Abstract
Background
Invasive pulmonary aspergillosis (IPA) is seen during coronavirus-2019 (COVID-19), has been reported in different incidences, and is defined as COVID-19-associated pulmonary aspergillosis (CAPA). Detection of galactomannan antigen is an important diagnostic step in diagnosing IPA. Enzyme-linked immunoassay (ELISA) is the most frequently used method, and lateral flow assay (LFA) is increasingly used with high sensitivity and specificity for rapid diagnosis. The present study aimed to compare the sensitivity of LFA and ELISA in the diagnosis of CAPA in COVID-19 patients followed in our hospital's ICU for pandemic (ICU-P).
Methods
This study included patients with a diagnosis of COVID-19 cases confirmed by polymerase chain reaction and were followed up in ICU-P between August 2021 and February 2022 with acute respiratory failure. The diagnosis of CAPA was based on the European Confederation of Medical Mycology (ECMM) and the International Society for Human and Animal Mycology 2020 (ECMM/ ISHAM) guideline. Galactomannan levels were determined using LFA and ELISA in serum samples taken simultaneously from the patients.
Results
Out of the 174 patients followed in the ICU-P, 56 did not meet any criteria for CAPA and were excluded from the analysis. The rate of patients diagnosed with proven CAPA was 5.7% (10 patients). A statistically significant result was obtained with LFA for the cut-off value of 0.5 ODI in the diagnosis of CAPA (p < 0.001). The same significant statistical relationship was found for the cut-off value of 1.0 ODI for the ELISA (p < 0.01). The sensitivity of LFA was 80% (95% CI: 0.55–1.05, p < 0.05), specificity 94% (95% CI: 0.89–0.98, p < 0.05); PPV 53% (95% CI: 0.28–0.79, p > 0.05) and NPV was 98% (95% CI: 0.95–1.01, p < 0.05). The risk of death was 1.66 (HR: 1.66, 95% CI: 1.02–2.86, p < 0.05) times higher in patients with an LFA result of ≥ 0.5 ODI than those with < 0.5 (p < 0.05).
Conclusions
It is reckoned that LFA can be used in future clinical practice, particularly given its effectiveness in patients with hematological malignancies and accuracy in diagnosing CAPA.
Similar content being viewed by others
Background
Coronavirus-2019 (COVID-19) continues to maintain its agenda as a serious pandemic factor. Different clinical manifestations associated with COVID-19 challenge clinicians, and secondary infections are an important cause of morbidity. Secondary bacterial infections have increased the need for mechanical ventilation and mortality [1, 2]. Invasive fungal infections occur as another cause of morbidity in the course of COVID-19 [3,4,5,6].
Invasive pulmonary aspergillosis (IPA), defined as COVID-19-associated pulmonary aspergillosis (CAPA), has been reported in different incidences [7,8,9,10,11,12,13,14,15,16]. IPA is one of the viral infections increasing susceptibility to bacterial and fungal infections [5, 6]. Respiratory viruses can directly damage the airway and predispose to fungal infections [5, 6]. Lympopenia, especially seen in the course of viral infections, is an important risk factor [5, 6]. In addition, steroid use has been identified as an important risk factor for both IPA susceptibility and mortality [4, 7]. Conditions that cause profound immunosuppression such as hematopoietic stem cell transplantation or acute leukemias or conditions associated with respiratory epithelial damage such as chronic obstructive pulmonary disease or asthma are the main predisposing diseases [5,6,7,8]. Broad-spectrum antibiotic therapy agents used in intensive care units (ICUs) also disrupt the natural microbial barriers and increase susceptibility to fungal infections [4, 7]. Hypertension, coronary heart diseases, and diabetes are the other defined predisposing diseases for CAPA [4]. Aspergillus fumigatus was found to be the most prevalent Aspergillus spp. isolated among respiratory samples with positive cultures followed by Aspergillus flavus [17].
Detection of galactomannan antigen is an important diagnostic step in diagnosing IPA. Galactomannan is a polysaccharide antigen located in the wall structure of Aspergillus species [18]. Enzyme-linked immunoassay (ELISA) is the most frequently used method, and lateral flow assay (LFA) is increasingly used with high sensitivity and specificity for rapid diagnosis. LFA is a self-contained immunochromatographic test for the qualitative and quantitative detection of galactomannan antigen from different samples. The principle of LFA use is based on the lateral flow, and it is based on the formation of complexes of galactomannan-specific antibodies in samples with antigens. The resulting complex is detected with a visible line, and quantitative results are obtained utilizing different specific devices [19]. In a study from our clinic, the diagnostic efficiency of LFA and ELISA were evaluated simultaneously for 87 patients diagnosed with hematological malignancy. LFA was more specific than ELISA in terms of the cut-off value of 0.5 optical density index (ODI) [20].
The present study aimed to compare the sensitivity of LFA and ELISA in the diagnosis of CAPA in COVID-19 patients followed in our hospital's ICU for pandemic (ICU-P).
Materials and methods
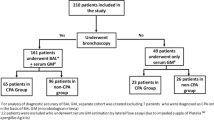
This study included patients with a diagnosis of COVID-19 cases confirmed by polymerase chain reaction (PCR) and were followed up in ICU-P between August 2021 and February 2022 with acute respiratory failure (ARF). The diagnosis of CAPA was based on the European Confederation of Medical Mycology (ECMM) and the International Society for Human and Animal Mycology 2020 (ECMM/ ISHAM) guidelines [5]. The criteria are shown in Table 1. Patients not considered for CAPA were excluded from the study. The remaining cases were categorized according to the relevant guideline (Fig. 1 Patients' flowchart).
In addition to demographic data such as age and gender, comorbidities, being diagnosed with an active solid or hematological malignancy, immunosuppressive drug usage, and survival of the patients included in the study were recorded. Galactomannan levels were determined using LFA and ELISA in serum samples taken simultaneously from the patients.
Serum samples were taken from all patients at the time of admission to the ICU-P and the results were obtained and recorded after studying the samples with LFA and ELISA on the same day. Sterile respiratory tract samples taken at the time of hospitalization or during follow-up in ICU-P were subjected to direct microscopic examination, culture on Sabouraud medium and cytopathological examination.
LFA analysis
For the LFA (sōna Aspergillus galactomannan LFA, IMMY, Norman, Oklahoma, United States of America), 300 µL of serum was pretreated by addition of 100 µL of EDTA-containing buffer, heating at 120 °C for 6–8 min and centrifugation. Eighty microliters of the resulting supernatant were transferred to a separate test tube to which 40 μL of running buffer was added. A test strip was then inserted into this tube. Results were recorded after 30 min. All tests were performed by the same researcher (IS) and read using a digital reader (Cube reader, Chembio Diagnostics GmbH) provided by the manufacturer.
Statistical analysis
In the analysis of the data, the mean and standard deviation, median, minimum and maximum values of the features, frequency, and percentage values were used to identify categorical variables. Parametric tests were used without the normality test due to the compatibility of the Central Limit Theorem [21]. A Chi-square test statistic was used to evaluate the relationship between two independent variables. In evaluating the diagnostic performance of the LFA and ELISA method, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio, negative likelihood ratio, accuracy, and diagnostic odds ratio statistics were used. Differences based on LFA (cut-off: 0.5) and ELISA (cut-off: 1.0) groups were determined by the Log-Rank test, and the Hazard ratio (HR) was given with a 95% confidence interval. The statistical significance level of the data was taken as p < 0.05. New York software and MedCalc statistical package program were used for the data evaluation.
Ethical committee approval was received (Istanbul Training and Research Hospital, approval date, and number: 28/01/2022-28).
Results
Out of the 174 patients followed in the ICU-P, 56 did not meet any criteria for CAPA and were excluded from the analysis. The rate of patients diagnosed with proven CAPA was 5.7% (10 patients). The most common comorbidity encountered was hypertension, with 32.2%. A total of 88 patients died in the ICU-P follow-up (74.6%) (Table 2).
A statistically significant result was obtained with LFA for the cut-off value of 0.5 ODI in the diagnosis of CAPA (p < 0.001). The same significant statistical relationship was found for the cut-off value of 1.0 ODI for the ELISA (p < 0.01) (Table 3).
Table 4 shows the diagnostic test performance analysis for the cut-off value of 0.5 ODI for the LFA test in the diagnosis of CAPA. The sensitivity was 80% (95% CI: 0.55–1.05, p < 0.05) and the specificity was 94% (95% CI: 0.89–0.98, p < 0.05). Figure 2 shows the comparative ROC analysis of LFA and ELISA for the cut-off value of 0.5 ODI.
Table 4 shows also the diagnostic test performance analysis for the cut-off value of 1.0 ODI for the ELISA in the diagnosis of CAPA. The sensitivity was 20% (95% CI: 0.05–0.45, p > 0.05) and the specificity was 97% (95% CI: 0.94–0.99, p < 0.05).
The total number of patients who died in the follow-up interval of the 0-207th day was 88 (74.58%), and the number of non-ex was 30 (25.42%). The results of the log-rank test for comparing the two survival curves are shown in Table 5. Life curves were found to differ substantially, and an LFA result of 0.5 ODI significantly affected survival (p < 0.05). The risk of death was 1.66 (HR: 1.66, 95% CI: 1.02–2.86, p < 0.05) times higher in patients with an LFA result of ≥ 0.5 ODI than those with < 0.5 (p < 0.05). Moreover, the risk of death was 18.01 (HR: 18.01, 95% CI: 1.39–46.24, p < 0.05) times higher in those with an ELISA result of ≥ 1.0 ODI than those with < 1.0 (p < 0.05) (Table 5).
In Fig. 3, it was observed that the study was terminated on day 207 and the probability of survival (%) decreased. “Number at risk” indicates the number of patients at risk at the end of each period. While 15 patients with LFA results of ≥ 0.5 ODI were at risk at the beginning of the study (Day 0), the number of patients at risk was 5 at the end of the 50th day. In Fig. 4, the same analysis was performed for the ELISA cut-off value of ≥ 1.0 ODI. At the beginning of the study (Day 0), 5 patients were at risk, while at the end of the 50th day, the number of patients at risk was 0.
Discussion
This study reveals new findings in many aspects. While there were significant statistical results with LFA for the cut-off value of 0.5 ODI in the diagnosis of CAPA, the same significant statistical relationship was found for the cut-off value of 1.0 ODI for the ELISA. For the cut-off value of 0.5 ODI, sensitivity was 80%, specificity 94%, PPV 53% and NPV 98% for LFA. In addition, the risk of death was 1.66 times higher in patients with an LFA result of ≥ 0.5 ODI than those with < 0.5. LFA could play an important role in diagnosing aspergillosis secondary to viral infections due to its high sensitivity–specificity and ease of administration.
A review from 2022 revealed that the incidence of CAPA in patients with ICU follow-up ranges from 0 to 34.4% [22]. In another study, the incidence of CAPA was 10–15% in patients with ICU follow-up, and mortality was reported to be between 43 and 52% [7]. In another review, 1421 patients were evaluated, and CAPA mortality was found to be 48.4% [23]. In our study, the rate of patients diagnosed with proven CAPA was 5.7%, while mortality was 74.6% despite all effective treatment options. It should be noted that our center serves a large number of immigrant patients and therefore the number of patients who are not under follow-up and treatment in terms of their comorbidities caused the mortality rate to be quite high compared to other studies in literature.
In a recent study from 2022 [24], LFA was evaluated in COVID-19 patients with ARF; while the sensitivity of LFA was 20% for the cut-off value of 0.5 ODI, the specificity was 93%. The sensitivity for the cut-off value of 1.0 ODI was 9%, while the specificity was 99%. In this study, the diagnostic performance was examined with the combination of respiratory samples. In the analysis performed by combining tracheal aspirate, non-directed bronchial lavage, and bronchoalveolar lavage samples, the sensitivity was 83%, and the specificity was 44% for the cut-off value of 0.5 ODI. For the cut-off value of 1.0 ODI, the sensitivity was 81%, and the specificity was 67%. In another study [25], galactomannan antigen was studied by LFA and ELISA in both serum and bronchoalveolar lavage samples of COVID-19 patients followed up in the ICU.The sensitivity of LFA in serum samples for 0.5 ODI turned out to be 56.3% while the specificity was 94.2%. In our study, the sensitivity was 80%, and the specificity was 94% for the cut-off value of 0.5 ODI for LFA. The same statistical relationship could not be found for the cut-off value of 1.0 ODI for the LFA contrary to ELISA. Therefore, it is suggested that LFA can be used with very high sensitivity and specificity for 0.5 ODI in suspicion of CAPA. LFA seems to be more successful compered to ELISA in terms of low galactomannan-antigenemia.
Serum LFA efficacy has been studied in hematological malignancies where invasive fungal infections are common, and its efficacy has also been demonstrated. In the study of Hoenigl et al. [26], sensitivity for the cut-off value of 0.5 ODI was 78.6%, while specificity was 80.5%. In the study conducted in our clinic [20], the sensitivity was 90.9%, and the specificity was 90.8% for the same cut-off value. Although studies on the effectiveness of serum LFA in hematological malignancies seem to be more compatible with each other, CAPA has emerged as a newer field in evaluating the effectiveness of the LFA test. In our study, LFA yields successful results with a sensitivity of 80% and a specificity of 94% for 0.5 ODI for the diagnosis of CAPA. It is a non-invasive, rapid and effective diagnostic method for 0.5 ODI and can play an important role in the early diagnosis and treatment of ICU-patients for whom invasive diagnostic methods may not seem to be favorable options.
Besides diagnosing CAPA with high sensitivity and specificity, our study revealed important data regarding mortality. The risk of death was 1.66 times higher in patients with an LFA result of ≥ 0.5 ODI than those with < 0.5. In the multivariate analysis performed in the MYCOVID study from 2022, which included patients also with ICU follow-up, it was revealed that the diagnosis of probable or possible CAPA increased the mortality risk 1.45 times (HR: 1.45, 95% CI: 1.03–2.03, p = 0.033) [27]. Within current practices, where insufficient awareness is an important factor in the diagnosis and early treatment of CAPA, it could be thought that LFA will play an important role in high diagnostic performance and efficacy in mortality prediction.
There were also some limitations of this study. The fact that interventional methods are less accessible due to pandemic conditions may have limited the “proven” patient group. The fact that PCR is not used to diagnose aspergillus in our clinic might also have limited the proven CAPA group.
Conclusions
In conclusion, for LFA, the sensitivity was 80%, the specificity 94%, the PPV 53%, and NPV was 98% for the cut-off value of 0.5 ODI and was found to be superior to ELISA. In addition, the risk of death was 1.66 times higher in patients with an LFA result of ≥ 0.5 ODI than those with < 0.5. Concerning its efficiency in patients with hematological malignancies and accuracy diagnosing CAPA, LFA expected to be a useful and effective part of future clinical practices.
Availability of data and materials
Datasets analyzed during the current study are available in [Mendeley Data] [https://doi.org/10.17632/vc8rxy598m.1].
Abbreviations
- COVID-19:
-
Coronavirus-2019
- IPA:
-
Invasive pulmonary aspergillosis
- CAPA:
-
COVID-19-associated pulmonary aspergillosis
- ICU:
-
Intensive care units
- ELISA:
-
Enzyme-linked immunoassay
- LFA:
-
Lateral flow assay
- ODI:
-
Optical density index
- ICU-P:
-
Intensive care unit for pandemic
- PCR:
-
Polymerase chain reaction
- ARF:
-
Acute respiratory failure
- ECMM/ISHAM:
-
European Confederation of Medical Mycology (ECMM) and the International Society for Human and Animal Mycology 2020
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- HR:
-
Hazard ratio
References
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62.
Chong WH, Saha BK, Ananthakrishnan R, Chopra A. State-of-the-art review of secondary pulmonary infections in patients with COVID-19 pneumonia. Infection. 2021;49:591–605.
Jenks JD, Nam HH, Hoenigl M. Invasive aspergillosis in critically ill patients: review of definitions and diagnostic approaches. Mycoses. 2021;64:1002–14.
Arastehfar A, Carvalho A, van de Veerdonk FL, Jenks JD, Koehler P, Krause R, et al. COVID-19 associated pulmonary aspergillosis (CAPA)—from immunology to treatment. J Fungi. 2020;6:91.
Koehler P, Bassetti M, Chakrabarti A, Chen SCA, Colombo AL, Hoenigl M et al. European Confederation of Medical Mycology; International Society for Human and Animal Mycology; Asia Fungal Working Group; INFOCUS LATAM/ISHAM Working Group; ISHAM Pan Africa Mycology Working Group; European Society for Clinical Microbiology; Infectious Diseases Fungal Infection Study Group; ESCMID Study Group for Infections in Critically Ill Patients; Interregional Association of Clinical Microbiology and Antimicrobial Chemotherapy; Medical Mycology Society of Nigeria; Medical Mycology Society of China Medicine Education Association; Infectious Diseases Working Party of the German Society for Haematology and Medical Oncology; Association of Medical Microbiology; Infectious Disease Canada. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2021; 21: 149–162.
Hoenigl M. Invasive Fungal Disease Complicating Coronavirus Disease 2019: When It Rains. It Spores Clin Infect Dis. 2021;73:1645–8.
Bartoletti M, Pascale R, Cricca M, Rinaldi M, Maccaro A, Bussini L et al.; PREDICO Study Group. Epidemiology of invasive pulmonary aspergillosis among intubated patients with COVID-19: a prospective study. Clin Infect Dis. 2021; 73: 3606–3614.
Nasri E, Shoaei P, Vakili B, Mirhendi H, Sadeghi S, Hajiahmadi S, et al. Fatal invasive pulmonary aspergillosis in COVID-19 patient with acute myeloid leukemia in Iran. Mycopathologia. 2020;185:1077–84.
Janssen NAF, Nyga R, Vanderbeke L, Jacobs C, Ergün M, Buil JB, et al. Multinational observational cohort study of COVID-19-associated pulmonary aspergillosis1. Emerg Infect Dis. 2021;27:2892–8.
van Arkel ALE, Rijpstra TA, Belderbos HNA, van Wijngaarden P, Verweij PE, Bentvelsen RG. COVID-19–associated pulmonary aspergillosis. Am J Respir Crit Care Med. 2020;202:132–5.
Rutsaert L, Steinfort N, Van Hunsel T, Bomans P, Naesens R, Mertes H, et al. COVID-19-associated invasive pulmonary aspergillosis. Ann Intensive Care. 2020;10:71.
Wang J, Yang Q, Zhang P, Sheng J, Zhou J, Qu T. Clinical characteristics of invasive pulmonary aspergillosis in patients with COVID-19 in Zhejiang, China: a retrospective case series. Crit Care. 2020;24:299.
Alanio A, Dellière S, Fodil S, Bretagne S, Mégarbane B. Prevalence of putative invasive pulmonary aspergillosis in critically ill patients with COVID-19. Lancet Respir Med. 2020;8:48–9.
Lamoth F, Glampedakis E, Boillat-Blanco N, Oddo M, Pagani JL. Incidence of invasive pulmonary aspergillosis among critically ill COVID-19 patients. Clin Microbiol Infect. 2020;26:1706–8.
White PL, Dhillon R, Cordey A, Hughes H, Faggian F, Soni S, et al. A national strategy to diagnose coronavirus disease 2019—associated invasive fungal disease in the intensive care unit. Clin Infect Dis. 2021;73:1634–44.
Dellière S, Dudoignon E, Fodil S, Voicu S, Collet M, Oillic PA, et al. Risk factors associated with COVID-19—associated pulmonary aspergillosis in ICU patients: a French multicentric retrospective cohort. Clin Microbiol Infect. 2020;27:1–5.
Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis. Thorax. 2015;70:270–7.
Heldt S, Hoenigl M. Lateral flow assays for the diagnosis of invasive aspergillosis: current status. Curr Fungal Infect Rep. 2017;11:45–51.
Mercier T, Guldentops E, Lagrou K, Maertens J. Prospective evaluation of the turbidimetric β-D-glucan assay and 2 lateral flow assays on serum in invasive Aspergillosis. Clin Infect Dis. 2021;72:1577–84.
Serin I, Dogu MH. Serum Aspergillus galactomannan lateral flow assay for the diagnosis of invasive aspergillosis: a single-centre study. Mycoses. 2021;64:678–83.
Norman G. Likert scales, levels of measurement and the “laws” of statistics. Adv Health Sci Educ Theory Pract. 2010;15:625–32.
Kariyawasam RM, Dingle TC, Kula BE, Vandermeer B, Sligl WI, Schwartz IS. Defining COVID-19-associated pulmonary aspergillosis: systematic review and meta-analysis. Clin Microbiol Infect. 2022;28:920–7.
Chong WH, Neu KP. Incidence, diagnosis and outcomes of COVID-19-associated pulmonary aspergillosis (CAPA): a systematic review. J Hosp Infect. 2021;113:115–29.
Autier B, Prattes J, White PL, Valerio M, Machado M, Price J, et al. Aspergillus lateral flow assay with digital reader for the diagnosis of COVID-19-associated pulmonary aspergillosis (CAPA): a multicenter study. J Clin Microbiol. 2022;60: e0168921.
Ghazanfari M, Yazdani Charati J, Davoodi L, Arastehfar A, Moazeni M, Abastabar M, et al. Comparative analysis of galactomannan lateral flow assay, galactomannan enzyme immunoassay and BAL culture for diagnosis of COVID-19-associated pulmonary aspergillosis. Mycoses. 2022;65:960–8.
Hoenigl M, Egger M, Boyer J, Schulz E, Prattes J, Jenks JD. Serum lateral flow assay with digital reader for the diagnosis of invasive pulmonary aspergillosis: a two-centre mixed cohort study. Mycoses. 2021;64:1197–202.
Gangneux JP, Dannaoui E, Fekkar A, Luyt CE, Botterel F, De Prost N, et al. Fungal infections in mechanically ventilated patients with COVID-19 during the first wave: the French multicentre MYCOVID study. Lancet Respir Med. 2022;10:180–90.
Acknowledgements
We are grateful to Ekin Ekici and Elif Ertas for their great contributions to the writing and reviewing of this article. We are also grateful to Ala Saglik Hizmetleri Ticaret Anonim Sirketi and Neutec Pharmaceutical Turkey for providing the necessary support for the study. Finally, we would like to thank Mehmet Toptas for his great support and efforts during the difficult academic process.
Funding
No funding was received. None of the authors has disclosures relevant to this manuscript. Neutec Pharma Limited was our sponsor for the procurement of LFA kits.
Author information
Authors and Affiliations
Contributions
I.S. and S.B. designed the study. I.S. performed the LFA procedure. T.AC., H.G., O.S. and B.D. analysed the data. I.S. and S.B. wrote the paper with input from all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical committee approval was received (Istanbul Training and Research Hospital, approval date, and number: 28/01/2022-28), and the patients or their relatives gave informed consent before the beginning of the study. The experimental procedures were based on the Declaration of Helsinki and relevant institutional regulations.
Consent for publication
Not applicable.
Competing interests
The authors declared that they do not have any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Serin, I., Baltali, S., Cinli, T.A. et al. Lateral flow assay (LFA) in the diagnosis of COVID-19-associated pulmonary aspergillosis (CAPA): a single-center experience. BMC Infect Dis 22, 822 (2022). https://doi.org/10.1186/s12879-022-07828-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07828-y