Abstract
Background
Over the last 20 years, integrated care programs for frail elderly people aimed to prevent functional dependence and reduce hospitalization and institutionalization. However, results have been inconsistent and merely modest. To date, evidence on the cost-effectiveness of these programs is scarce. We evaluated the cost-effectiveness of the CareWell program, a multicomponent integrated care program for frail elderly people.
Methods
Economic evaluation from a healthcare perspective embedded in a cluster controlled trial of 12 months in 12 general practices in (the region of) Nijmegen. Two hundred and four frail elderly from 6 general practices in the intervention group received care according to the CareWell program, consisting of multidisciplinary team meetings, proactive care planning, case management, and medication reviews; 165 frail elderly from 6 general practices in the control group received usual care. In cost-effectiveness analyses, we related costs to daily functioning (Katz-15 change score i.e. follow up score minus baseline score) and quality adjusted life years (EQ-5D-3 L).
Results
Adjusted mean costs directly related to the intervention were €456 per person. Adjusted mean total costs, i.e. intervention costs plus healthcare utilization costs, were €1583 (95% CI -4647 to 1481) higher in the intervention group than in the control group. Incremental Net Monetary Benefits did not show significant differences between groups, but on average tended to favour usual care.
Conclusions
The CareWell primary program was not cost-effective after 12 months. From a cost-effectiveness perspective, widespread implementation of the program in its current form cannot be recommended.
Trial registration
The study was registered in the ClinicalTrials.govProtocol Registration System: (NCT01499797; December 26, 2011). Retrospectively registered.
Similar content being viewed by others
Background
Frail elderly account for a disproportionally large share of healthcare costs, spending over $70,000/year in 2011 in the United States, with particularly high expenditure on in-patient and post-acute care [1, 2]. In the Western world, the prevalence of frailty - a state of increased vulnerability to adverse outcomes through a complex interplay of physical, psychological, social and environmental factors [3] – will even increase due to population ageing, since frailty is thought to be present in 10% of people aged ≥65 years up to 25%–50% of people aged ≥85 years [4, 5]. Western countries are forced to adapt their healthcare policies addressing frail elderly in order to achieve cost reductions in health and social services and maintain financial sustainability.
Proactive integrated care programs, addressing the complex and interacting healthcare and welfare needs, are thought to have the potential to prevent adverse outcomes and lower healthcare costs [6, 7]. However, results so far have shown merely modest, inconsistent results regarding their effectiveness and efficiency [8,9,10,11,12]. Some studies pointed out the potential to prevent hospitalization and nursing home admissions [10, 11, 13], but accompanying increases in home care and social services use might impede overall cost savings [8, 10, 14]. Formal economic evaluations of integrated programs targeting frail elderly are scarce [15, 16]. Moreover, heterogeneity between studies regarding target population (age, low or high risk of functional decline), context (home-, primary care- or institution based), and intervention components hinder comparability and generalizability. Moreover, results of economic evaluations need to be interpreted in the light of national contexts [17].
In the Netherlands, the Dutch Ministry of Health, Welfare and Sports initiated the National Care for the Elderly Program in 2008, in which over 650 organizations in health, welfare and housing work together in eight regional networks led by academic medical centres to improve care for elderly people with complex care needs. As part of this program, we developed the CareWell primary care program that aimed to reduce functional decline, institutionalization, and hospitalization of community-dwelling frail elderly. Although effectiveness of the program could not be demonstrated [18], the program might theoretically save overall costs and, depending on the trade-off between costs and effects, might be cost-effective. Therefore, we conducted a separate economic evaluation to answer the following research questions:
-
What are the differences in health care costs between participants receiving care according to the CareWell primary care program and those receiving care as usual?
-
Is the CareWell primary care program cost-effective from a healthcare perspective after 12 months?
Methods
Design
This economic evaluation from a healthcare perspective was performed alongside a cluster controlled effectiveness study with a follow-up of 12 months. Design, methods and outcomes of the effectiveness study have been reported elsewhere [18].
Setting and participants
The study was conducted between September 2011 and September 2012 in 12 general practitioner (GP) practices in the region of Nijmegen, the Netherlands. After informed consent, frail elderly aged ≥70 years were included with the use of the EASY-Care TOS instrument [19]: First, GPs use prior knowledge to subdivide ‘not frail’ from ‘(possibly) frail’ elders. Then, trained nurses perform a comprehensive geriatric assessment of (possible) frail elders during a home visit. Last, GPs and nurses weigh all signs into a final frailty judgment. Exclusion criteria were institutionalization, and/or critical or terminal illnesses. Details on the recruitment and informed consent procedures have been reported previously [18, 20].
Intervention
In brief, the CareWell primary care program consisted of four key components: 1) multidisciplinary team (MDT) meetings, 2) proactive care planning, 3) case management, and 4) medication reviews.
Each practice assembled a MDT consisting of a general practitioner (GP), practice nurse(s) and/or community nurse(s), an elderly care physician (ECP) [21], and a social worker with elderly care expertise. Each participant was discussed in a MDT meeting at least half-yearly, more often if needed. Meetings were planned every 4–8 weeks. Tailor-made proactive care plans, based on the individual health-related problems and goals as assessed with the EASY-Care TOS [19], were formulated for each participant on enrolment in the program and revised after discussion in a MDT meeting at least every 6 months. A case manager, either a nurse or social worker, was assigned to each participant. They were responsible for care planning and coordination, patient-support in goal setting and self-management, and caregivers support. Last, the GP and nurse conducted a yearly medication review in collaboration with a pharmacist for each participant with polypharmacy (use of ≥5 chronically prescribed drugs).
Professionals received financial reimbursement to cover time-investment and overhead costs.
Usual care
In the Netherlands, GPs provide continuous, person-centred care to community-dwelling frail elderly, facilitated by the use of high-standard electronic medical records and patient panels, defining the population under care [22, 23]. GPs often collaborate with practice and/or community nurses. Moreover, elderly care physicians, i.e. medical practitioners that are specialized as primary care experts in geriatric medicine, increasingly operate (as consultants) in the care for community-dwelling frail elderly [21]. However, the coordination between GPs, other primary and specialist care providers, and home care and community services is often perceived to be insufficient, leading to a fragmented delivery of care [24].
GPs in the usual care group were explicitly asked to decline new relevant inter professional collaborations during the intervention period. No restrictions on pre-existing collaborations between GPs and (practice) nurses were imposed.
Outcome measures
Dependence in functioning in (instrumental) activities of daily living (measured with the Katz-15 [25] change score, i.e. follow-up score minus baseline score) and health-related quality of life (measured with the EuroQol five-dimensional three-level instrument (EQ-5D-3 L) [26]) were collected at baseline and at follow-up after 12 months by structured interviews by trained nurses. The Katz-15 score ranges from 0 to 15 points with higher scores indicating more dependence in (instrumental) activities of daily living. The EQ-5D-3 L instrument is a ‘preference-based’ measure of health status [27], that defines health-related quality of life according to five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) at three levels (no problems, some problems, severe problems) [26]. In line with the guidelines of the National Care for the Elderly Program, we used the modified EQ-5D + C-3 L instrument that includes cognitive functioning as an additional dimension, with a similar operationalization at three levels [28]. To date, to the best of our knowledge, there is no validated weighting formula for the EQ-5D + C-3 L. Utilities, reflecting the relative desirability of each health state, were thus calculated for the EQ-5D-3 L, without the cognitive dimension, using the Dutch tariff [29]. EQ-5D-3 L scores range from − 0.33 to 1.00, with a higher score indicating a higher health status. Quality Adjusted Life Years (QALYs) were then calculated by multiplying the utilities by the amount of time spent in a particular health state. 1 QALY represents 1 year in perfect health [29].
Healthcare utilization costs and intervention costs
We assessed intervention costs and healthcare utilization during the follow up period. [17] An overview of the healthcare cost variables, prices per unit and sources are presented in Table 1.
Intervention costs regarding time spent on team meetings, care planning, case management, and medication reviews were assessed by instructing practice and/or community nurses and social workers to fill in monthly time registration forms at participant level. To stimulate uniformity in and compliance with time registrations, structured timesheets with written instructions were sent each month as reminders. GPs and ECPs estimated their mean time spent on the intervention per GP practice, from which invested time per participant was calculated. Pharmacists estimated a time investment of 30 min per participant per medication review.
Healthcare utilization variables, i.e. GP care, hospital care, institutionalization (i.e. nursing home admission, care home admission), home care, and physiotherapy were individually assessed at baseline and follow up through a structured interview by the nurse. Data on domestic care and day care were individually extracted from registries from the municipality of Nijmegen and welfare organizations. Last, data on medication costs (both reimbursed and non-reimbursed) were individually extracted from the electronic patient files (EPF).
Costs were calculated by multiplying volumes of care with their corresponding unit prices. In calculating costs of time invested by practice and/or community nurses and social workers we used their Collective Agreements. The thus generated hourly wages were raised with an estimated 45% for employers and overhead expenses and thus set on €30, €27, and €32 respectively [30]. We used hourly wages of €103, €103, and €85 in calculating costs of time invested by the GPs, ECPs, and pharmacists respectively, according to the fixed rates of the Dutch Healthcare Authority. Costs of healthcare utilization were valued according to the Dutch manual for costing research [30]. When no standardized unit cost prices were available, costs were derived from the Dutch Healthcare Authority. Medication costs were valued using prices of the Royal Dutch Society for Pharmacy [31], using minimum cost prices. All costs were presented in Euros, and indexed to the year 2011 using the consumer price index.
Statistical analysis
Katz-15 change scores and EQ-5D-3 L scores were analyzed using mixed model multilevel analyses, accounting for clustering of participants within GP practices and correcting for those variables that differed between groups at baseline and correlated to the primary outcome, as well as for baseline Katz-15 and EQ-5D-3 L scores to account for regression to the mean [18]. Quality adjusted life years (QALYs) were derived from the EQ-5D-3 L using the trapezium rule (i.e. an approximation of the area under the QALY curve). Mean healthcare utilization costs were analyzed with descriptive statistics and compared between groups using multilevel mixed model analyses, adjusting for clustering of participants within GP practices and for relevant covariates. The incremental Net Monetary Benefit (iNMB) statistic was used to evaluate cost-effectiveness [32] and consequently used as the dependent variable in the mixed model. The iNMB prevents several statistical drawbacks of an incremental cost-effectiveness ratio and enables the use of multilevel regression techniques including covariates in a convenient way [17]. It indicates the monetary gains or costs of an intervention at explicit Willingness to Pay (WTP) thresholds per gained unit of effect. In formula: iNMB = (WTP * ∆ effects) – ∆ costs. An iNMB (and 95% lower-level confidence interval) greater than zero indicates significant cost-effectiveness of the intervention. We used five WTP thresholds per point improvement on the Katz-15 change score, i.e. €0, €5000, €10,000, €15,000, and €20,000, where no reference values were readily available. Six commonly used WTP thresholds per QALY were used: €0, €20,000, €40,000, €60,000, €80,000, and €100,000 [33].
Results
Participants
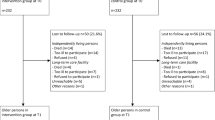
In total, 536 participants (287 in the intervention group resp. 249 in the control group) were included in the effectiveness study [18]. At baseline, participants in the intervention group significantly more often lived alone, had more health-related limitations in social functioning, more cognitive deficits, and more social disadvantage, but showed less complex care [18]. No significant between-group differences in baseline Katz-15 scores and EQ-5D-3 L scores were found. We had a loss to follow up of 28.9% participants in the intervention group and 33.7% in the control group, mainly due to death, institutionalization and declined consent for follow-up (Fig. 1). Additionally, we encountered a considerable number of missing cost variables, mainly medication cost data due to declined consent for use of EPF medication data and limited coverage of medication data in the EPFs. We adhered a complete case analysis with regard to missing values [34]. We analyzed costs and iNMB both with and without medication cost data, including 148 (51.6%) resp. 182 (63.4%) participants in the intervention group and 103 (41.3%) resp. 146 (58.6%) participants in the control group (Fig. 1), and considered the analyses including medication costs as the primary analysis. Participants included in the economic evaluation had a lower frailty index. This frailty index was calculated based on the accumulation of deficits in health (symptoms, morbidities, and/or functional abilities), and was used as an extra indicator of frailty next to the EasyCare-TOS [28]. It theoretically ranges from 0 (no indication of frailty) to 1 (extreme frailty), though frailty index scores in similar studies typically culminate at 0.7.Therefore, in addition to the covariates included in the effectiveness analysis, the frailty index was included as a covariate in this economic evaluation.
Outcome measures
At 12 months, we found no significant differences in functional dependence (adjusted mean difference of 0.37, 95% CI -0.1 to 0.8) nor QALYs (adjusted mean difference of − 0.031, 95% CI -0.1 to 0.0) between the intervention and control group, but the control group did show less functional decline (Table 2) [18].
Healthcare utilization costs and intervention costs
Mean intervention costs, adjusted for clustering and relevant covariates, were €456 (95% CI -512 to − 398). In the intervention group, mean total costs, i.e. intervention costs plus healthcare utilization costs, adjusted for clustering and relevant covariates, were €1583 (95% CI -4647 to 1481) higher than in the control group. Mean adjusted healthcare utilization costs, i.e. without the intervention costs, were €1143 (95% CI -4198 to 1912) higher in the intervention group. Of the healthcare utilization variables, only medication costs differed significantly, although mean costs of hospitalization, institutionalization, home care and physiotherapy in the intervention group exceeded those in the control group (Table 2).
Economic analysis
Figure 2 shows the iNMBs. It can be noticed that generally these iNMBs are negative, meaning that the intervention does not provide value for money compared to usual care, although the results are not significant. Sensitivity analysis, excluding medication costs, underlined these results.
Incremental net monetary benefits (in Euros) against WTP for Katz-15 change score* and QALY. Upper panels show the incremental net monetary benefits (in formula: iNMB = (WTP * ∆ effects) – ∆ costs) against WTP for Katz-15 change scores; lower panels show iNMBs against WTP for QALY. All iNMBs are negative, i.e. the intervention does not provide value for money compared to usual care (not significant). Sensitivity analyses, excluding medication costs, underline the results (right panels)WTP = Willingness to Pay. QALY = Quality Adjusted Life Year, derived from the EQ-5D-3 L, based on the Dutch tariff [29] using the trapezium rule.* Improvement on the Katz-15 change score is indicated by a lower score, meaning less functional decline regarding (instrumental) activities of daily living
Discussion
In this cluster controlled study with a follow up of 12 months, healthcare utilization costs and cost-effectiveness of the CareWell primary care program was compared to usual care. Earlier, effectiveness of the CareWell program on daily functioning and quality of life could not be demonstrated [18]. In this study, we found no statistically significant differences between groups in total costs and healthcare utilization costs, with the exception of higher medication costs in the intervention group. Moreover, cost-effectiveness analyses showed no significant differences between groups, but tended to favour usual care.
There are some possible explanations for the absence of cost-effectiveness. First, there is still a lively debate on the concept of frailty and the right timing of interventions [35, 36]. Possibly, the targeted population was too heterogeneous or, in part, too frail to respond to the intervention. Second, the Katz-15 index, measuring daily functioning, might be too restricted to capture the effects of our heterogeneous intervention. Possibly, more person- or goal centred outcomes, e.g. goal-attainment scaling, might suit better [37]. Moreover, the sensitivity to change of the EQ-5D-3 L in frail elders might have been (too) low [38]. The concept of ‘capability wellbeing’ has recently been suggested as an alternative, more sensitive measure [33]. However, further work on the validity and value of these capability indices in economic evaluations is needed [33, 39]. Third, it is likely that more profound effects of the intervention only become apparent after a longer follow up period that exceeds the time needed for implementation, individual and organizational learning effects, and efficient multidisciplinary collaboration [40, 41]. This lag-time in effectiveness is presumed to be even more important in complex interventions like our program [40]. Awareness to these short-run inefficiencies that might have resulted from the time limits set by the National Care for the Elderly Program is needed. Last, the selection of motivated professionals in the intervention group might have limited the room for improvement in the delivered care and possibly led to higher costs due to more proactive care, irrespective of the CareWell program. The overall increased awareness to the health care needs of frail elderly in Western countries in the last two decades together with the Dutch high-quality primary care might have further reduced the contrasts between the CareWell program and usual care. Possibly, our program would show clearer effectiveness in less well managed healthcare settings [12].
Our results are in line with comparable integrated care programs aimed at frail elderly, performed in other contexts [14, 42]. More recently, three cost-effectiveness studies of integrated care programs from the National Care for the Elderly Program demonstrated no effects on functioning nor quality of life, at unchanged or higher total costs mainly due to increased GP care and intervention costs without (expected) decreases in hospital and long-term care costs, after 12–24 months [43,44,45]. However, Van Leeuwen et al. did find increasing effects at lower costs compared to usual care in the last 18–24 months of follow up [45]. Previously, Counsell et al. demonstrated similar decreased costs in their third year of follow up, mainly through a shift away from emergency and hospital services towards more-desirable chronic and preventive care expenditures [14]. This supports our assumption of a lag-time in effectiveness. The results of the cost-utility analyses of the recent other Dutch studies, finding low probabilities of the intervention increasing QALYs at lower costs, correspond with our results [45, 46]. However, only Van Leeuwen et al. performed a formal cost-effectiveness analysis [45]. Like us, they found low probabilities of the intervention being cost-effective.
This study has several strengths. First, we used a comprehensive approach to costing, including a wide variety of cost variables that were assessed at participant level, thus enhancing internal validity. Next, robust multilevel techniques were used in analyzing both differences in costs and net monetary benefits. Last, since we used only a limited number of exclusion criteria and included participants from heterogeneous GP practices, our results should be generalizable to the population of frail elders in the Netherlands and comparable high-quality primary care settings.
We also should consider some limitations. First, we were unable to include informal care costs, since informal caregivers’ willingness to participate was low and differed between groups. We were therefore not able to adhere to the societal perspective, as announced in our study protocol [20], but had to switch to a healthcare perspective. Since prior studies show contrasting results on the impact of informal care on total costs, the impact of this switch on our results is unclear [42, 45]. Next, since the extraction of data on healthcare use from external sources like healthcare insurance companies, as originally planned in the study design, was not possible, we had to collect these data through participants’ retrospective self-report. This could have led to recall bias. Different studies showed self-report after 12 months to be an appropriate, reasonably accurate method for obtaining a wide range of healthcare utilization data in elderly people [47, 48]. More salient events in general suffer less from memory decay and thus recall bias [49]. Seidl et al. for example found the recall bias of hospital admissions of elderly people not to be influenced by applying various recall periods, although the probability of correctly self-reporting a single event was higher using a shorter recall period [48]. However, less salient events such as GP contacts could lead to both under- and over-reporting, and show less accuracy in self-report [49, 50]. Also, time registrations used to calculate intervention costs might be biased due to inaccuracies. However, we have no reason to assume unequal distributions of these potential biases between the groups. Last, we had to deal with a considerable number of missing medication cost data that had to be considered missing not at random. However, our additional sensitivity analysis without medication costs did not reveal other results.
Conclusions
After 12 months follow-up, no net monetary benefit of the CareWell program over usual care could be demonstrated.
This study adds to the currently scarce body of evidence regarding cost-effectiveness of integrated care programs targeting frail elderly. Future economic evaluations should account for pitfalls in their design with respect to the target population, outcome measures used, and adequate follow-up period. From a cost-effectiveness perspective, the CareWell primary program in its current form is not suited for widespread implementation.
Abbreviations
- ECP:
-
Elderly care physician
- EPF:
-
Electronic patient file
- EQ-5D-3 L:
-
EuroQol five-dimensional three-level instrument
- GP:
-
General practitioner
- iNMB:
-
Incremental net monetary benefit
- MDT:
-
Multidisciplinary team
- QALY:
-
Quality adjusted life years
- WTP:
-
Willingness to pay
References
Ganguli I, Thompson RW, Ferris TG. What can five high cost patients teach us about healthcare spending? Healthcare (Amsterdam, Netherlands). 2016;
Joynt KE, Figueroa JF, Beaulieu N, Wild RC, Orav EJ, Jha AK. Segmenting high-cost Medicare patients into potentially actionable cohorts. Healthcare (Amsterdam, Netherlands) 2016.
De Lepeleire J, Iliffe S, Mann E, Frailty DJM. An emerging concept for general practice. Br J Gen Pract. 2009;59(562):e177–82.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62.
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–92.
Clarkson P, Brand C, Hughes J, Challis D. Integrating assessments of older people: examining evidence and impact from a randomised controlled trial. Age Ageing. 2011;40(3):388–91.
Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health aff (Project Hope). 2001;20(6):64–78.
Markle-Reid M, Browne G, Weir R, Gafni A, Roberts J, Henderson SR. The effectiveness and efficiency of home-based nursing health promotion for older people: a review of the literature. Med Care Res Rev. 2006;63(5):531–69.
Eklund K, Wilhelmson K. Outcomes of coordinated and integrated interventions targeting frail elderly people: a systematic review of randomised controlled trials. Health Soc Care Community. 2009;17(5):447–58.
Beland F, Bergman H, Lebel P, Clarfield AM, Tousignant P, Contandriopoulos AP, Dallaire L. A system of integrated care for older persons with disabilities in Canada: results from a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2006;61(4):367–73.
Bernabei R, Landi F, Gambassi G, Sgadari A, Zuccala G, Mor V, Rubenstein LZ, Carbonin P. Randomised trial of impact of model of integrated care and case management for older people living in the community. BMJ. Clin Res. 1998;316(7141):1348–51.
Beswick AD, Rees K, Dieppe P, Ayis S, Gooberman-Hill R, Horwood J, Ebrahim S. Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet (London, England). 2008;371(9614):725–35.
Counsell SR, Callahan CM, Clark DO, Tu W, Buttar AB, Stump TE, Ricketts GD. Geriatric care management for low-income seniors: a randomized controlled trial. JAMA. 2007;298(22):2623–33.
Counsell SR, Callahan CM, Tu W, Stump TE, Arling GW. Cost analysis of the geriatric resources for assessment and Care of Elders care management intervention. J Am Geriatr Soc. 2009;57(8):1420–6.
Stuck AE, Aronow HU, Steiner A, Alessi CA, Bula CJ, Gold MN, Yuhas KE, Nisenbaum R, Rubenstein LZ, Beck JC. A Trial of annual in-home comprehensive geriatric assessments for elderly people living in the community. N Engl J Med. 1995;333(18):1184–9.
Fairhall N, Sherrington C, Kurrle SE, Lord SR, Lockwood K, Howard K, Hayes A, Monaghan N, Langron C, Aggar C, et al. Economic evaluation of a multifactorial, interdisciplinary intervention versus usual care to reduce frailty in frail older people. J Am Med Dir Assoc. 2015;16(1):41–8.
Drummond MF, Sculpher MJ, Torrance GW, OB BJ, Stoddart GL. Methods for the economic evaluation of health care Programmes. New York: NY: Oxford university press; 2005.
Ruikes FG, Zuidema SU, Akkermans RP, Assendelft WJ, Schers HJ, Koopmans RT. Multicomponent program to reduce functional decline in frail elderly people: a cluster controlled trial. J Am Board Fam Med. 2016;29(2):209–17.
van Kempen JA, Schers HJ, Jacobs A, Zuidema SU, Ruikes F, Robben SH, Melis RJ, Olde Rikkert MG. Development of an instrument for the identification of frail older people as a target population for integrated care. Br J Gen Pract. 2013;63(608):e225–31.
Ruikes FG, Meys AR, van de Wetering G, Akkermans RP, van Gaal BG, Zuidema SU, Schers HJ, van Achterberg T, Koopmans RT. The CareWell-primary care program: design of a cluster controlled trial and process evaluation of a complex intervention targeting community-dwelling frail elderly. BMC Fam Pract. 2012;13:115.
Koopmans RT, Lavrijsen JC, Hoek JF, Went PB, Schols JM. Dutch elderly care physician: a new generation of nursing home physician specialists. J Am Geriatr Soc. 2010;58(9):1807–9.
Doran T, Roland M. Lessons from major initiatives to improve primary care in the United Kingdom. Health Aff. 2010;29(5):1023–9.
van Weel C, Schers H, Timmermans A. Health care in the Netherlands. J Am Board Fam Med. 2012;25(Suppl 1):S12–7.
Boeckxstaens P, De Graaf P. Primary care and care for older persons: position paper of the European forum for primary care. Qual Prim Care. 2011;19(6):369–89.
Weinberger M, Samsa GP, Schmader K, Greenberg SM, Carr DB, Wildman DS. Comparing proxy and patients' perceptions of patients' functional status: results from an outpatient geriatric clinic. J Am Geriatr Soc. 1992;40(6):585–8.
Krabbe PF, Stouthard ME, Essink-Bot ML, Bonsel GJ. The effect of adding a cognitive dimension to the EuroQol multiattribute health-status classification system. J Clin Epidemiol. 1999;52(4):293–301.
Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? PharmacoEconomics. 2016;34(7):645–9.
Lutomski JE, Baars MA, Schalk BW, Boter H, Buurman BM, den Elzen WP, Jansen AP, Kempen GI, Steunenberg B, Steyerberg EW, et al. The development of the older persons and informal caregivers survey minimum DataSet (TOPICS-MDS): a large-scale data sharing initiative. PLoS One. 2013;8(12):e81673.
Lamers LM, McDonnell J, Stalmeier PF, Krabbe PF, Busschbach JJ. The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ. 2006;15(10):1121–32.
Hakkaart-van Roijen L, Tan S, Bouwmans C. Handleiding voor Kostenonderzoek, Methoden en Standaard Kostprijzen voor Economische Evaluaties in De Gezondheidszorg (Dutch manual for costing: methods and standard costs for economic evaluations in healthcare). College voor Zorgverzekeringen: Diemen, The Netherlands; 2011.
Z-index. In. G-Standard. The Hague, The Netherlands: Royal Dutch Society for Pharmacy; 2006. https://www.z-index.nl/g-standaard.
Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ. 2002;11(5):415–30.
Makai P, Looman W, Adang E, Melis R, Stolk E, Fabbricotti I. Cost-effectiveness of integrated care in frail elderly using the ICECAP-O and EQ-5D: does choice of instrument matter? Eur J Health Econ. 2015;16(4):437–50.
Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ (Clinical research ed). 2009;b2393:338.
Marzetti E, Calvani R, Landi F, Hoogendijk EO, Fougere B, Vellas B, Pahor M, Bernabei R, Cesari M. Innovative Medicines Initiative: The SPRINTT Project. J Frailty Aging. 2015;4(4):207–8.
Lacas A, Rockwood K. Frailty in primary care: a review of its conceptualization and implications for practice. BMC Med. 2012;10:4.
Rockwood K, Howlett S, Stadnyk K, Carver D, Powell C, Stolee P. Responsiveness of goal attainment scaling in a randomized controlled trial of comprehensive geriatric assessment. J Clin Epidemiol. 2003;56(8):736–43.
Brazier JE, Walters SJ, Nicholl JP, Kohler B. Using the SF-36 and Euroqol on an elderly population. Qual Life Res. 1996;5(2):195–204.
Al-Janabi H, Flynn TN, Peters TJ, Bryan S, Coast J. Test-retest reliability of capability measurement in the UK general population. Health Econ. 2015;24(5):625–30.
van de Wetering G, Olde Rikkert M, van der Wilt GJ, Adang E. Understanding and anticipating lag-time bias in cost-effectiveness studies: the role of time in cost-effectiveness analysis. Int J Technol Assess Health Care. 2014;30(6):608–11.
de Stampa M, Vedel I, Bergman H, Novella JL, Lechowski L, Ankri J, Lapointe L. Opening the black box of clinical collaboration in integrated care models for frail, elderly patients. The Gerontologist. 2013;53(2):313–25.
Sandberg M, Kristensson J, Midlov P, Jakobsson U. Effects on healthcare utilization of case management for frail older people: a randomized controlled trial (RCT). Arch Gerontol Geriatr. 2015;60(1):71–81.
Metzelthin SF, van Rossum E, Hendriks MR, De Witte LP, Hobma SO, Sipers W, Kempen GI. Reducing disability in community-dwelling frail older people: cost-effectiveness study alongside a cluster randomised controlled trial. Age Ageing. 2015;44(3):390–6.
Looman WM, Huijsman R, Bouwmans-Frijters CA, Stolk EA, Fabbricotti IN. Cost-effectiveness of the 'Walcheren integrated care Model' intervention for community-dwelling frail elderly. Fam Pract. 2016; 33(2):154–60.
van Leeuwen KM, Bosmans JE, Jansen AP, Hoogendijk EO, Muntinga ME, van Hout HP, Nijpels G, van der Horst HE, van Tulder MW. Cost-effectiveness of a chronic care model for frail older adults in primary care: economic evaluation alongside a stepped-wedge cluster-randomized trial. J Am Geriatr Soc. 2015;63(12):2494–504.
Looman WM, Huijsman R, Bouwmans-Frijters CA, Stolk EA, Fabbricotti IN. Cost-effectiveness of the 'Walcheren integrated care Model' intervention for community-dwelling frail elderly. Fam Pract. 2016;33(2):154–60.
Lubeck DP, Hubert HB. Self-report was a viable method for obtaining health care utilization data in community-dwelling seniors. J Clin Epidemiol. 2005;58(3):286–90.
Seidl H, Meisinger C, Kirchberger I, Burkhardt K, Kuch B, Holle R. Validity of self-reported hospital admissions in clinical trials depends on recall period length and individual characteristics. J Eval Clin Pract. 2016;22(3):446–54.
Brusco NK, Watts JJ. Empirical evidence of recall bias for primary health care visits. BMC Health Serv Res. 2015;15:381.
Garcia PA, Dias JM, Silva SL, Dias RC. Prospective monitoring and self-report of previous falls among older women at high risk of falls and fractures: a study of comparison and agreement. Brazilian J Phys Ther. 2015;19(3):218–26.
Acknowledgements
We are most grateful to all participants and health care professionals that were involved in the study. Furthermore, we would like to thank all professionals, volunteers, and health care organizations that are involved in ‘Netwerk 100’ (https://www.netwerk100.nl/) for their contributions to the development of the CareWell-primary care program.
Funding
This study was funded by the Dutch National Care for the Elderly Program, as initiated by the Netherlands Organization for Health Research and Development (ZonMW: project no. 313050201). Health insurance companies (CZ and UVIT) and the municipality provided additional funding. Funding bodies were not involved in the design, methods, subject recruitment, data collection, analysis or preparation of the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
FR, HS, RK and SZ designed the study. FR acquired the data. FR, EA and SZ were responsible for the statistical analyses. FR, PA, HS, RK and SZ and contributed to the interpretation of data. FR wrote the first draft. PA, HS, RK and SZ critically revised this draft. FR wrote the final draft. All authors approved of the final version, and are accountable for all aspects of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was reviewed by the Ethics Committee of the Radboud University Medical Centre Nijmegen (registration number 2010/403). All participants gave written informed consent. In case of cognitive deficits, both the participant and their primary caregiver/ legal representative consented.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ruikes, F.G.H., Adang, E.M., Assendelft, W.J.J. et al. Cost-effectiveness of a multicomponent primary care program targeting frail elderly people. BMC Fam Pract 19, 62 (2018). https://doi.org/10.1186/s12875-018-0735-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-018-0735-4