Abstract
Background
Gastrointestinal graft–versus-host disease (GvHD) is a potentially life-threatening complication after allogeneic stem cell transplantation (SCT). Since therapeutic options are still limited, a prophylactic approach seems to be warranted.
Methods
In this randomised, double-blind-phase III trial, we evaluated the efficacy of budesonide in the prophylaxis of acute intestinal GvHD after SCT. The trial was registered at https://clinicaltrials.gov, number NCT00180089.
Patients were randomly assigned to receive either 3 mg capsule three times daily oral budesonide or placebo. Budesonide was applied as a capsule with pH-modified release in the terminal ileum. Study medication was administered through day 56, follow-up continued until 12 months after transplantation. If any clinical signs of acute intestinal GvHD appeared, an ileocolonoscopy with biopsy specimens was performed.
Results
The crude incidence of histological or clinical stage 3–4 acute intestinal GvHD until day 100 observed in 91 (n =48 budesonide, n =43 placebo) evaluable patients was 12.5% (95% CI 3-22%) under treatment with budesonide and 14% (95% CI 4-25%) under placebo (p = 0.888). Histologic and clinical stage 3–4 intestinal GvHD after 12 months occurred in 17% (95% CI 6-28%) of patients in the budesonide group and 19% (CI 7-32%) in the placebo group (p = 0.853). Although budesonide was tolerated well, we observed a trend towards a higher rate of infectious complications in the study group (47.9% versus 30.2%, p = 0.085). The cumulative incidences at 12 months of intestinal GvHD stage >2 with death as a competing event (budesonide 20.8% vs. placebo 32.6%, p = 0.250) and the cumulative incidence of relapse (budesonide 20.8% vs. placebo 16.3%, p = 0.547) and non-relapse mortality (budesonide 28% (95% CI 15-41%) vs. placebo 30% (95% CI 15-44%), showed no significant difference within the two groups (p = 0.911). The trial closed after 94 patients were enrolled because of slow accrual. Within the limits of the final sample size, we were unable to show any benefit for the addition of budesonide to standard GvHD prophylaxis.
Conclusions
Budesonide did not decrease the occurrence of intestinal GvHD in this trial. These results imply most likely that prophylactic administration of budenoside with pH-modified release in the terminal ileum is not effective.
Similar content being viewed by others
Background
Acute intestinal GvHD is a frequent complication after allogeneic stem cell transplantation (SCT) and remains a major cause of morbidity and mortality. In spite of standard GvHD prophylaxis between 20 to 80% of the patients suffer from clinically relevant acute GvHD [1]-[9]. Whereas acute GvHD with affection of the skin and/or liver rarely becomes life-threatening, acute intestinal GvHD represents one of the most frequent causes of death after allogeneic SCT. Severe cases may suffer from watery stools up to a volume of several litres, bloody stools or ileus. The median survival of correspondent patients with acute GvHD grade 3 and 4 constitute between two and three months only [8]. Therefore a prophylactic approach seems to be warranted.
Budesonide has demonstrated its efficacy in the treatment of various chronic inflammatory bowel diseases [10]-[20]. It is a locally acting steroid derived from 16α-hydroxyprednisolon with strong anti-inflammatory, antiexudative and anti-oedematous characteristics. The local effect of budesonide is comparable to prednisolone [11],[15],[21]. It underlies a high first pass effect in the liver and therefore is associated with fewer side effects compared to corticosteroids with systemic efficacy. The bioavailability accounts for 9 to 12%. Some reports of the effectiveness of budesonide and other locally acting steroids in acute GvHD already exist [22],[23]. A study on the potential value of budesonide for the prophylaxis of intestinal GvHD has not been performed.
Methods
Study design and patients
The PROGAST trial, a study of budesonide as an agent for prevention of acute intestinal GvHD was a randomised, double-blind, placebo-controlled multicentre trial. The study was conducted at 3 centres from March 2003 through May 2007. The medical ethics committee of the TU Dresden and the ethics committee at Charité, Berlin approved the protocol, and all patients provided written informed consent. The trial was registered at https://clinicaltrials.gov, number NCT00180089.
Eligible male and female patients were at least 12 years of age and in preparation for related or unrelated allogeneic SCT. The stem cell donors –related or unrelated- were selected based on the compatibility for 10 HLA alleles (HLA-A, −B, −C, DRB1 and DQB1) by high-resolution (2 digit for class I, 4 digit for class II) DNA typing. One single allele mismatch was allowed within the same broad serotype or within a cross-reactive group. GvHD prophylaxis regimes followed international standards with cyclosporine A or tacrolimus in combination with methotrexate, optionally combined with anti-thymocyte globulin (ATG) or alemtuzumab.
Patients who received a T-cell-depleted graft, or who had received budesonide within 4 weeks prior to transplantation, as well as patients with local gut infections, apparent infectious disease, portal hypertension, profound liver function impairment, liver cirrhosis or severe psychiatric diseases were excluded.
Study treatment and randomisation
Patients were randomly assigned to receive either oral budesonide (Budenofalk® 3 mg, Dr. Falk Pharma GmbH, Freiburg, Germany) at a daily dose of 9 mg (3 mg TID) or placebo. Budesonide was administered as a capsule. The galenical formulation assured a drug release according to a pH >6.4 which resembles the pH in the terminal ileum. Medication started one day before allogeneic SCT and was continued until day 56. Afterwards the patients went into a follow-up period until 12 months.
Randomisation was performed centrally with the use of a randomisation procedure stratified according to the relationship of the donor (related or unrelated), conditioning regimens ( dosage reduced or intensive), and in-vivo T-cell-depletion (with or without anti-thymocyte globulin (ATG)/alemtuzumab).
Evaluation of efficacy and safety
GvHD evaluation was performed weekly starting from day 5 until day 56 after SCT and followed by visits in week 12, 16, 20, 24 and 56. Clinical signs of intestinal GvHD were classified according to Glucksberg-classification [24] of acute GvHD: occurrence of diarrhoea, bloody stools, abdominal pain, nausea and vomiting. If one of these symptoms emerged, a colonoscopy with specimens according to a standardized protocol was performed [25]. GvHD was histologically classified following Lerner's classification [26]. Monitoring for adverse events using common toxicity criteria (CTC) was performed until 12 months after transplantation.
Primary and secondary end points
The primary efficacy end point was the rate of patients with acute intestinal GvHD > stage 2 until day 100 after transplantation. Patients with histologic GvHD > grade 2 and patients with clinical signs of GvHD > stage 2 together with a positive histologic result for GvHD were classified as failures with respect to the primary end point. Secondary end points included the rate of patients with acute intestinal GvHD > stage 2 during follow-up until 12 months after transplantation, tolerability and safety of budesonide, severity of acute intestinal GvHD, incidence of chronic intestinal GvHD and infectious complications. Survival end points were overall and relapse-free survival, as well as relapse incidence and non-relapse mortality.
Study oversight
The study was jointly designed by haematologists and gastroenterologists of the University Hospital Dresden. A total of three centres participated in this trial (University Hospital Dresden, Charité-Campus Benjamin Franklin in Berlin, German Hospital for Diagnostics, Wiesbaden). Data was collected and analysed by the local Coordination Centre for Clinical Trials (KKS) in Dresden. The academic authors vouch for the veracity and completeness of the data and the data analyses.
Statistical analysis
For the primary end point, the rate of patients with acute intestinal GvHD > stage 2 after transplantation a rate of 30% for the placebo group was assumed. The expected incidence of GI GvHD seems to depend mainly on the frequency of endoscopic investigations. In fact Martin and coworkers [27] could show that the incidence of early stages of gut GvHD can be as high as 60%, especially in recipients of grafts from unrelated donors. It was calculated that 242 patients would be needed to provide a power of 80% in order to detect a difference in GvHD occurrence of 15% among the two groups (budesonide versus placebo). The software was nQuery Advisor® 7.0.
The overall incidence of acute and chronic GvHD and infectious complications were compared with the use of the chi-square test and accordingly Fisher's exact test. Efficacy analyses were performed according to the intention-to-treat principle. All patients receiving at least one dose of the study drug were included in the safety analysis. Tolerability of budesonide was assessed by means of CTC score. The comparison of overall and relapse-free survival was made with Kaplan-Meier survival analysis [28] and adjacent log-rank test between the budesonide and the placebo group. The cumulative incidence of stage 3 to 4 GI GvHD until 12 months after transplantation was calculated with death without intestinal GVHD as a competing risk [29]. Relapse incidence and non-relapse mortality were considered as competing events. Cumulative incidences were compared with the Gray test. Cross tables were analysed by means of Fisher's exact test.
Results
Patients
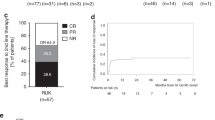
Due to a lack of sufficient patient recruitment, the protocol committee decided to terminate the study prematurely. Of the 94 patients who underwent randomisation, 48 received budesonide and 46 received placebo. Three patients assigned to the placebo group did not take any study medication (2 patients withdrew their consent; 1 patient died), thus the ITT population consisted of 91 patients. The baseline disease characteristics were similar among the two groups (Table 1) except for multiple myeloma which was more frequent in the placebo group. A total of 91 patients completed the trial (Figure 1).
Primary end point
Within the first 100 days after transplantation, a total of 6 patients (12.5%, 95% CI 3-22%) in the budesonide group and 6 patients (14%, 95% CI 4-25%) in the placebo group had experienced histologic or clinical acute intestinal GvHD > stage 2 according to Lerner's- and Glucksberg classification [24],[26] of intestinal GvHD. There was no significant difference within the two groups (p = 0.888, Table 2). With the final sample size of 91 patients the post hoc power to detect a 15% difference in a chi-square test was 31% (15% acute GvHD in the treatment arm compared to 30% acute GvHD in the placebo arm). The final sample size should only permit to reveal a difference of 25% (5% acute GvHD in the experimental arm and 30% acute GvHD in the placebo arm) with a type I error of 5% and a power of 80%.
Nevertheless if the trial would have continued to enroll and results continued on current trajectory there would be no significant difference (1.5%) within the two groups.
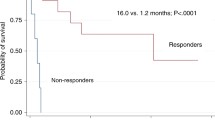
Secondary end points
The crude incidences of histologic and clinical stage 3–4 intestinal GvHD after 12 months observed in 91 (n =48 budesonide, n =43 placebo) evaluable patients were 17% (n =9, 95% CI 6-28%) in the budesonide group and 19% (n =8, 95% CI 7-32%) in the placebo group (p = 0.853). The cumulative incidences at 12 months of intestinal GvHD stage >2 with death as a competing event (budesonide 20.8% vs. placebo 32.6%, p = 0.250) and the cumulative incidence of relapse (budesonide 20.8% vs. placebo 16.3%, p = 0.547) and non-relapse mortality ( budesonide 28% (95% CI 15-41%) vs. placebo 30% (95% CI 15-44%), showed no significant difference within the two groups ( p = 0.911, Figures 2 and 3).
Through month 12, the incidences of adverse events (AE) and severe adverse events (SAE) were similar among the two groups (Table 3). Every patient in the budesonide group (100%) and 97.7% in the placebo group had at least one adverse event. Classified by the CTC score, budesonide was tolerated. There was a statistically insignificant trend to a higher rate of overall infectious complications until month 12 in the budesonide group (47.9%) compared to placebo (30.2%), but there was no difference in the rate of gastrointestinal infections (placebo 4.6% vs. budesonide 4.4%). Further on a statistically insignificant trend to a higher overall survival (72.9% budesonide, 62.8% placebo) in the budesonide group was observed.
The incidence of chronic intestinal GvHD showed a higher percentage in the placebo group (budesonide 6.3% (n = 3), placebo 11.6% (n = 5), but failed to reach significance.
The distribution of the severity stages of acute intestinal GvHD, as well as incidence and severity stages of skin, liver and grades of overall GvHD showed no difference between the two groups.
Discussion
GI GvHD remains a huge problem, with few therapeutic options. Acute GvHD is mediated by immunocompetent donor T cells, which migrate to lymphoid tissues soon after allogeneic stem cell transplantation. In the light of the high mortality of severe GI GvHD which often does not respond to steroid therapy, alternative treatments are being actively investigated. Besides the options of in-vivo or in-vitro T-cell-depletion, a prophylactic pharmacologic approach seems to be the most promising. Ideally, prophylactic treatment should not affect transplantation associated mortality and the incidence of relapse. T-cell-depleted grafts effectively reduce the risk of acute GvHD but are associated with a higher relapse rate because of the missing Graft-versus-leukemia effect. An intensified pharmacologic prophylaxis has been associated with an increase in the relapse rate, a higher rate of systemic infections and a late recurrence of GvHD.
A prophylactic approach with budesonide asa locally acting immunosuppressive treatment seems to be attractive because of a lower risk of systemic complications during therapy, as seen in patients with chronic inflammatory bowel disease. Underlying rationale is a strong anti-inflammatory local effect of budesonide on the one hand and a high first pass effect in the liver of more than 90%, which leads to negligible systemic effects on the other hand.
Even though the present study suggests that oral budesonide is not effective for the prevention of acute intestinal GvHD, early intervention in patients with a high-risk of gastrointestinal GvHD still seems to be an attractive strategy.
Furthermore it should be taken into account that the applied galenic formulation of budesonide has its maximum effect in the terminal ileum and right-sided colon. This is based on the pH-modified release of oral budesonide and therefore it is not adequate for prophylaxis of intestinal GvHD in the jejunum or proximal ileum. Some open-label studies showed efficacy in distal ulcerative colitis, but this finding has to be confirmed in controlled trials [30]. Therefore it remains unclear, if budesonide has a sufficient effect in the prophylaxis of GvHD in the distal colon.
Besides pharmacokinetic analyses suggest that a single dose of 9 mg budesonide may lead to a higher local concentration of budesonide compared to 3 mg three times per day [31] as performed in this study and therefore, could increase the therapeutic potential.
Overall infectious complications showed a trend to a higher frequency in the budesonide group, but gastrointestinal infections were equal in both groups and reflect better potentially side effects of locally acting budesonide.
As an additional second endpoint there was also no difference in the incidence of liver involvement, a site where the first-pass effect would lead to the assumption of a local efficacy of the study compound.
Conclusion
In summary, this study failed to show a significant effect of prophylactic treatment with oral budesonide in preventing gastrointestinal GvHD. This study was closed prematurely because of slow accrual. Within the limitations of the sample size, no significance difference in outcomes were able to be detected in primary and secondary outcomes.
Authors' contributions
RS coordinated the study, performed statistical analysis and drafted the manuscript. MB conceived of the study, and participated in its design and coordination and helped to draft the manuscript. JS performed the statistical analysis and helped to draft the manuscript. AK helped to draft the manuscript.UP helped to draft the manuscript. US performed the statistical analysis. XG performed the statistical analysis. LU participated in the study design. DA performed histology. GB performed histology. RS participated in the study design. JH helped to draft the manuscript. RG participated in the study design. RM participated in the study design. GE conceived of the study and participated in its design. SM conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
References
Deeg HJ, Antin JH: The clinical spectrum of acute graft-versus-host disease. Semin Hematol. 2006, 43 (1): 24-31. 10.1053/j.seminhematol.2005.09.003.
Washington K, Jagasia M: Pathology of graft-versus-host disease in thegastrointestinal tract. Hum Pathol. 2009, 40 (7): 909-917. 10.1016/j.humpath.2009.04.001.
Gratwohl A, Hermans J, Apperley J, Arcese W, Bacigalupo A, Bandini G, di Bartolomeo P, Boogaerts M, Bosi A, Carreras E: Acute graft-versus-host disease: grade and outcome in patients with chronic myelogenous leukemia. Working party chronic leukemia of the european group for blood and marrow transplantation. Blood. 1995, 86 (2): 813-818.
Nash RA, Pepe MS, Storb R, Longton G, Pettinger M, Anasetti C, Appelbaum FR, Bowden RA, Deeg HJ, Doney K: Acute graft-versus-host disease: analysis of risk factors after allogeneic marrow transplantation and prophylaxis with cyclosporine and methotrexate. Blood. 1992, 80 (7): 1838-1845.
Ratanatharathorn V, Nash RA, Przepiorka D, Devine SM, Klein JL, Weisdorf D, Fay JW, Nademanee A, Antin JH, Christiansen NP, van der Jagt R, Herzig RH, Litzow MR, Wolff SN, Longo WL, Petersen FB, Karanes C, Avalos B, Storb R, Buell DN, Maher RM, Fitzsimmons WE, Wingard JR: Phase III study comparing methotrexate and tacrolimus (prograf, FK506) with methotrexate and cyclosporine for graft-versus-host disease prophylaxis after HLA-identical sibling bone marrow transplantation. Blood. 1998, 92 (7): 2303-2314.
Vogelsang GB, Arai S: Mycophenolate mofetil for the prevention and treatment of graft-versus-host disease following stem cell transplantation: preliminary findings. Bone Marrow Transplant. 2001, 27 (12): 1255-1262. 10.1038/sj.bmt.1703076.
Weisdorf D, Haake R, Blazar B, Miller W, McGlave P, Ramsay N, Kersey J, Filipovich A: Treatment of moderate/severe acute graft-versus-host disease after allogeneic bone marrow transplantation: an analysis of clinical risk features and outcome. Blood. 1990, 75 (4): 1024-1030.
Nevo S, Enger C, Swan V, Wojno KJ, Fuller AK, Altomonte V, Braine HG, Noga SJ, Vogelsang GB: Acute bleeding after allogeneic bone marrow transplantation: association with graft versus host disease and effect on survival. Transplantation. 1999, 67 (5): 681-689. 10.1097/00007890-199903150-00007.
Ferrara JL, Deeg HJ: Graft-versus-host disease. N Engl J Med. 1991, 324: 667-674. 10.1056/NEJM199103073241005.
Seow CH, Benchimol EI, Steinhart AH, Griffiths AM, Otley AR: Budesonide for Crohn's disease. Expert Opin Drug Metab Toxicol. 2009, 5 (8): 971-979. 10.1517/17425250903124355.
Campieri M, Ferguson A, Doe W, Persson T, Nilsson LG: Oral budesonide is as effective as oral Prednisolone in active Crohn's disease. The global budesonide study group. Gut. 1997, 41 (2): 209-214. 10.1136/gut.41.2.209.
Ferguson A, Campieri M, Doe W, Persson T, Nygård G: Oral budesonide as maintenance therapy in Crohn's disease-results of a 12-month study. Global budesonide study group. Aliment Pharmacol Ther. 1998, 12 (2): 175-183. 10.1046/j.1365-2036.1998.00285.x.
Greenberg GR, Feagan BG, Martin F, Sutherland LR, Thomson AB, Williams CN, Nilsson LG, Persson T: Oral budesonide as maintenance treatment for Crohn's disease: a placebo-controlled, dose-ranging study. Gastroenterology. 1996, 110 (1): 45-51. 10.1053/gast.1996.v110.pm8536887.
Hellers G, Cortot A, Jewell D, Leijonmarck CE, Löfberg R, Malchow H, Nilsson LG, Pallone F, Pena S, Persson T, Prantera C, Rutgeerts P: Oral budesonide for prevention of postsurgical recurrence in Crohn's disease. Gastroenterology. 1999, 116 (2): 294-300. 10.1016/S0016-5085(99)70125-3.
Löfberg R, Danielsson A, Suhr O, Nilsson A, Schiöler R, Nyberg A, Hultcrantz R, Kollberg B, Gillberg R, Willén R, Persson T, Salde L: Oral budesonide versus Prednisolone in patients with active extensive and left-sided ulcerative colitis. Gastroenterology. 1996, 110 (6): 1713-1718. 10.1053/gast.1996.v110.pm8964395.
Miehlke S, Heymer P, Bethke B, Bästlein E, Meier E, Bartram HP, Wilhelms G, Lehn N, Dorta G, DeLarive J, Tromm A, Bayerdörffer E, Stolte M: Budesonide treatment for collagenous colitis: a randomized, double-blind, placebo-controlled, multicenter trial. Gastroenterology. 2002, 123 (4): 978-984. 10.1053/gast.2002.36042.
Miehlke S, Madisch A, Karimi D, Wonschik S, Kuhlisch E, Beckmann R, Morgner A, Mueller R, Greinwald R, Seitz G, Baretton G, Stolte M: Budesonide is effective in treating lymphocytic colitis: a randomized double-blind placebo-controlled study. Gastroenterology. 2009, 136 (7): 2092-2100. 10.1053/j.gastro.2009.02.078.
McDonald GB: Oral beclomethasone dipropionate: a topically active corticosteroid for the treatment of gastrointestinal graft-versus-host disease following allogeneic hematopoietic cell transplantation. Expert Opin Investig Drugs. 2007, 16 (10): 1709-1724. 10.1517/13543784.16.10.1709.
McKeage K, Goa KL: Budesonide (Entocort EC Capsules): a review of its therapeutic use in the management of active Crohn's disease in adults. Drugs. 2002, 62 (15): 2263-2282. 10.2165/00003495-200262150-00015.
Rutgeerts P, Löfberg R, Malchow H, Lamers C, Olaison G, Jewell D, Danielsson A, Goebell H, Thomsen OO, Lorenz-Meyer H, Hodgson H, Persson T, Seidegard C: A comparison of budesonide with prednisolone for active Crohn's disease. N Engl J Med. 1994, 331 (13): 842-845. 10.1056/NEJM199409293311304.
Brogden RN, McTavish D: Budesonide. An updated review of its pharmacological properties, and therapeutic efficacy in asthma and rhinitis. Drugs. 1992, 44 (3): 375-407. 10.2165/00003495-199244030-00007. Erratum in: Drugs. 1992 Dec;44(6):1012. Drugs. 1993 Jan;45(1):1301
Bertz H, Afting M, Kreisel W, Duffner U, Greinwald R, Finke J: Feasibility and response to budesonide as topical corticosteroid therapy for acute intestinal GVHD. Bone Marrow Transplant. 1999, 24 (11): 1185-1189. 10.1038/sj.bmt.1702055.
McDonald GB, Bouvier M, Hockenbery DM, Stern JM, Gooley T, Farrand A, Murakami C, Levine DS: Oral beclomethasone dipropionate for treatment of intestinal graft-versus-host disease: a randomized, controlled trial. Gastroenterology. 1998, 115 (1): 28-35. 10.1016/S0016-5085(98)70361-0.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, Lerner KG, Thomas ED: Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974, 18 (4): 295-304. 10.1097/00007890-197410000-00001.
Cruz-Correa M, Poonawala A, Abraham SC, Wu TT, Zahurak M, Vogelsang G, Kalloo AN, Lee LA: Endoscopic findings predict the histologic diagnosis in gastrointestinal graft-versus-host disease. Endoscopy. 2002, 34 (10): 808-813. 10.1055/s-2002-34257.
Lerner KG, Kao GF, Buckner CD, Clift RA, Thomas ED: Histopathology of graft-vs.-host reaction (GvHR) in human recipients of marrow from HL-A-matched sibling donors. Transplant Proc. 1974, 6: 367-371.
Martin PJ, McDonald GB, Sanders JE, Anasetti C, Appelbaum FR, Deeg HJ, Nash RA, Petersdorf EW, Hansen JA, Storb R: Increasingly frequent diagnosis of acute gastrointestinal graft-versus-host disease after allogeneic hematopoietic celltransplantation. Biol Blood Marrow Transplant. 2004, 10 (5): 320-327. 10.1016/j.bbmt.2003.12.304.
Kaplan E, Meier P: Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958, 53: 457-462. 10.1080/01621459.1958.10501452.
Lin DY: Non-parametric inference for cumulative incidence functions in competing risks studies. Stat Med. 1997, 16: 901-910. 10.1002/(SICI)1097-0258(19970430)16:8<901::AID-SIM543>3.0.CO;2-M.
Gross V: Oral pH-modified release budesonide for treatment of inflammatory bowel disease, collagenous and lymphocytic colitis. Expert Opin Pharmacother. 2008, 9 (7): 1257-1265. 10.1517/14656566.9.7.1257.
Kolkman JJ, Möllmann HW, Möllmann AC, Penã AS, Greinwald R, Tauschel HD, Hochhaus G: Evaluation of oral budesonide in the treatment of active distal ulcerative colitis. Drugs Today (Barc). 2004, 40 (7): 589-601. 10.1358/dot.2004.40.7.850477.
Acknowledgements
The study was partly supported by Dr. Falk Pharma GmbH, Freiburg, Germany.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
R. Schmelz has received honoraria for clinical studies and lecture fees from Dr. Falk Pharma GmbH.
M. Bornhäuser has received lecture honoraria from Novartis, Roche and Celgene.
J. Schetelig: has received lecture honoraria from Roche, Genzyme and GSK.
A. Kiani: no financial relationship.
U. Platzbecker has received lecture honoraria from Novartis, Amgen and Celgene.
U. Schwanebeck has received grant/research support for clinical trials from Ardeypharm GmbH, Smith & Nephew, UCB Pharma:Spouse/Partner, Pharmion GmbH, GlaxoSmithKline, Otsuka Frankfurt Research Institute, Support;Bristol-Myers Squibb Co. , Sanofi-Aventis, Support;TEVA, Novartis Pharma GmbH, Apogepha Pharma, GABA, Dr. Falk Pharma GmbH
X. Grählert has received grant/research support for clinical trials from Dr. Falk Pharma GmbH, GABA, Novartis, TEVA, Sanofi-Aventis, Bristol-Myers Squibb, Otsuka, GlaxoSmithKline, Pharmion, UCB Pharma, Smith & Nephew.
L. Uharek: no financial relationship
D. Aust has received lecture fees from Dr. Falk Pharma.
G. Baretton: no financial relationship.
R. Schwerdtfeger: no financial relationship.
J. Hampe: has received lecture honoraria from Dr. Falk Pharma GmbH and grant funding from Metanomics / BASF and Bayer AG.
R. Greinwald is an employee of Dr. Falk Pharma GmbH.
R. Mueller is an employee of Dr. Falk Pharma GmbH.
G. Ehninger: no financial relationship.
S. Miehlke has received honoraria for clinical studies, advisory boards, and lecture fees from Dr. Falk Pharma GmbH.
The trial was in part supported by Dr. Falk Pharma GmbH.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited.
About this article
Cite this article
Schmelz, R., Bornhäuser, M., Schetelig, J. et al. Randomised, double-blind, placebo-controlled trial of oral budesonide for prophylaxis of acute intestinal graft-versus-host disease after allogeneic stem cell transplantation (PROGAST). BMC Gastroenterol 14, 197 (2014). https://doi.org/10.1186/s12876-014-0197-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-014-0197-7