Abstract
Background
Hemichorea is a rare manifestation of nonketotic hyperglycemia that usually affects elderly Asian women with poor glycemic control. Non-contrast computerized Tomography and T1- weighted Magnetic Resonance Imaging shows characteristic hyperintense basal ganglia lesions.
Case presentation
A Fifty-seven year old Sri Lankan female presented with a two-day history of right upper limb chorea. She had been diagnosed with diabetes mellitus one year ago, but was not on any treatment and did not have any micro vascular or macro vascular complications. Random blood sugar was 420 mg/dl and full blood count, liver function tests, renal function tests, inflammatory markers, thyroid function tests, Urine protein / creatinine ratio, electrocardiogram and 2D Echo were normal. Arterial blood gas did not show acidosis and ketone bodies were not detected in urine. Non-contrast computerized Tomography brain on day 1 showed left side hyperdense lentiform and caudate nuclei and MRI on day 3 showed slightly high signal intensity of left side basal ganglia on T1- weighted images and low signal intensity on T2-weighted and Fluid-attenuated inversion recovery images. She was started on insulin and a low dose of clonazepam and glycemic control was achieved on day 3. Two days later, the chorea completely disappeared. CT brain was repeated 4 days and 10 days following glycemic control, which showed rapid resolution of CT changes. Clonazepam was stopped in 2 weeks and chorea did not recur.
Conclusion
This is a rare manifestation of diabetes in Sri lanka and diagnosing this rare entity will direct clinicians to achieve optimum glycemic control as the treatment which will lead to rapid clinical response without any other medications. In this case report we high light that with the clinical improvement, repeating a CT scan even after a very short period like 2 weeks will show rapid radiological resolution. This repeat imaging can also be useful to confirm the diagnosis, which will minimize unnecessary investigations and treatments. Further cases of hyperglycemic nonketotic chorea with brain imaging performed within short intervals is needed to evaluate the nature of rapid radiological changes, which will be useful to understand the pathology of this condition.
Similar content being viewed by others
Background
Hemichorea is a rare manifestation of nonketotic hyperglycemia that usually affects elderly Asian women with poor glycemic control. The pathophysiology of hemichorea in hyperglycemia is controversial but these patients display distinct neuroimaging features. Non Contrast Computerized Tomography (NCCT) and T1- weighted Magnetic resonance imaging (MRI) show characteristic hyperintense basal ganglia lesions but the T2-weighted brain MRI findings vary [1,2,3]. In this case we followed up a patient with nonketotic hyperglycemic chorea with serial CT scans performed in very short intervals which revealed rapid radiological resolution.
Case presentation
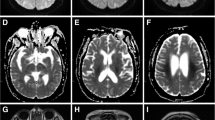
A Fifty-seven year old Sri Lankan female presented with a two-day history of acute onset right upper limb chorea. She had been diagnosed with diabetes mellitus one year ago, but was not on any treatment and did not have any micro vascular or macro vascular complications. On examination, right upper limb chorea was evident and the rest of the nervous system examination was normal including fundoscopy. Random blood sugar on admission was 420 mg/dl. Full blood count, liver function tests, renal function tests, inflammatory markers, thyroid function tests, Anti nuclear antibody, Urine protein / creatinine ratio, electrocardiogram and 2D Echo were normal. Arterial blood gas did not show acidosis and ketone bodies were not detected in urine. NCCT brain on day 1 showed left side hyperdense lentiform and caudate nuclei(Fig. 1). MRI on day 3 showed slightly high signal intensity of left side basal ganglia on T1- weighted images and low signal intensity on T2-weighted and Fluid-attenuated inversion recovery images(Fig. 2). Diffusion weighted imaging and Susceptibility weighted imaging were normal. She was started on insulin and a low dose of clonazepam (0.5 mg nocte) and glycemic control was achieved on day 3. Two days later, the chorea completely disappeared. NCCT was repeated 4 days and 10 days following glycemic control, which showed rapid resolution of CT changes (Fig. 1). Clonazepam was stopped in 2 weeks and chorea did not recur.
Serial NCCT brain showing resolution of left side high intensity basal ganglia. a: Day 1 NCCT brain showing left side hyperdense lentiform and caudate nuclei shown by black arrows. b: NCCT brain 4 days after glycemic control showing rapid resolution of left side hyperdense lentiform and caudate nuclei (The hyperdense area is shown by blue arrows). c: NCCT brain 10 days after glycemic control showing rapid resolution of left side hyperdense lentiform and caudate nuclei (The initial hyperdense area is shown by red arrows, which has resolved by day 10)
Discussion
In this case, the patient had hemichorea, nonketotic hyperglycemia and hyperintense caudate and lentiform nuclei on NCCT and T1-MRI supporting the diagnosis of hyperglycemic nonketotic chorea. Several hypotheses have been put forward to explain the mechanism of chorea including relative dopaminergic hypersensitivity, vascular insufficiency causing transient ischemia to basal ganglia and shifting of cerebral metabolism to the anaerobic pathway causing reduction in both GABA and acetylcholine with metabolic acidosis leading to basal ganglia dysfunction [1, 2, 4]. As in our case, in most of the cases the chorea ameliorated completely with good glycemic control [1, 5] suggesting a reversible pathology.
Lai, P.H. at el., evaluated neuroimaging of 10 patients with nonketotic hyperglycemic hemichorea in primary diabetes mellitus and CT and T1-weighted MR images showed lesions of the putamen and/or caudate unilaterally or bilaterally. Lin, J.J. and colleagues report 7 similar patients with CT showing an increased density in the contralateral putamen and/or caudate and MRI revealing abnormal hyperintensity on T1-weighted and hypointensity on T2-weighted images [5]. The theories for characteristic radiological findings are abnormal deposition of calcium in neurons or glial cells, petechial hemorrhages from small vessels, extravascular hemosiderin deposition and gemistocyte (swollen reactive astrocytes having rich protein content) accumulation following acute injury [4]. Lin, J.J. and colleagues followed up 7 patients and the lesions on CT and MRI showed complete resolution within 3 months and 11 months, respectively [5]. In one literature survey, 19 out of 22 patients who had a follow-up brain MRI after an interval of 2 months – 1.5 years, the high signal intensity basal ganglia lesions resolved along with the improvement in chorea [1]. In another case series, 8 out of 9 patients underwent follow up CT scans within an interval of 1–18 months and the hyperdense striatal lesions had disappeared completely or near-completely [6].
In our patient we did serial CT scans over two weeks, which showed rapid resolution. As mentioned above, we came across on very few case reports in literature where the progression of radiological manifestations was monitored, but in this case we did CT scans in very short intervals. Previous case reports describe rapid clinical improvement but in this case with the resolution of chorea following glycemic control we also noticed the improvement of the CT scan within a very short period of few days. The rapid resolution of radiological changes suggests that the pathological changes in the brain parenchyma in hyperglycemic nonketotic chorea are rapidly reversing.
Conclusion
The patient had poorly controlled diabetes without any complications, suggesting that chorea might not be related to microvascular or macrovascular complications of diabetes. This is a rare manifestation of diabetes in Sri lanka and diagnosing this rare entity will direct clinicians to achieve optimum glycemic control as the treatment which will lead to rapid clinical response without any other medications. In this case report we high light that with the clinical improvement, repeating a CT scan even after a very short period like 2 weeks will show rapid radiological resolution. This repeat imaging can also be useful to confirm the diagnosis, which will minimize unnecessary investigations and treatments. Further case reports and case series of hyperglycemic nonketotic chorea with brain imaging performed within short intervals is needed to evaluate the nature of rapid radiological changes which will be useful to understand the pathology of this condition.
Abbreviations
- MRI:
-
Magnetic Resonance Imaging
- NCCT:
-
Non-Contrast Computerized Tomography
References
Oh SH, et al. Chorea associated with non-ketotic hyperglycemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI study: a meta-analysis of 53 cases including four present cases. J Neurol Sci. 2002;200(1–2):57–62.
Chang KH, et al. Temporal features of magnetic resonance imaging and spectroscopy in non-ketotic hyperglycemic chorea-ballism patients. Eur J Neurol. 2010;17(4):589–93.
Lai PH, et al. Chorea-ballismus with nonketotic hyperglycemia in primary diabetes mellitus. AJNR Am J Neuroradiol. 1996;17(6):1057–64.
Cherian A, et al. Concepts and controversies in nonketotic hyperglycemia-induced hemichorea: further evidence from susceptibility-weighted MR imaging. J Magn Reson Imaging. 2009;29(3):699–703.
Lin JJ, et al. Presentation of striatal hyperintensity on T1-weighted MRI in patients with hemiballism-hemichorea caused by non-ketotic hyperglycemia: report of seven new cases and a review of literature. J Neurol. 2001;248(9):750–5.
Chromoblastomycosis. Urol Cutaneous Rev. 1946;50(6):341–3.
Acknowledgements
This case report was supported by doctors working in ward 16, national hospital of Sri Lanka, in acquisition, analysis and interpretation of data.
Funding
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
All data are included in the manuscript.
Author information
Authors and Affiliations
Contributions
Dr. HMMTBH collected data, followed up the patient and did the literature review and designed,drafted the manuscript. Dr. SPP assisted in the literature review, analyzing, and designed, drafted the manuscript. Dr. SS is the consultant managing the patient and collected data, followed up the patient and designed, drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The Authors declare that there they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Herath, H., Pahalagamage, S. & Senanayake, S. Case report of hyperglycemic nonketotic chorea with rapid radiological resolution. BMC Med Imaging 17, 54 (2017). https://doi.org/10.1186/s12880-017-0228-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-017-0228-2