Abstract
Introduction
Low central venous oxygen saturation (ScvO2) has been associated with increased risk of postoperative complications in high-risk surgery. Whether this association is centre-specific or more generalisable is not known. The aim of this study was to assess the association between peri- and postoperative ScvO2 and outcome in high-risk surgical patients in a multicentre setting.
Methods
Three large European university hospitals (two in Finland, one in Switzerland) participated. In 60 patients with intra-abdominal surgery lasting more than 90 minutes, the presence of at least two of Shoemaker's criteria, and ASA (American Society of Anesthesiologists) class greater than 2, ScvO2 was determined preoperatively and at two hour intervals during the operation until 12 hours postoperatively. Hospital length of stay (LOS) mortality, and predefined postoperative complications were recorded.
Results
The age of the patients was 72 ± 10 years (mean ± standard deviation), and simplified acute physiology score (SAPS II) was 32 ± 12. Hospital LOS was 10.5 (8 to 14) days, and 28-day hospital mortality was 10.0%. Preoperative ScvO2 decreased from 77% ± 10% to 70% ± 11% (p < 0.001) immediately after surgery and remained unchanged 12 hours later. A total of 67 postoperative complications were recorded in 32 patients. After multivariate analysis, mean ScvO2 value (odds ratio [OR] 1.23 [95% confidence interval (CI) 1.01 to 1.50], p = 0.037), hospital LOS (OR 0.75 [95% CI 0.59 to 0.94], p = 0.012), and SAPS II (OR 0.90 [95% CI 0.82 to 0.99], p = 0.029) were independently associated with postoperative complications. The optimal value of mean ScvO2 to discriminate between patients who did or did not develop complications was 73% (sensitivity 72%, specificity 61%).
Conclusion
Low ScvO2 perioperatively is related to increased risk of postoperative complications in high-risk surgery. This warrants trials with goal-directed therapy using ScvO2 as a target in high-risk surgery patients.
Similar content being viewed by others
Introduction
Several randomised controlled clinical studies have shown improved morbidity and mortality in high-risk surgical patients with perioperative optimisation of haemodynamics using strict treatment protocols in the single-centre setting [1–3]. The haemodynamic endpoints in goal-directed studies have been based on values derived from the pulmonary artery catheter [1–4], oesophageal Doppler [5–10], or (very recently) lithium indicator dilution and pulse power analysis [11]. Central venous oxygen saturation (ScvO2) and mixed venous oxygen saturation (SvO2) have been proposed to be indicators of the oxygen supply/demand relationship. However, the relationship between SvO2 and ScvO2 remains controversial [12]. Venous oxygen saturations differ among organ systems because different organs extract different amounts of oxygen. It is therefore conceivable that venous oxygen saturation depends on the site of measurement [13]. Redistribution of blood flow and alterations in regional oxygen demand (for example, in shock, severe head injury, general anaesthesia, as well as microcirculatory disorders) may affect the difference between ScvO2 and SvO2. Although ScvO2 principally reflects the relationship of oxygen supply and demand, mainly from the brain and the upper part of the body [13], it correlates reasonably well with concomitantly measured SvO2 [12, 13], which is more dependent on changes in oxygen extraction in the gastrointestinal tract.
In patients with severe sepsis and septic shock, early ScvO2-driven haemodynamic treatment was found to reduce mortality [14]. More recently, low postoperative ScvO2 values were associated with an increased risk of complications in high-risk surgical patients [11]. Despite increasing evidence of beneficial effects on outcome, goal-directed therapies are not widely used in clinical practice. The reasons are a lack of demonstrated effect in large multicentre studies, the need for postoperative intensive care resources, the necessity of instituting complex protocols, as well as the need for monitoring techniques that are not routinely used in these specific patient groups. Using the ScvO2 as a potential target variable for haemodynamic optimisation is attractive because central venous catheterisation is routinely used in high-risk patients undergoing major surgery, ScvO2 can be screened, pre-emptive treatment is possible, and no major changes are necessary for the infrastructure in the operation area.
The present investigation was a pilot study designed to assess the incidence of low perioperative ScvO2 in high-risk surgical patients and the association of low ScvO2 with outcome in a multicentre setting. The aim was to evaluate whether the association of ScvO2 and postoperative complications in a strictly protocolised, interventional single-centre study on goal-directed haemodynamic management in high-risk surgical patients [11] could be confirmed in a purely observational, multicentre setting. Specifically, this pilot study was designed to clarify (a) the recruitment rate of patients scheduled for major surgery in a multicentre setting, (b) the range of perioperative ScvO2 in such patients, (c) the number of postoperative complications, and (d) the potential association between ScvO2 and complications. With these data, it should be possible to define whether a trial with goal-directed therapy using ScvO2 as a target is reasonable to conduct.
Materials and methods
Two university hospitals in Finland and one in Switzerland participated in the study. The study was approved by the appropriate ethics committee for each institution, and written informed consent was obtained from each patient. Patients were screened for inclusion and exclusion criteria between September 20 and December 20, 2004.
Inclusion criteria
For a patient to be included in the study, both of the following criteria had to be fulfilled: (a) increased surgical risk based on intra-abdominal or retroperitoneal surgery with an expected duration of at least 90 minutes or on abdominal aortic surgery and (b) two or more of Shoemaker's criteria of high risk [2]. These criteria include patient history (more than 70 years old with limited major physiological function, previous severe cardiopulmonary or vascular illness, and severe nutritional disorders), current clinical condition (severe multiple trauma, massive acute blood loss, shock, septicaemia or septic shock, respiratory failure, acute abdominal catastrophe, and acute intestinal or renal failure), the surgical procedure (extensive surgery for cancer or prolonged surgery more than eight hours), ASA (American Society of Anesthesiologists) class of greater than two, and a perioperative need for a central venous catheter.
Exclusion criteria
Exclusion criteria for the study were a contraindication for a central venous catheter, unstable angina pectoris, primary hepatic or hepato-biliary surgery, the refusal of blood products, and the inability to give informed consent or refusal to consent.
Study protocol
Anaesthesia, operation, and postoperative treatment were performed according to the local standards. All patients were postoperatively admitted either to an intensive care unit (ICU) or another high-dependency care (HDC) area (intermediate care unit or postanaesthesia care unit). Blood samples for the measurement of ScvO2 and haemoglobin were taken after induction of anaesthesia and thereafter at two hour intervals up to 12 hours postoperatively. Blood gas analyses were performed by intermittent blood sampling and co-oximetry (ABL 725; Radiometer, Copenhagen, Denmark [centres 1 and 2]; GEM Premier 3000; Instrumentation Laboratory, Barcelona, Spain [centre 3]).
Complications
Complications and deaths occurring within 28 days of enrolment were included in the data analysis. Complications were prospectively defined and were diagnosed by clinical staff. Length of stay in the study hospital was censored at 28 days, and the patient's location at 28 days was recorded.
Statistics
Data are presented as mean ± standard deviation when normally distributed, as medians (interquartile range) when not normally distributed, or (for categorical variables) as a percentage of the group from which they were derived. Normality was tested with the Kolmogorov-Smirnov test. Categorical data were tested with Fisher's exact test. Continuous data were tested with the t test when normally distributed and with the Mann-Whitney U test when not normally distributed. Trends in physiological parameters over time were compared with repeated-measures analysis of variance.
Univariate analysis was performed to test associations with complications and death. For data recorded hourly during the study period, the baseline values, the lowest values, and the mean over the 12-hour study period were tested. A multiple logistic regression model was used to identify independent risk factors for postoperative complications. A stepwise approach was used to enter new terms into the logistic regression model, where p < 0.05 was set as the limit for inclusion of new terms. Results of logistic regression are reported as adjusted odds ratios (ORs) with 95% confidence intervals (CIs). Receiver operator characteristic (ROC) curves were constructed to identify optimal cutoff values for association with outcome. The optimum cutoff was defined as the value associated with the highest sum of sensitivity and specificity. Analysis was performed with SPSS version 12.01 (SPSS Inc., Chicago, IL, USA) and Sigma Plot version 10.01 (Systat Software, Inc., Richmond, CA, USA) software, and significance was set at p < 0.05.
Results
Of 218 screened patients, 60 patients fulfilled requirements for both inclusion and exclusion criteria and gave written informed consent (21 females, 39 males). Their mean age was 72 ± 10 years, and simplified acute physiology score (SAPS II) was 32 ± 12. In two centres, all patients were elective surgical cases, whereas in the third centre, 12 out of 21 patients were emergencies. Demographics and outcome data as well as indications for laparatomy stratified for the three centres are indicated in Table 1. Mean SAPS II scores in the three centres were 30, 26, and 40, respectively, and the associated mortality rates were 0%, 6%, and 24%, respectively.
As compared with preoperative values, ScvO2 was lower immediately after surgery. Haemoglobin decreased (preoperative 110 ± 19 g/l versus 102 ± 17 g/l immediately after surgery, p = 0.003).
Overall length of stay in the ICU/HDC was 1.0 (0 to 1) days, and hospital LOS was 10.5 (8 to 14) days (observation period 28 days). Six patients died (28-day mortality 10%); three of them were emergency cases (28-day mortality in emergency cases 25%).
Sixty-seven postoperative complications were recorded in 32 patients (20 cardiorespiratory, 23 surgical, 19 infectious, and 5 other; between 1.0 and 1.3 per patient per centre). Univariate analysis identified nine variables associated with postoperative complications (Table 2). Six of them were ScvO2 variables (Figure 1a,b). Additionally, haemoglobin (111 ± 18 versus 105 ± 23 g/l, p = 0.018), SAPS II (27 ± 11 versus 45 ± 26, p = 0.003), and hospital LOS (10 [8 to 12] versus 14 [10 to 17] days, p = 0.001) were associated with postoperative complications.
Intraoperative (a) and postoperative (b) ScvO2 variables in patients who did and did not develop postoperative complications. P values correspond to univariate analysis of variance. ICU, intensive care unit; IMC, intermediate care unit; intraop, intraoperative; preop, preoperative; postop, postoperative; ScvO2, central venous oxygen saturation.
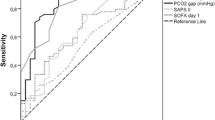
After multivariate analysis, mean ScvO2 value (OR 1.23 [95% CI 1.01 to 1.50], p = 0.037), hospital LOS (OR 0.75 [95% CI 0.59 to 0.94], p = 0.012), and SAPS II (OR 0.90 [95% CI 0.82 to 0.99], p = 0.029) were independently associated with postoperative complications. ROC curves for these variables are displayed in Figure 2. The areas under the ScvO2 and SAPS II, but not LOS, ROC curves were significantly different from 0.5 (p = 0.004 and 0.002, respectively). The optimal value of mean ScvO2 for discriminating between patients who did or did not develop complications was 73% (sensitivity 72%, specificity 61%). The relation between ScvO2 and hospital LOS in survivors and non-survivors is displayed in Figure 3.
Receiver operator characteristic (ROC) analysis for (a) mean ScvO2, (b) SAPS II score, and (c) hospital length of stay (LOS). Outcome parameter for ROC analysis is occurrence of postoperative complications. Area under the curve (AUC) was 0.74 for mean ScvO2 (p = 0.004), 0.78 for SAPS II score (p = 0.002), and 0.61 for LOS (p = 0.15). SAPS II, simplified acute physiology score; ScvO2, central venous oxygen saturation.
Central venous oxygen saturation (ScvO2) (percentage) in survivors and non-survivors and in patients with high and low mean ScvO2 values. The numbers above the error bars indicate the corresponding LOS data for the different sub-groups. *Wilcoxon signed rank test versus preoperative (p < 0.05). #Mann-Whitney test versus ScvO2 >73% (p = 0.001). ICU/IMC, intensive care unit/intermediate care unit; LOS, length of stay in hospital.
Discussion
The main finding of this study was that in the multicentre setting, low ScvO2 during the peri- and postoperative period was associated with an increased risk of postoperative complications in high-risk patients undergoing major surgery. Our results support the feasibility of testing ScvO2 as a target variable to improve outcome in high-risk surgery. The criteria to define patients at high risk were pragmatic and clinically oriented and resulted in a sufficient recruitment rate. Furthermore, despite the relative heterogeneity of the patient population, ScvO2 had a reasonable predictive value for postoperative complications.
Pearse et al. [11] found that low minimum ScvO2 values during the first eight postoperative hours were associated with increased risk of postoperative complications. Their findings come from a strictly protocolised, interventional single-centre study on goal-directed haemodynamic management in high-risk surgical patients. Our results further confirm the association between ScvO2 and postoperative complications in a purely observational, multicentre setting. Furthermore, intraoperatively, we were able to demonstrate a significant difference in ScvO2 between patients who did and did not develop complications. Taken together, the present study and that of Pearse et al. suggest that the overall peri- and postoperative course of ScvO2 should be taken into account if ScvO2-targeted interventions are considered for testing in large-scale clinical trials.
Despite the relative similarity of the participating centres and the presence of comparable infrastructures for postoperative care, the hospital LOS varied widely between the centres. The reason for this is certainly multifactorial and likely to include, among other things, care processes within the individual centres, discharge policies, and variations in local health care organisation. These variations were likely to dilute any association between ScvO2 and length of stay in the relatively small sample size. Hence, we used clinically relevant predefined complications as the main outcome measure. The hospital mortality in the present study was comparable with the recent study of Pearse et al. [11] and clearly lower than what would be expected from several previous studies on high-risk surgery. Due to the small sample size and different proportions of emergency patients, relevant between-centre comparisons cannot be made.
The prognostic significance of ScvO2 less than 65% has been demonstrated in myocardial infarction [15], trauma [16], severe sepsis [17], and cardiac failure [18]. However, the only interventional trial of ScvO2 conducted so far used a target of 70% [14]. In the study of Pearse et al. [11], a level of 65% seemed to discriminate best between patients with and without complications. This may be related to the lower tissue oxygen delivery in surgical patients as compared with patients with sepsis. Despite complex physiology, the association between ScvO2 and outcome after major surgery seems to be similar to the association between cardiac index and outcome or between oxygen delivery and outcome [19–22].
The best cutoff for ScvO2 in predicting complications in our study was 73%. This corresponds well with the mean ScvO2 of 75% found by Pearse et al. [11] in patients who did not develop complications. The observed cutoff value of ScvO2 should be interpreted with some caution due to the sample size. Nevertheless, the somewhat higher best cutoff of ScvO2 for predicting complications in our study could be related to the fact that our study was observational, whereas Pearse et al. used protocolised treatment. When using protocols, the fluctuation in ScvO2 is likely to be reduced. This may also explain why in our study the mean ScvO2, rather than the minimum ScvO2, had predictive value.
In our study, the perioperative mean of ScvO2 was 74% in patients who did not develop postoperative complications. This is comparable with previous measurements in healthy subjects [23] and in patients after surgery [11, 22] but is higher than in patients with favourable outcome after severe sepsis, trauma, cardiac failure, or myocardial infarction [15–18]. Accordingly, targets for ScvO2 in future prospective trials should probably be adapted to the specific study groups.
We believe that our results encourage trials with goal-directed therapy using ScvO2 as a target in high-risk surgery patients. Based on our data and in agreement with results from others [11], target values should be in the range of 70% to 75%, and values less than 65% should be strictly avoided. In patients with cardiac failure or trauma, lower targets (at approximately 65%) may be appropriate [15, 16].
Obviously, in a multicentre approach, the inclusion of 60 patients with an observed 28-day mortality of 10% is enough to be able to demonstrate a benefit in terms of complication rate but not in terms of length of stay and mortality. To demonstrate a relative reduction in 28-day mortality of 34% (as in the study of Rivers et al. [14], with a beta error of 80% and an alpha error of 5%, the sample size in a patient group similar to that in this study would be 85 for both groups. Although the risk factors for postoperative complications agree well with previous studies, the small sample size for the multivariate analysis should be considered in interpreting our results.
Because oxygen demands are normally well controlled during general anaesthesia, efforts to increase ScvO2 should target oxygen delivery (arterial oxygen saturation, haemoglobin, and cardiac output). In fact, in this trial, preoperative haemoglobin concentrations were significantly lower in patients with complications as compared with patients without. To avoid sudden drops in ScvO2 as a consequence of the combination of hypovolaemia and anaemia during surgical bleeding, it may be prudent to correct low (<10 g/dl) preoperative haemoglobin concentrations.
A drop in ScvO2 was noted between the end of surgery and the first readings in the ICU. This finding is consistent with previous findings on ScvO2 [11] and SvO2 [19, 21] in surgical patients. Both decreased systemic oxygen delivery and increased oxygen consumption may have contributed. Pearse et al. [11] reported unchanged cardiac output in the postoperative period. If this was the same in our patients, oxygen delivery still could have decreased due to the significantly lower postoperative haemoglobin concentrations. Postoperative oxygen consumption is determined by various factors, including pain, emergence from anaesthesia, body temperature, and shivering. To avoid low postoperative ScvO2, all of these factors may have to be controlled.
Conclusion
In our study, low ScvO2 was frequently observed in patients during and after major surgery and was related to postoperative complications. In prospective trials using ScvO2 as a goal, the specific patient group has to be taken into account when target levels are defined.
Key messages
-
Low ScvO2 perioperatively is related to increased risk of postoperative complications in high-risk surgery.
-
Trials with goal-directed therapy using ScvO2 as a target in high-risk surgery patients are warranted.
Appendix
The Collaborative Study Group on Perioperative ScvO2 Monitoring is composed of authors from three centres:
Bern:
Hendrik Bracht1, Verena Eigenmann2, Matthias Haenggi1, Daniel Inderbitzin3, Stephan M Jakob1 (co-principal investigator), Stefanie Loher1, Christine Raeber1, Jukka Takala1 (coordinating investigator), Andreas Vogt7
Kuopio:
Kimmo Mäkinen5, Pekka Miettinen5, Minna Niskanen6, Ilkka Parviainen6 (co-principal investigator)
Tampere:
Heli Leppikangas4, Silvia Nunes4, Esko Ruokonen4 (co-principal investigator)
1Department of Intensive Care Medicine, University Hospital Bern, CH-3010 Bern, Switzerland
2Department of Cardiovascular Surgery, University Hospital Bern, CH-3010 Bern, Switzerland
3Department of Visceral and Transplantation Surgery, University Hospital Bern, CH-3010 Bern, Switzerland
4Department of Intensive Care, Tampere University Hospital, P.O. Box 2000, 33521 Tampere, Finland
5Department of Surgery, Kuopio University Hospital, P.O. Box 1777, 70211 Kuopio, Finland
6Department of Anesthesia and Intensive Care Medicine, Kuopio University Hospital, P.O. Box 1777, 70211 Kuopio, Finland
7Department of Anesthesiology, University Hospital Bern, CH-3010 Bern, Switzerland
Abbreviations
- HDC:
-
high-dependency care
- ICU:
-
intensive care unit
- LOS:
-
length of stay
- OR:
-
odds ratio
- ROC:
-
receiver operator characteristic
- SAPS II:
-
simplified acute physiology score
- ScvO2:
-
central venous oxygen saturation
- SvO2:
-
mixed venous oxygen saturation.
References
Boyd O, Grounds RM, Bennett ED: A randomized clinical trial of the effect of deliberate perioperative increase of oxygen delivery on mortality in high-risk surgical patients. JAMA 1993, 270: 2699-2707. 10.1001/jama.270.22.2699
Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS: Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest 1988, 94: 1176-1186.
Wilson J, Woods I, Fawcett J, Whall R, Dibb W, Morris C, McManus E: Reducing the risk of major elective surgery: randomised controlled trial of preoperative optimisation of oxygen delivery. BMJ 1999, 318: 1099-1103.
Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J: A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg 2000, 90: 1052-1059.
McKendry M, McGloin H, Saberi D, Caudwell L, Brady AR, Singer M: Randomised controlled trial assessing the impact of a nurse delivered, flow monitored protocol for optimisation of circulatory status after cardiac surgery. BMJ 2004, 329: 258. 10.1136/bmj.38156.767118.7C
Gan TJ, Soppitt A, Maroof M, el-Moalem H, Robertson KM, Moretti E, Dwane P, Glass PS: Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology 2002, 97: 820-826. 10.1097/00000542-200210000-00012
Mythen MG, Webb AR: Perioperative plasma volume expansion reduces the incidence of gut mucosal hypoperfusion during cardiac surgery. Arch Surg 1995, 130: 423-429.
Sinclair S, James S, Singer M: Intraoperative intravascular volume optimisation and length of hospital stay after repair of proximal femoral fracture: randomised controlled trial. BMJ 1997, 315: 909-912.
Venn R, Steele A, Richardson P, Poloniecki J, Grounds M, Newman P: Randomized controlled trial to investigate influence of the fluid challenge on duration of hospital stay and perioperative morbidity in patients with hip fractures. Br J Anaesth 2002, 88: 65-71. 10.1093/bja/88.1.65
Wakeling HG, McFall MR, Jenkins CS, Woods WG, Miles WF, Barclay GR, Fleming SC: Intraoperative oesophageal Doppler guided fluid management shortens postoperative hospital stay after major bowel surgery. Br J Anaesth 2005, 95: 634-642. 10.1093/bja/aei223
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED: Changes in central venous saturation after major surgery, and association with outcome. Crit Care 2005,9(6):R694-699. 10.1186/cc3888
Reinhart K, Kuhn HJ, Hartog C, Bredle DL: Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med 2004, 30: 1572-1578. 10.1007/s00134-004-2337-y
Bloos F, Reinhart K: Venous oximetry. Intensive Care Med 2005, 31: 911-913. 10.1007/s00134-005-2670-9
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001, 345: 1368-1377. 10.1056/NEJMoa010307
Hutter AM Jr, Moss AJ: Central venous oxygen saturations. Value of serial determinations in patients with acute myocardial infarction. JAMA 1970, 212: 299-303. 10.1001/jama.212.2.299
Scalea TM, Hartnett RW, Duncan AO, Atweh NA, Phillips TF, Sclafani SJ, Fuortes M, Shaftan GW: Central venous oxygen saturation: a useful clinical tool in trauma patients. J Trauma 1990, 30: 1539-1543.
Rady MY, Rivers EP, Martin GB, Smithline H, Appleton T, Nowak RM: Continuous central venous oximetry and shock index in the emergency department: use in the evaluation of clinical shock. Am J Emerg Med 1992, 10: 538-541. 10.1016/0735-6757(92)90178-Z
Ander DS, Jaggi M, Rivers E, Rady MY, Levine TB, Levine AB, Masura J, Gryzbowski M: Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol 1998, 82: 888-891. 10.1016/S0002-9149(98)00497-4
Bland RD, Shoemaker WC, Abraham E, Cobo JC: Hemodynamic and oxygen transport patterns in surviving and nonsurviving postoperative patients. Crit Care Med 1985, 13: 85-90.
Kusano C, Baba M, Takao S, Sane S, Shimada M, Shirao K, Natsugoe S, Fukumoto T, Aikou T: Oxygen delivery as a factor in the development of fatal postoperative complications after oesophagectomy. Br J Surg 1997, 84: 252-257. 10.1002/bjs.1800840232
Polonen P, Hippelainen M, Takala R, Ruokonen E, Takala J: Relationship between intra- and postoperative oxygen transport and prolonged intensive care after cardiac surgery: a prospective study. Acta Anaesthesiol Scand 1997,41(7):810-817.
Peerless JR, Alexander JJ, Pinchak AC, Piotrowski JJ, Malangoni MA: Oxygen delivery is an important predictor of outcome in patients with ruptured abdominal aortic aneurysms. Ann Surg 1998, 227: 726-732. 10.1097/00000658-199805000-00013
Madsen P, Iversen H, Secher NH: Central venous oxygen saturation during hypovolaemic shock in humans. Scand J Clin Lab Invest 1993, 53: 67-72.
Acknowledgements
This study was supported by a grant from Edwards Lifesciences.
Author information
Consortia
Additional information
Competing interests
The authors declare that they have no competing interests. No author received individual funding in connection with this study.
Authors' contributions
HB performed programming of databases for all centres, data acquisition, data analysis, calculation of statistics and manuscript revision. VE, DI, SL, IP, CR, and AV provided data acquisition and manuscript revision. MH carried out data acquisition and interpretation and manuscript revision. SMJ participated in the study design and coordination, performed the measurements, and wrote a first draft of the manuscript. HL and SN recruited patients, performed data acquisition, data analysis and interpretation, and manuscript revision. KM and PM carried out patient recruitment, data acquisition, and manuscript revision. MN and ER performed data interpretation and manuscript revision. JT provided study conception and design, data interpretation, and manuscript revision. All authors were given the opportunity to read and approve the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Collaborative Study Group on Perioperative ScvO2 Monitoring. Multicentre study on peri- and postoperative central venous oxygen saturation in high-risk surgical patients. Crit Care 10, R158 (2006). https://doi.org/10.1186/cc5094
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc5094