation (RMSEA) was calculated. Cartilage calcification was transformed binary (0 = negative and 1 = positive DCR-detectable cartilage calcification of the 1st MH). All statistical analyses were performed with statistical software R (version 3.1.1) [44], and the package lavaan [45] and ggplot2 [46]. Regression coefficient β and correlation coefficient r were reported. A p-value less than 0.05 was considered statistically significant.
Results
In this study 168 metatarsal heads (MH) from 84 individual donors (n = 37 female and n = 47 male) were analyzed by DCR and histological assessment. The mean age was 62.7 years (SD ±18.8, range 20–93); 37 of the donors were female and 47 male. The distribution of gender and age by decade is shown in Additional file 3: Figure S3. The biometric characteristics of the study population are listed in Table 1.
Prevalence of cartilage calcification of the 1st MH analyzed by DCR
The prevalence of hyaline cartilage calcification of the 1st MH in the study population was 48.8 % (41 of 84 donors) (95 %-CI [37.7 %, 60.0 %]) (Table 2). The left joint was affected in 31.0 % (26/84) (95 %-CI [21.3 %, 42.0 %]) and the right joint in 36.9 % (31/84) (95 %-CI [26.6 %, 48.1 %]), no preference for cartilage calcification of one side could be detected (p = 0.42). Unilateral cartilage calcification was observed in 61.0 % (95 %-CI [44.5 %, 75.8 %]) of the affected donors (25/41) and bilateral calcification in 39.0 % (16/41) (95 %-CI [24.2 %, 55.5 %]). There was a significant correlation between the mean amount of cartilage calcification of one MH with the mean amount of cartilage calcification of the contralateral side in individuals with bilateral calcification (rs = 0.40; 95 %-CI: [0.26, 0.52], p < 0.001). Overall, cartilage calcification was detectable in 57 of 168 joints (33.9 %).
Histochemical staining with von Kossa confirmed the presence of hyaline cartilage calcifications (Additional file 2: Figure S2 B).
The distribution of the prevalence of cartilage calcification by age and BMI is shown in Table 3.
Gender-specific prevalence of cartilage calcification of the 1st MH
Cartilage calcification in at least one MH was detected by DCR in 51.4 % of female (19/37) (95 %-CI [34.4 %, 68.1 %]) and in 46.8 % of male donors (22/47) (95 %-CI [32.1 %, 61.9 %]), corresponding to an overall prevalence of cartilage calcification within the study population of 48.8 % (95 %-CI [37.7 %, 60.0 %]) (Table 2). In summary, no significant difference in cartilage calcification of the 1st MH could be detected for gender (p = 0.41).
Correlation of cartilage calcification of the 1st MH with histological OA grade by OARSI
The distribution of the histological OA grade by OARSI and the corresponding prevalence of DCR-detectable cartilage calcification is shown in Table 4 (n = 168). A histological OA grade by OARSI ≥ 3 was considered as severe osteoarthritis.
In 85.7 % (144/168) of all analyzed metatarsal heads only mild cartilage damage (OARSI < 3) was detected. Accordingly, 14.3 % (24/168) of all metatarsal heads displayed severe cartilage damage (OARSI ≥ 3). Cartilage calcification was detectable by DCR in 75 % of samples with OARSI ≥ 3 (18/24). Interestingly, even in the samples with mild or no cartilage damage (OARSI < 3) cartilage calcification was also detectable in 27.1 % (39/144) of the analyzed samples.
In addition, the percentage of samples with DCR-detectable cartilage calcifications rises with increase of the histological OA grade by OARSI (Table 4) and there was a significant correlation between the mean amount of cartilage calcification (in % of total cartilage area) of the MH and histological OA grade by OARSI (rs = 0.51, 95 %-CI [0.32, 0.65], p < 0.001) (Fig. 1a).
Correlation between CC and histological OA grade by OARSI (a), between CC and age (b) and between CC and BMI (c). The scatter diagrams (data points are jittered to avoid overplotting) show the relation between the mean amount of cartilage calcification (in % of total cartilage area) and histological OA grade by OARSI (a), respectively age in years (b) and BMI (c). For better overview, the y-axis is displayed on a logarithmic scale. The scatter diagram A is shown with an orthogonal linear regression line (blue line). The mean amount of cartilage calcification correlated significantly with the histological OA grade (a) (rs = 0.51, 95 %-CI[0.32, 0.65], p < 0.001) but not with age (b) (rs = 0.20, 95 %-CI[−0.02, 0.40], p = 0.07) or BMI (c) (rs = −0.07, 95 %-CI[−0.17, 0.14], p = 0.51)
Correlation of cartilage calcification of the 1st MH and age
There was no significant correlation between the mean amount of cartilage calcification (in % of total cartilage area) with age (rs = 0.20, 95 %-CI [−0.02, 0.40], p = 0.07) (Fig. 1b).
Correlation of cartilage calcification of the 1st MH and BMI
There was no significant correlation between BMI and the mean amount of hyaline cartilage calcification. (Fig. 1c) (rs = −0.07, p = 0.51).
Interrelationship between cartilage calcification, histological OA grade, age and BMI
To analyze the interaction of cartilage calcification, histological OA grade, age and BMI simultaneously, simple regression analysis is not an appropriate tool. For a simultaneous analysis of these interrelationships we used structural equation modeling (SEM), which directly accounts for measurement error in the estimation. The histological OA grade and cartilage calcification were included as latent variables, age and BMI as manifest variables. Latent variables are factors, which consist of at least two inter-related measured variables. They are called latent because they are not directly measured, but rather are represented by the overlapping variance of measured variables. They are said to better represent the research constructs than measured variables because they contain less measurement error [47].
The SEM is schematically represented in Fig. 2. There was a significant correlation between cartilage calcification and histological OA grade (r = 0.74, 95 %-CI [0.43, 1.05], p < 0.001). Age had no influence on cartilage calcification (p = 0.15, 95 %-CI [−0.08, 0.53]), but a significant influence on histological OA grade (β = 0.62, 95 %-CI [0.26, 0.99], p = 0.001). BMI had no influence on cartilage calcification (p = 0.37, 95 %-CI [−0.45, 0.17]) or histological OA grade (p = 0.16, 95 %-CI [−0.56, 0.09]). The measures of global model fit indicated a good model fit (Chi-square = 7.83, p = 0.17, df = 5; RMSEA = 0.08).
Structural equation model. Manifest (measured) variables are represented by boxes, latent (i. e. not observable) variables are represented by circles. Abbreviations: hOA = histological osteoarthritis grade, CC = cartilage calcification, Age = age in years, BMI = body mass index [kg/m2], CCL/R = DCR-detctable hyaline cartilage calcification of the left/right central axial slab of MH, OAL/R = histological OA grade (by OARSI) of the left/right MH
Discussion
In this cross-sectional study we analyzed and quantified articular cartilage calcification of 168 metatarsophalangeal joints by a high-resolution imaging technique (DCR) in a post-mortem cohort of 84 adult donors. There prevalence of cartilage calcification of the 1st MTPJ in the cohort was 48.8 % (41 of 84 donors). Cartilage calcification was detectable in 33.9 % of all analyzed joints (57/168). In cases with bilateral manifestation, there was a significant correlation between the mean amounts of cartilage calcification of one joint with the mean amount of cartilage calcification of the contralateral side. The mean amount of cartilage calcification correlated significantly with histological OA grade, but not with age, gender or BMI.
To our knowledge, this is the first time that articular cartilage calcification of the first MTP joint is described and quantified by a high-resolution imaging technique (DCR).
Other cross-sectional studies have analyzed the prevalence of cartilage calcification by standard radiography in various joints. The reported prevalence of CC was considerably lower than in the current study (knee 7–21 %, hip 0,4–5 %, wrist 5–8 % and symphysis pubis 3–12 %) [24–30]. The only study that has applied DCR to detect cartilage calcification in the general population has been published by Mitsuyama et al. who have observed cartilage calcification in 100 % of 106 knee joints from the general population (mean age 50.3 years, range 12–74) [40]. In this paper, the authors have detected cartilage calcification already in knees of young donors (<20 years) without macroscopically severe OA and they have shown an association between increasing amount of cartilage calcification and increasing age [40], but did not adjust for the histological OA grade in their analyses. In our study, hyaline cartilage calcification was also detected in joints of young donors, but in contrast to Mitsuyama et al., we adjusted for histological OA grade and did not find an association between cartilage calcification and age. It is conceivable, although currently speculative, that the association of knee joint CC with age in the study of Mitsuyama et al. would disappear after adjustment for OA grade. Based on our current data, at least in the 1st MTPJ, we believe that cartilage calcification is an age-independent process. In the heavily loaded 1st MTPJ, mechanical stress could be a predisposing factor for CC. However, in the present analysis, the additional mechanical stress induced by increasing BMI did not appear to have an influence on cartilage calcification, nor on OA grade of the 1st MTPJ. These data argue against mechanical load as a relevant contributing factor in the genesis of cartilage calcifications. Along similar lines, Nguyen et al. described that hyaline cartilage calcification was also found in less weight-bearing zones of knee joints [48]. To clarify the relevance of these still preliminary observations, further studies with direct comparisons of weight-bearing and non-weight-bearing joints, respectively joints zones are required.
The observation that cartilage calcification is already observed to a large degree in samples without signs of severe OA (CC in 27.1 % of all analyzed samples with OARSI < 3) is highly intriguing. Similar findings have been described in two animal models of spontaneous OA, in which cartilage calcification was detected before cartilage degeneration occurred [49, 50]. Taken together, these data confirm the notion that cartilage calcification occurs not only in OA joints but also in histologically intact hyaline cartilage. Although this is strongly suggestive of a causal relationship between CC and OA, the biological meaning of this observation will have to be uncovered by future studies.
Nevertheless and as expected from observations in other joints, we also found a significant relationship between cartilage calcification of the 1st MTPJ and histological OA grade. Taken together, these data can be seen as a hint that increasing amount of cartilage calcification may trigger and accelerate OA progression by yet to be identified molecular mechanisms.
This study has some limitations. There was no detailed history of the donors about predisposing factors of OA of the 1st MTPJ such as infection, previous trauma or chronic mechanical overload. Moreover, it remains unclear whether the donors had clinical symptoms such as pain or reduced mobility of the 1st MTPJ. Another limitation of the study was that the analyzed cartilage-bone slabs of the metatarsal head reflect only a small part of the whole cartilage surface of the joint. Finally we have not performed an analysis of the type of cartilage calcification (BCP or CPPD). For this characterization a complex and time-consuming analysis by FTIR spectroscopy or X-Ray diffractometry is required, which was not the objective of this study.
Conclusion
DCR analysis of articular cartilage calcification of the 1st MTPJ in a cross sectional cohort of the general population revealed that cartilage calcification already occurs in histologically intact hyaline cartilage, is associated with OA severity but is independent of age and BMI.
These novel and partially unexpected data are suggestive of an intimate relationship between cartilage calcification and the pathogenesis of OA but at the same time demonstrate that a lot more work is required before we will reach a comprehensive understanding of the biological and pathophysiological role of hyaline cartilage calcification.
Abbreviations
- 1stMTPJ:
-
First metatarsophalangeal joint
- BMI:
-
Body mass index
- CC:
-
Cartilage calcification
- DCR:
-
Digital contact radiography
- hOA:
-
Histological osteoarthritis grade
- MH:
-
Metatarsal head
- OA:
-
Osteoarthritis
- OARSI:
-
Osteoarthritis cartilage histopathology assessment system
- SEM:
-
Structural equiation modeling
References
Keenan AM, Tennant A, Fear J, Emery P, Conaghan PG. Impact of multiple joint problems on daily living tasks in people in the community over age fifty-five. Arthritis Rheum. 2006;55:757e64.
Gorter KJ, Kuyvenhoven MM, de Melker RA. Nontraumatic foot complaints in older people. A population based survey of risk factors, mobility, and well-being. J Am Podiatr Med Assoc. 2000;90:397e402.
Camasta C. Hallux limitus and hallux rigidus. Clin Pod Med Surg. 1996;13:425–8.
Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, eitology and radiographic assessment. Foot Ankle Int. 2003;24:731–43.
Iagnocco A, Rizzo C, Gattamelata A, et al. Osteoarthritis of the foot: a review of the current state of knowledge. Med Ultrason. 2013;15(1):35–40.
Menz HB, Munteanu SE, Landorf KB, Zammit GV, Cicuttini FM. Radiographic evaluation of foot osteoarthritis: sensitivity of radiographic variables and relationship to symptoms. Osteoarthritis Cartilage. 2009;17(3):298–303.
Wilder FV, Barrett JP, Farina EJ. The association of radiographic foot osteoarthritis and radiographic osteoarthritis at other sites. Osteoarthritis Cartilage. 2005b;13(3):211e5.
van Saase JL, van Romunde LK, Cats A, Vandenbroucke JP, Valkenburg HA. Epidemiology of osteoarthritis: Zoetermeer Survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Ann Rheum Dis. 1989;48(4):271e80.
Beeson P, Phillips C, Coor S, et al. Cross-sectional study to evaluate radiological parameters in hallux rigidus. Foot (Edinb). 2009;19:7–21.
Munuera PV, Dominguez G, Castillo JM. Radiographic study of the size of the first metatarsophalangeal segment in feet with incipient hallux limitus. J Am Podiatr Med Assoc. 2007;97:46–8.
Zammit GV, Hylton BM, Muneaunu SE. Structural factors associated with hallux limitus/rigidus: a systematic review of case control studies. J Orthop Sports Phys Ther. 2009;39:733–42.
Englund M. The role of biomechanics in the initiation and progression of OA of the knee. Best Pract Res Clin Rheumatol. 2010;24:39–46.
Stein G, Pawel A, Koebke J, et al. Morphology of the first metatarsal head and hallux rigidus: a cadaveric study. Surg Radiol Anat. 2012;34(7):589–92.
McMaster MJ. The pathogenesis of hallux rigidus. J Bone Joint Surg Br. 1978;60:82–7.
Goodfellow J. Aetiology of hallux rigidus. Proc R Soc Med. 1966;59(9):821–4.
Kessel L, Bonney G. Hallux rigidus in the adolescent. J Bone Joint Surg Br. 1958;40-B(4):669–73.
Roddy E, Zhang W, Doherty M. Are joints affected by gout also affected by osteoarthritis? Ann Rheum Dis. 2007;66(10):1374–7.
Shereff MJ, Baumhauer JF. Hallux rigidus and osteoarthrosis of the first metatarsophalangeal joint. J Bone Joint Surg Am. 1998;80(6):898–908.
Landis WJ, Jacquet R. Association of calcium and phosphate ions with collagen in the mineralization of vertebrate tissues. Calcif Tissue Int. 2013;93(4):329–37.
Cotran RS, Kumare V, Robbins SL. Cellular injury and cellular death. In: Robbins SL, editor. Pathological Basis of Disease. 5th ed. Philadelphia: WB Saunders; 1994. p. 1–35.
Zhang W, Doherty M, Bardin T, et al. European league against rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann Rheum Dis. 2011;70(4):563–70.
Fuerst M, Bertrand J, Lammers L, et al. Calcification of articular cartilage in human osteoarthritis. Arthritis Rheum. 2009;60(9):2694–703.
Abreu M, Johnson K, Chung CB, et al. Calcification in calcium pyrophosphate dihydrate (CPPD) crystalline deposits in the knee: anatomic, radiographic, MR imaging, and histologic study in cadavers. Skeletal Radiol. 2004;33(7):392–8.
Derfus BA, Kurian JB, Butler JJ, et al. The high prevalence of pathologic calcium crystals in preoperative knees. J Rheumatol. 2002;29:570–4.
Gordon GV, Villanueva T, Schumacher HR, Gohel V. Autopsy study correlating degree of osteoarthritis, synovitis and evidence of articular calcification. J Rheumatol. 1984;11(5):681–6.
Felson DT, Anderson JJ, Naimark A, Kannel W, Meenan RF. The prevalence of chondrocalcinosis in the elderly and its association with knee osteoarthritis: the Framingham Study. J Rheumatol. 1989;16(9):1241–5.
Ramonda R, Musacchio E, Perissinotto E, et al. Prevalence of articular chondrocalcinosis in elderly subjects in a rural area of Catalonia. Ann Rheum Dis. 1993;52(6):418–22.
Neame RL, Carr AJ, Muir K, Doherty M. UK community prevalence of knee chondrocalcinosis: evidence that correlation with osteoarthritis is through a shared association with osteophyte. Ann Rheum Dis. 2003;62(6):513–8.
Wilkins E, Dieppe P, Maddison P, Evison G. Osteoarthritis and articular chondrocalcinosis in the elderly. Ann Rheum Dis. 1983;42(3):280–4.
Abhishek A, Doherty S, Maciewicz R, et al. Evidence of a systemic predisposition to chondrocalcinosis and association between chondrocalcinosis and osteoarthritis at distant joints: a cross-sectional study. Arthritis Care Res (Hoboken). 2013;65(7):1052–8.
Fuerst M, Niggemeyer O, Lammers L, et al. Articular cartilage mineralization in osteoarthritis of the hip. BMC Musculoskelet Disord. 2009;10(12):166.
Fuerst M, Lammers L, Schäfer F, et al. Investigation of calcium crystals in OA knees. Rheumatol Int. 2010;30(5):623–31.
Rosenthal AK. Update in calcium deposition diseases. Curr Opin Rheumatol. 2007;19(2):158–62.
Lioté F, Ea HK. Clinical implications of pathogenic calcium crystals. Curr Opin Rheumatol. 2014;26(2):192–6.
Ea H-K, Nguyen C, Bazin D, et al. Articular cartilage calcification in osteoarthritis: insights into crystal induced stress. Arthritis Rheum. 2011;63(1):10–8.
Rosenthal AK. Crystals, inflammation, and osteoarthritis. Curr Opin Rheumatol. 2011;23(2):170–3.
Ishida T, Dorfman HD, Bullough PG. Tophaceous pseudogout (tumoral calcium pyrophosphate dihydrate crystal deposition disease). Hum Pathol. 1995;26(6):587–93.
Contreras M, Nolla JM, Mateo L, Rozadilla A. Pseudopodagra caused by hydroxyapatite. Report of 3 cases. Rev Clin Esp. 1993;192(4):173–4.
Mines D, Abbuhl SB. Hydroxyapatite pseudopodagra in a young man: acute calcific periarthritis of the first metatarsophalangeal joint. Am J Emerg Med. 1996;14(2):180–2.
Mitsuyama H, Healey RM, Terkeltaub RA, Coutts RD, Amiel D. Calcification of human articular knee cartilage is primarily an effect of aging rather than osteoarthritis. Osteoarthritis Cartilage. 2007;15(5):559–65.
Pritzker KP, Gay S, Jimenez SA, et al. Osteoarthritis cartilage histopathology: grading and staging. Osteoarthritis Cartilage. 2006;14(1):13–29.
Klein RB. Principles and Practice of Structural Equation Modeling. 3rd ed. New York: The Guilford Press; 2010.
Hair JF, Black WC, Babin BJ, Anderson RE, Tatham RL. Multivariate data analysis. 6th ed. Upper Saddle River: Pearson/Prentice Hall; 2006.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. http://www.R-project.org/. Vienna, Austria. 2014.
Rosseel Y, Lavaan. An R package for structural equation modeling. J Stat Softw. 2012;48(2):1–36.
Wickham H. ggplot2: elegant graphics for data analysis. 1st ed. New York: Springer; 2009.
Beran TN, Violato C. Structural equation modeling in medical research: a primer. BMC Res Notes. 2010;3:267.
Nguyen C, Bazin D, Daudon M, et al. Revisiting spatial distribution and biochemical composition of calcium-containing crystals in human osteoarthritic articular cartilage. Arthritis Res Ther. 2013;15(5):R103.
Bendele AM, White SL. Early histopathologic and ultrastructural alterations in femorotibial joints of partial medial meniscectomized guinea pigs. Vet Pathol. 1987;24(5):436–43.
Evans RG, Collins C, Miller P, Ponsford FM, Elson CJ. Radiological scoring of osteoarthritis progression in STR/ORT mice. Osteoarthritis Cartilage. 1994;2(2):103–9.
Acknowledgements
We thank Prof. Michael Amling, IOBM, University Medical Center Hamburg, Germany, for helpful discussions and support and Elke Leicht for expert technical assistance.
Funding
No specific funding was received from any funding bodies in the public, commercial or not-for-profit sectors to carry out the work described in this manuscript.
Availability of data and material
All data generated or analyzed in this study is available on request from first or corresponding authors.
Authors’ contributions
JH, TH contributed to the conception and design of the study, acquisition of data, analysis and interpretation of data, as well as drafting and revision of the manuscript. JH and TH contributed equally to this work. SH was responsible for interpretation of the data and statistical analysis. MK contributed DCR analysis and interpretation of the data. JB contributed to the conception and design of the study, data acquisition and interpretation. KP contributed to the acquisition of data. WR contributed to the conception and design of the study. AN contributed to the conception and design of the study, analysis and interpretation of data, as well as drafting and revision of the manuscript. All authors included on this paper have made substantial contributions to this work and fulfill therefore the criteria of authorship. All authors read and approved the final manuscript. JH, TH and AN take responsibility for the integrity of the work as a whole, from inception to finished article.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This cross-sectional study was approved by the local Ethics Committee of the Medical Association Hamburg, Germany (Ärztekammer Hamburg, PV: 4570) and was carried out according to existing rules and regulations of the University Medical Center Hamburg-Eppendorf. Informed consent to the removal and use of the joints for scientific purposes was obtained from the family members.
Author information
Authors and Affiliations
Corresponding authors
Additional files
Additional file 1: Figure S1.
Sample preparation and DCR. A. Each metatarsal head (MH) of the 1st MTPJ was cut in one standardized 4 mm thick cartilage-bone-slab (dashed line) along the central axial plane. B. Radiographs were taken from each cartilage-bone slab of the MH using a high-resolution digital radiography device (DCR). In these radiographs, calcifications of the hyaline cartilage could be detected as radiopaque spots (red arrow) within the surrounding cartilage matrix. The mean amount of total cartilage calcification in % of total cartilage area for each MH was measured by image-analysis software. (DOCX 6230 KB)
Additional file 2: Figure S2.
DCR-images and histological examination. A. DCR-images with hyaline cartilage calcifications (original size and 3 × magnification) of cartilage-bone slabs of the metatarsal heads from different donors and the corresponding Safranin O stainings from the central load-bearing zone of the metatarsal head. Histological OA grade was evaluated by the OARSI score. Deposition of cartilage calcification was detectable in all OA grades (OARSI 0–6) by DCR. B. The existence of DCR-detectable hyaline cartilage calcification (calcium-phosphate-crystals) was histochemically confirmed by von Kossa stainings. (DOCX 2250 KB)
Additional file 3: Figure S3.
Study population histogram by decade. 84 donors; 37 female and 47 male. The mean age was 62.73 years, SD ± 18.8, range 20–93 years. (DOCX 20 KB)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hubert, J., Hawellek, T., Hischke, S. et al. Hyaline cartilage calcification of the first metatarsophalangeal joint is associated with osteoarthritis but independent of age and BMI. BMC Musculoskelet Disord 17, 474 (2016). https://doi.org/10.1186/s12891-016-1324-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-016-1324-0