Abstract
Background
Failure of conservative treatment in patients over 70 years of age with a rotator cuff tear makes surgery a possible option, considering the increase in life expectancy and the high functional demands of elderly patients. The purpose of this systematic review of the literature was to evaluate the subjective and objective outcomes after arthroscopic rotator cuff repair in patients over 70 years of age.
Methods
A systematic review was performed to identify all the studies reporting subjective and objective outcomes in patients aged 70 years or older undergoing arthroscopic rotator cuff repair. Constant Murley Score (CMS), visual analog scale (VAS), American Shoulder and Elbow Surgeons Score (ASES), and Simple Shoulder Test (SST) were used to detect any clinical improvement after surgery. Retear and satisfaction were also analyzed.
Results
Out of 941 studies identified, only 6 papers have been included in the review. All studies reported improvements in postoperative functional outcome scores that exceed the minimal clinically relevant difference. The mean retear rate amounts to 21.9%, which is in line with the failure rate of rotator cuff repair in general population. Moreover, postoperative satisfaction is very high (95%).
Conclusion
This systematic review suggests that arthroscopic rotator cuff repair in patients over 70 years of age could be a valid treatment option after failure of conservative approach.
Level of evidence: 4
Trial registration The study was registered on PROSPERO (registration ID: CRD42018088613)
Similar content being viewed by others
Introduction
Rotator cuff (RC) tears are a common cause of pain and disability of the shoulder in adult population, with an incidence that increases with age. In fact, although a genetic susceptibility seems to be present [1], the RC lesions basically result as part of a degenerative process of aging [2, 3].
Radiologic studies revealed that the prevalence of asymptomatic full-thickness RC tears is 28% in patients ≥ 60 years and 50% in patients ≥ 70 years [4, 5]. Moreover, 50% of these asymptomatic tears seem to become symptomatic at a mean of 2.8 years after diagnosis [6].
In older patients, primary conservative treatment for symptomatic RC tears is a reasonable option, as shown by the good clinical results for this population [7, 8].
Moreover, surgical treatment in elderly patients could be insidious since advanced age has been identified as a negative prognostic factor for RC healing with a retear rate of 32% in patients older than 70 years [9, 10]. Low healing response in older patients may be due to several reasons that potentially increase the difficulty of repair: larger lesions, fatty degeneration, and poor quality of tendon [2, 9, 11]. Furthermore, age-related comorbidities may frequently compromise surgical treatment. In fact, older patients are often affected by osteoporosis, which can be responsible for anchor pullout or tuberosity fracture [4], and metabolic syndrome, which is reported to reduce tendon healing [12, 13].
However, failure of conservative therapy in this population makes surgical treatment of RC tears a valid option of treatment, considering the increase in life expectancy and the high functional demands of many patients > 70 years [14]. Recently, several authors have started to study the results of RC repair in elderly patients.
The purpose of this systematic review of the literature was to evaluate the subjective and objective outcomes after arthroscopic RC repair in patients over 70 years of age.
Materials and methods
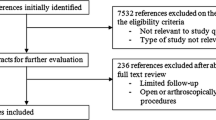
A systematic review was performed to identify all studies reporting subjective and objective outcomes in patients aged 70 years or older undergoing arthroscopic RC repair. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed to perform this systematic review of the literature and to present the results [15]. A protocol was written stating the purpose of the review, and the search strategy and was registered on PROSPERO on February 27, 2018 (registration ID: CRD42018088613). A flow diagram according to PRISMA guidelines summarizes our selection protocol (Fig. 1).
Searches
An electronic search of the literature was performed in the MEDLINE database via PubMed and Embase database from the databases’ inception up to 26 November 2020, using the following search string for title and abstract: (((Rotator Cuff OR Rotator Cuff Injuries OR Rotator Cuff Tear Arthropathy) AND (repair) AND (Arthroscopy OR arthroscopic)) NOT ((platelet-rich plasma) OR (prp)) OR ((Rotator Cuff OR Rotator Cuff Injuries OR Rotator Cuff Tear Arthropathy) AND (repair) AND (Arthroscopy OR arthroscopic)) NOT ((miniopen OR mini + open OR open))) LIMITS (aged OR aged,70 and more). MeSH terms were used for “Rotator Cuff”, “Rotator Cuff Injuries”, “Rotator Cuff Tear Arthropathy”, and “Arthroscopy”.
The search was restricted to English-language literature; meta-analyses, systematic reviews, and narrative reviews were excluded.
Study inclusion and exclusion criteria
According to the methodology recommended by Harris et al. [16], after deletion of duplicates, title and abstract of all identified studies were independently examined by two reviewers, who applied the study eligibility criteria.
In particular, the inclusion criteria were English language and level of evidence 1 to 5 that evaluated the subjective and objective outcomes after arthroscopic RC repair in patients aged 70 years or over.
Exclusion criteria were not meeting inclusion criteria, reviews, narrative reviews, systematic reviews, meta-analyses, and clinical studies that evaluate open or mini-open RC repair in patients aged 70 years or older, or arthroscopic RC repair with the use of platelet-rich plasma augmentation. In addition, epidemiological, radiological, animal, and cadaveric studies were excluded.
In case of disagreement between reviewers, consensus was sought through discussion and, in case of persistent disagreement, a third reviewer was consulted and the study was included until full-text review could be performed. Finally, eligible articles underwent full-text review for a more detailed evaluation. Both reviewers also manually cross-referenced to ensure that all potential studies were included. Reviewers were not blinded to the authors or affiliated institutions of the retrieved studies. The final list of included studies was agreed to by consensus.
Study quality assessment
Two reviewers (C.F. and C.S.) independently assessed methodological quality of the included studies according to the Methodological Index for Nonrandomized Studies (MINORS) checklist [17]. On the basis of this tool, 8 items for noncomparative studies and 12 items for comparative studies have been evaluated with a score that varies from 0 to 2 (0, not reported; 1, reported but inadequate; 2, reported and adequate). Therefore, the maximum global score was 16 for a noncomparative study and 24 for a comparative study.
The level of evidence of each article was assessed using the 2003 Journal of Bone and Joint Surgery definitions for orthopedic publications [18].
Data extraction strategy
Two reviewers independently (C.F. and C.S.) extracted study data using a standardized data extraction form that was predefined according to the protocol. Discordance was resolved by both reviewers rechecking their extracted data until data sheets corresponded. If no consensus could be reached, a third reviewer (AM) was consulted. When presented, for each study, information regarding the characteristics of the studies (author, year and journal of publication, study design and level of evidence, number of patients and shoulders), the characteristics of the participants of the studies (age, dominant shoulder or not, follow-up duration, preoperative validated outcome measures), and the clinical outcome of the treatment (postoperative outcome measures, failure rates and evidence of tendon healing, clinical results of the final follow-up) was extracted. Where possible, the compiled data from individual studies with the same outcome measures were pooled together. Demographic data were compiled to assess weighted mean ages across groups.
Results
As shown in Fig. 1, our search identified 941 studies based on the described searching strategy protocol.
After a careful screening of title and abstract, 15 articles underwent full-text review for a more detailed evaluation. The strict eligibility criteria applied in this review finally reduced the number of articles to six studies [10, 19,20,21,22,23].
The characteristics of the included studies are presented in Table 1.
The mean follow-up was 28 months with a wide range (12–50 months). As shown in “Materials and methods” section, different scores were evaluated since there is not a common tool for the clinical evaluation: Constant Murley Score (CMS), visual analog scale (VAS), American Shoulder and Elbow Surgeons Score (ASES score), and Simple Shoulder Test (SST). The CMS was assessed at the postoperative follow-up in four studies (265 shoulders): the mean value was 71.5 points (range 58.0–76.0 points). Of four studies analyzed, only three reported the preoperative CMS (236 shoulders) with a mean preoperative value of 40.3 points (range 23.0–48.8 points). The CMS improved after surgery with a mean value of improvement of 31.2 points (Fig. 2). Considering the minimal clinically important difference for CMS (10.4 points) [24], the overall analysis of the reported data showed a relevant increase in the mean CMS after surgery.
The VAS score was evaluated in three studies (Fig. 3). The overall analysis of postoperative VAS score revealed a significant difference as compared with the preoperative values: in particular, this score decreased after surgery from 6.3 cm (range 4.6–8.0 cm) to 1.7 cm (range 0.5–2.0 cm). The difference of 4.6 cm is almost three times the minimal clinically important difference for VAS (1.4 cm) [25.]
Similar improvements were registered in ASES and SST score as shown in Fig. 4.
Retears of the RC were evaluated with ultrasound in three studies (237 patients). According to these studies, 21.9% (range 17.5–32%) of the patients presented a new lesion at follow-up.
In one study [20], patients with full-thickness reruptures had a significantly lower Constant Score (77 versus 70; p = 0.015) and ASES (91 versus 82; p = 0.02). Also, Robinson et al. [10] showed a greater improvement of the postoperative Constant Score in patients with intact rotator cuff at follow-up (43 versus 14 points), but there is no information about significance level.
Satisfaction, reported in three studies [21,22,23], was, on average, very high: the mean value of satisfied patients at final follow-up was 95% (range 93–97%).
Discussion
The principal finding of the present study is that arthroscopic RC repair in elderly population over 70 years of age provides good improvement in shoulder function with a very high rate of patient satisfaction (95%). On average, more than 450 patients were evaluated in this review, and the satisfactory results of the study justify the surgical approach in elderly population.
In literature, the effect of advanced age on RC healing is still debated, and 69 years of age is identified as a conventional cutoff value for successful healing after arthroscopic repair in small- to medium-sized RC tears [26]. Indeed, the retear rate, which increases minimally until 65 years of age, starts to rise substantially over the age of 70 years, probably because older patients frequently present large and complete tears upon surgery [2]. In fact, Miyazaki et al. confirmed that extensive lesions were greater in older population (37.5% among patients up to 69 years of age and 50% among those aged over 75 years). [21].
Nevertheless, despite the assumed poorer tendon healing capacity of older patients, the studies included in this systematic review showed improvement in all clinical and functional scores.
RC healing was assessed in only four studies with MRI or ultrasound [10, 20, 21, 23]. We found a mean retear rate of 18.6%, which is similar to the data reported by Diebold in his study of 1600 arthroscopic RC repairs. They reported an overall failure tendon healing in 13% of patients, with a retear rate of 25% in those aged 70 to 79 years [27].
Good and comparable outcomes are found even when RC tears in patients over 70 years are treated with an open technique [28,29,30]: De Carvalho et al. [28] show how the average postoperative Constant Score was 80.1 and the mean SST was 9.8. Nevertheless, arthroscopic RC repair is minimally invasive, with a lower risk of deltoid damage, allows treatment of associated lesions, and, potentially, results in faster recovery [31, 32].
Several limitations affect this study: firstly, the different clinical outcome scores used in the selected articles reduced the sample for quantitative analysis. In addition, there is no information about relevant clinical factors such as grade of fatty infiltration, treatment history, surgical technique (single-row, double-row, side-to-side sutures), or accessory surgical treatment (biceps tenotomy or tenodesis, acromioplasty, or distal clavicle resection). Moreover, our review is exposed to some bias because of the low level of the methodological quality of the studies included (no RCT) and the unavailability of raw data.
In conclusion, arthroscopic rotator cuff repair in patients over 70 years of age showed good clinical results and high satisfaction rate and can thus be considered a valid option of treatment after failure of conservative approach. The result of this review should encourage future randomized controlled studies to focus on this population to support surgical treatment also in elderly patients.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CMS:
-
Constant Murley Score
- VAS:
-
Visual analog scale
- ASES:
-
American Shoulder and Elbow Surgeons Score
- SST:
-
Simple Shoulder Test
- RC:
-
Rotator cuff
References
Longo UG, Margiotti K, Petrillo S, Rizzello G, Fusilli C, Maffulli N et al (2018) Genetics of rotator cuff tears: no association of col5a1 gene in a case-control study. BMC Med Genet 19(1):217
Hattrup SJ (1995) Rotator cuff repair: relevance of patient age. J Shoulder Elb Surg. 4(2):95–100
Uhthoff HK, Sano H (1997) Pathology of failure of the rotator cuff tendon. Orthop Clin North Am 28(1):31–41
Brewer BJ (1979) Aging of the rotator cuff. Am J Sports Med 7(2):102–110
Fehringer EV, Sun J, VanOeveren LS, Keller BK, Matsen FA (2008) Full-thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elb Surg. 17(6):881–885
Yamaguchi K (2001) Mini-open rotator cuff repair: an updated perspective. Instr Course Lect 50:53–61
Merolla G, Paladini P, Saporito M, Porcellini G (2011) Conservative management of rotator cuff tears: literature review and proposal for a prognostic. Prediction Score. Muscles Ligaments Tendons J. 1(1):12–19
Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY et al (2013) Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elb Surg. 22(10):1371–1379
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG (2005) Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Jt Surg Am 87(6):1229–1240
Robinson PM, Wilson J, Dalal S, Parker R, Norburn P, Roy BR (2013) Rotator cuff repair in patients over 70 years of age: early outcomes and risk factors associated with re-tear. Bone Jt J. 95(2):199–205
Charousset C, Bellaïche L, Kalra K, Petrover D (2010) Arthroscopic repair of full-thickness rotator cuff tears: is there tendon healing in patients aged 65 years or older? Arthrosc J Arthrosc Relat Surg. 26(3):302–309
Esenkaya I, Unay K (2011) Tendon, tendon healing, hyperlipidemia and statins. Muscles Ligaments Tendons J. 1(4):169–171
Longo UG, Franceschi F, Ruzzini L, Spiezia F, Maffulli N, Denaro V (2009) Higher fasting plasma glucose levels within the normoglycaemic range and rotator cuff tears. Br J Sports Med 43(4):284–287
Geary MB, Elfar JC (2015) Rotator cuff Tears in the elderly patients. Geriatr Orthop Surg Rehabil. 6(3):220–224
Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6(7):e1000097
Harris JD, Quatman CE, Manring MM, Siston RA, Flanigan DC (2014) How to write a systematic review. Am J Sports Med 42(11):2761–2768
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (Minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Jt Surg - Ser A. 85(1):1–3
Bhatia S, Greenspoon JA, Horan MP, Warth RJ, Millett PJ (2015) Two-year outcomes after arthroscopic rotator cuff repair in recreational athletes older than 70 years. Am J Sports Med 43(7):1737–1742
Flurin PH, Hardy P, Abadie P, Boileau P, Collin P, Deranlot J et al (2013) Arthroscopic repair of the rotator cuff: prospective study of tendon healing after 70 years of age in 145 patients. Orthop Traumatol Surg Res. 99(8S):S379–S384. https://doi.org/10.1016/j.otsr.2013.10.007
Miyazaki AN, da Silva LA, Santos PD, Checchia SL, Cohen C, Giora TSB. Evaluation of the results from arthroscopic surgical treatment of rotator cuff injuries in patients aged 65 years and over. Rev Bras Ortop. 2015;50(3):305–11. http://linkinghub.elsevier.com/retrieve/pii/S2255497115000695
Verma NN, Bhatia S, Baker CL, Cole BJ, Boniquit N, Nicholson GP et al (2010) Outcomes of arthroscopic rotator cuff repair in patients aged 70 years or older. Arthrosc J Arthrosc Relat Surg. 26(10):1273–1280. https://doi.org/10.1016/j.arthro.2010.01.031
Moraiti C, Valle P, Maqdes A, Boughebri O, Dib C, Giakas G et al (2015) Comparison of functional gains after arthroscopic rotator cuff repair in patients over 70 years of age versus patients under 50 years of age: a prospective multicenter study. Arthroscopy 31(2):184–190. https://doi.org/10.1016/j.arthro.2014.08.020
Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Äärimaa V (2013) Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elb Surg. 22(12):1650–1655
Tashjian RZ, Deloach J, Porucznik CA, Powell AP (2009) Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elb Surg. 18(6):927–932
Park JS, Park HJ, Kim SH, Oh JH (2015) Prognostic factors affecting rotator cuff healing after arthroscopic repair in small to medium-sized tears. Am J Sports Med 43(10):2386–2392
Diebold G, Lam P, Walton J, Murrell GAC (2017) Relationship between age and rotator cuff retear: a study of 1,600 consecutive rotator cuff repairs. J Bone Jt Surg Am 99(14):1198–1205
De Carvalho BR, Puri A, Calder JA (2012) Open rotator cuff repairs in patients 70 years and older. ANZ J Surg 82(6):461–465
Worland RL, Arredondo J, Angles F, Lopez-Jimenez F. Repair of massive rotator cuff tears in patients older than 70 years. J Shoulder Elb Surg. 1999;8(1):26–30. http://www.sciencedirect.com/science/article/pii/S1058274699900502
Yel M, Shankwiler JA, Noonan JE, Burkhead WZ (2001) Results of decompression and rotator cuff repair in patients 65 years old and older: 6 to 14-year follow-up. Am J Orthop. 30(4):347–352
Owens BD, Williams AE, Wolf JM (2015) Risk factors for surgical complications in rotator cuff repair in a veteran population. J Shoulder Elb Surg. 24(11):1707–1712
Day M, Westermann R, Duchman K, Gao Y, Pugely A, Bollier M et al (2018) Comparison of short-term complications after rotator cuff repair: open versus arthroscopic. Arthrosc J Arthrosc Relat Surg. 34(4):1130–1136
Acknowledgements
None.
Funding
No internal or external funding sources were utilized in this investigation.
Author information
Authors and Affiliations
Contributions
C.F.: conception of the study, extraction of data, writing of the work; C.S.: extraction of data, writing of the work; A.M.: analysis of data; L.P.: paper revision; R.C.: design of the study; P.S.R.: interpretation of data; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
P.S.R. is consultant for Johnson & Johnson, Smith and Nephew, Zimmer Biomet. All other authors have no conflicts of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fossati, C., Stoppani, C., Menon, A. et al. Arthroscopic rotator cuff repair in patients over 70 years of age: a systematic review. J Orthop Traumatol 22, 3 (2021). https://doi.org/10.1186/s10195-021-00565-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-021-00565-z