Abstract
Bone erosion is a hallmark of rheumatoid arthritis. Recent evidence from experimental arthritis suggests that osteoclasts are essential for the formation of local bone erosions. Two essential regulators of osteoclastogenesis have recently been described: the receptor-activator of nuclear factor kappa B ligand, which promotes osteoclast maturation, and osteoprotegerin (OPG), which blocks osteoclastogenesis. The present review summarizes the current knowledge on the role of osteoclasts in local bone erosion. In addition, the role of OPG as a therapeutic tool to inhibit local bone erosion is addressed. Finally, evidence for OPG as an inhibitor of systemic inflammatory bone loss is discussed.
Similar content being viewed by others
Local bone erosions in rheumatoid arthritis
Rheumatoid arthritis (RA) is a highly osteodestructive process, which leads to local, juxta-articular and systemic bone loss. Local bone erosion is part of the classification criteria of RA, has become a key monitoring parameter of RA and is associated with unfavorable prognosis, such as functional loss [1–3].
The first scientific description of local bone erosion came from the Austrian pathologist Anton Weichselbaum [4], who termed such lesions as "caries of the joint ends" (Fig. 1). Indeed, bone is eroded eccentrically starting from the junction zone, where the bone, the cartilage and the synovial membrane are closely attached to each other (Fig. 2). Bone is invaded by an inflammatory synovial tissue, known as 'pannus', which contains fibroblasts, mononuclear infiltrates, mast cells and numerous blood vessels.
First scientific description of local bone erosion in arthritis. (a) Photograph of Anton Weichselbaum, Chairman of Pathology at the University of Vienna from 1893 to 1916. (b) Title page of the manuscript published by Anton Weichselbaum in the Archives for Pathology, Anatomy, Physiology and Clinical Medicine in 1878. (c) Title of the manuscript, meaning "The finer changes of joint cartilage in fungous synovitis and caries of the joint-ends". Fungous synovitis was an old term for rheumatoid arthritis, which referred to excessive synovial hyperplasia. Caries of the joint ends was the first scientific description of local bone erosion in rheumatoid arthritis.
Local bone erosion starts from the junction of the cartilage, the bone and the synovial membrane. Histological sections of knee joints of hTNFtg mice stained by (a, b) hematoxylin and eosin, (c, d) tartrate-resistant acid phosphatase and (e, f) toluidine blue. Microphotographs show an overview of the knee joint ((a), (c), (e), original magnification, 25 ×) and close-ups of the junction zone ((b), (d), (f), original magnification, 100 ×). Note synovial inflammatory tissue at the junction zone (arrow in (b)), invading the subchondral bone by osteoclast-mediated bone resorption (arrow in (d)), and leading to proteoglycan loss of the articular cartilage (arrow in (f)).
From these histopathological observations it was evident that synovial inflammatory tissue has unique invasive properties, which even enable the invasion of bone and, finally, the destruction of bone. The molecular basis of this invasive nature has not been completely clarified and appears to be of a complex nature. Decreased apoptosis, activation of mitogenic signaling pathways and expression of enzymes that degrade the extracellular matrix, such as matrix metalloproteinases, play a part in this process [5–7]. Elegant studies have also linked such characteristics with synovial fibroblast-like cells of RA patients, which have intrinsic invasive properties and thus facilitate the spreading of inflammatory synovial tissue [8].
Evidence for a pivotal role of osteoclasts in local bone erosions
Bone erosion requires osteoclasts and, since the work of Bromley and Woolley, it has been known that inflammatory synovial tissue harbors osteoclasts [9]. A detailed characterization of osteoclast precursors and mature osteoclasts within local bone erosions was then accomplished by Gravallese and colleagues in the late 1990s, demonstrating that cells in synovial pannus show all the different maturation steps of the osteoclast lineage [10]. Furthermore, typical histological features of resorption lacunae were detected at the site of the erosion fronts. Lacunae are filled with multinucleated giant cells featuring typical morphological and molecular characteristics of mature osteoclasts.
These results have consequently lead to increasing interest in the role of osteoclasts in local bone erosion that is driven by the hypothesis that synovial pannus makes use of osteoclasts to accomplish bone damage. This assumption has now been supported by two studies that investigated the course of arthritis in genetically engineered mice, which lack osteoclasts (Table 1). Thus, while in wild-type mice the transfer of serum from arthritic K/BxN mice leads to immune complex-mediated, destructive synovitis, such serum transfer into receptor-activator of nuclear factor kappa B ligand (RANKL)-deficient mice leads to normal development of clinical arthritis, but the disease is not erosive [11]. RANKL-deficient mice have defective osteoclastogenesis due to defective presentation of RANKL, an essential signal for osteoclastogenesis, to osteoclast precursors [12].
Further direct evidence for a pivotal role of osteoclasts in local bone erosion comes from c-fos knockout mice, which exhibit a maturation arrest of the osteoclast lineage without affecting differentiation of other hematopoetic cells or changing the properties of the stroma [13]. These mice show complete uncoupling of synovial inflammation and bone erosion when arthritis is induced by overexpression of tumor necrosis factor (TNF) [14]. The osteoclast thus emerges as an essential prerequisite to form erosive arthritis, and therefore appears an attractive therapeutic target for RA.
Concepts to inhibit osteoclasts in arthritis
Inhibition of osteoclasts can be achieved by several different therapeutic strategies (Fig. 3). One of the best known and currently applied strategies are bisphosphonates, which inhibit osteoclasts through a complex mechanism including the inhibition of osteoclast attachment to the bone surface and the promotion of osteoclast apoptosis through inhibition of the mevalonate pathway. Based on the assumption that osteoclasts are essential for the formation of local bone erosion, bisphosphonates should inhibit this process. Indeed, pamidronate blocks local bone erosion in TNF-driven arthritis to a certain degree [15]. Only a few clinical studies have yet addressed the efficacy of bisphosphonates to inhibit local bone erosions in RA, and the results are conflicting [16–19]. However, only bisphosphonates of low potency such as etidronate were studied, which may fail to accomplish full inhibition of osteoclasts in the lesions. New, more potent bisphosphonates may thus shed new light on the efficacy of bisphosphonates on local bone erosion.
View into an erosion: mechanisms involved in osteoclastogenesis and arthritic bone erosion. The resorption front of local bone erosion in rheumatoid arthritis (RA) is illustrated. A resorption lacuna is filled with an osteoclast and surrounded by synovial inflammatory tissue (pannus) with fibroblast-like synoviocytes and T cells. Both of these cell types influence osteoclast maturation and activation, whereas cells of the macrophage lineage, which are not separately depicted, constitute the pool of osteoclast precursor cells. Potential therapeutic targets, which also represent essential mechanisms of osteoclast development and function, are indicated by black squares. Target molecules are grouped according to their functional role in the osteoclast (from the top): molecules, which influence the stromal cells to express pro-osteoclastogenic molecules (such as tumor necrosis factor [TNF], IL-1, IL-6, IL-11, IL-17 or prostaglandin E2 [PGE2]); receptor-ligand interactions, which are essential for osteoclast development and function (receptor-activator of nuclear factor kappa B ligand [RANKL]/receptor-activator of nuclear factor kappa B [RANK], macrophage-colony-stimulating factor (M-CSF)/c-fms, RGD-containing matrix molecules/avβ3 integrin); signaling intermediates downstream of the receptor level (src, TRAF-6, PI3-K); phosphokinases in the cytoplasm (akt, JNK, p38, ERK); transcription factors (c-fos, c-jun, nuclear factor [NF]-κB); and effector molecules essential for osteoclast function (cathepsin K, matrix metalloproteinase [MMP]-9, vATPase). The bar between the osteoclast and the bone indicates one of the complex methods of the function of bisphosphonates (inhibition of attachment of osteoclasts on bone), whereas other methods such as inhibition of the mevalonate pathway are not depicted.
Blockade of TNF-α and IL-1 are other currently used strategies. Both cytokines are potent osteoclastogenic factors, produced in inflammatory arthritis. Interestingly, clinical trials have shown that the effects of TNF-blockers on bone damage may exceed those effects on inflammation, suggesting that their ability to hamper osteoclast formation might be of important benefit [20, 21]. This is especially supported by the results from the Anti-Tumor Necrosis Factor Trial in Rheumatoid Arthritis with Concomitant Therapy, which showed that the effect of TNF-blockers on bone damage is independent of a clinical response to treatment [20]. Other current experimental approaches such as the application of RGD peptides, of proton pump inhibitors, of matrix metalloproteinase inhibitors and also of blockers of mitogen-activated protein kinases/stress-activated protein kinases may add a future therapeutic repertoire to block osteoclasts.
Osteoprotegerin as inhibitor of osteoclastogenesis
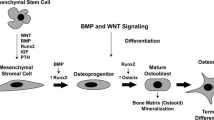
Osteoprotegerin (OPG) has emerged as one of the most attractive tools to inhibit osteoclast formation during the past years. The interaction of RANKL with its receptor-activator of nuclear factor kappa B (RANK) is an essential signal for osteoclastogenesis [22–24]. Mice deficient for RANKL or RANK are osteopetrotic due to complete lack of osteoclasts [24, 25]. Thus, the interaction of RANKL, which is expressed by stromal cells and activated T cells, with RANK, found on osteoclast precursor cells and mature osteoclasts, is essential for osteoclastogenesis and osteoclast activation.
OPG functions as a naturally occurring decoy receptor of RANK and inhibits the RANKL/RANK interaction [26, 27]. Evidence that OPG has profound effects on bone comes from OPG knockout mice, which are osteoporotic due to deregulated RANKL/RANK interaction and increased osteoclast formation [27], and also comes from the administration of OPG to laboratory animals and humans, which leads to an increase of bone mass [28, 29]. The rationale for using OPG to inhibit the formation of local bone erosions in patients with RA comes from several observations: the presence of osteoclasts in local bone erosions as described earlier [9, 10], the increased expression of RANKL and RANK within synovial inflammatory tissue [30–32], and the fact that many proinflammatory mediators present in the synovial membrane, such as TNF, IL-1, IL-17 and prostaglandin E2, induce RANKL expression [33–35].
The effects of OPG on local bone erosion
The efficacy of OPG to block local bone erosions has now been documented in different experimental models of arthritis, supporting the idea that RANKL-induced osteoclastogenesis and osteoclast activation is a key determinant in the formation of local bone erosion [15, 36, 37] (Table 2).
OPG was first studied in adjuvant arthritis, based on the hypothesis that RANKL expression by activated T cells is involved in bone resorption in this T-cell-driven arthritis model [36]. Indeed, OPG blocked bone erosion but did not affect synovial inflammation. Interestingly, OPG also affects bone erosion in a TNF-driven arthritis model, which is T-cell independent [15]. In this model, OPG reduced or even blocked bone erosion but had no major effect on synovial inflammation, suggesting that blockade of osteoclast generation and function is the mechanism involved (Fig. 4). This is supported by the reduction of synovial osteoclasts by OPG. These data were finally confirmed by observations in the collagen-induced arthritis model, showing protection of bone upon OPG treatment while synovial inflammation was not affected [37].
Effects of osteoprotegerin (OPG) on histopathological manifestations of arthritis. Human tumor necrosis factor (TNF)-transgenic mice remained untreated or were treated with OPG or anti-TNF. Treatment started at a stage of early arthritis, and effects on synovial inflammation, on bone erosion and on cartilage damage are shown. OPG significantly affects TNF-mediated bone erosion, but not inflammation or cartilage damage. * Significant (P < 0.05) reduction in severity.
These data suggest that, regardless of the nature of the precipitating mechanism, OPG appears a powerful tool to inhibit bone damage following synovial inflammation. Moreover, the RANKL/RANK interaction appears an important step in the formation of synovial osteoclasts, which is further supported by similar effects of other strategies to suppress RANKL expression, such as adeno-viral-based overexpression of IL-4, which is a potent antagonist of RANKL [38].
Systemic inflammatory bone loss and OPG
Apart from local bone erosion, systemic bone loss is a serious health burden in patients with RA. Osteoporosis develops in the majority of RA patients and is associated with increased fracture risk [39, 40]. Several factors precipitate systemic bone loss in RA patients, including female gender, high age, systemic use of glucocorticoids and decreased mobility of RA patients due to functional impairment. Interestingly, however, disease activity is also a major predictor for osteoporosis in RA patients, and is independent of other precipitating factors [41]. This suggests that the inflammatory process not only affects local bone, but also leads to bone loss at distant sites, possibly due to a disturbed cytokine balance with a negative net effect on bone.
The fact that osteoporosis in RA patients is due to increased bone resorption fuels the concept that cytokines, which stimulate osteoclastogenesis, are overexpressed and lead to systemic osteoporosis in RA patients [42]. This hypothesis is strongly supported by the fact that TNF-transgenic mice not only develop erosive arthritis, but are also severely osteoporotic [43]. Since TNF is a potent cofactor in RANKL-mediated osteoclastogenesis, OPG appears a feasible tool to treat inflammatory bone loss. Indeed, treatment of OPG reverses osteoporosis in TNF-transgenic mice and restores normal bone mass, suggesting that osteoporosis due to chronic inflammation is a consequence of osteoclast hyperactivity and increased bone resorption, and that TNF promotes generalized bone loss through RANKL [43] (Fig. 5).
Osteoprotegerin (OPG) reverses tumor necrosis factor (TNF)-mediated osteoporosis. Tibial heads of (a) wild-type mice, (b) hTNFtg mice and (c) hTNFtg mice treated with OPG are shown. Bone is stained by von Kossa (black). hTNFtg mice show rarefication of trabecular bone, indicating osteoporosis. OPG reverses TNF-mediated osteoporosis, as indicated by an increase of bone mass in the metaphyseal region of tibial bones. Arrowheads, trabecular bone.
Open questions on OPG in arthritis
Currently, no data on the effects of OPG in human RA are available. Given the results from animal models of RA, the major role of OPG in human RA might be protection from local bone erosion and systemic bone loss. Whether bone can be protected more efficiently by OPG than by other strategies, such as anti-TNF, anti-IL-1 or potent bisphosphonates, remains to be determined.
In the TNF-transgenic model, OPG was equally potent to TNF-blockade in blocking local bone erosions, and was superior to the IL-1 receptor antagonist (unpublished observations). Recent data suggest that OPG treatment might exert some inhibitory effect on synovial inflammation, especially if combined with a TNF-blocker (unpublished observations). This may be explained by blockade of RANKL/RANK interactions other than those involved in osteoclastogenesis, such as the interaction of T cells with dendritic cells [44]. Furthermore, binding of OPG to surface molecules distinct from RANKL, which has been demonstrated for tumor-necrosis-factor-related apoptosis inducing ligand, for example [45], could affect synovial inflammation. Also, the influence of OPG on loss of articular cartilage is controversial. Whereas protection of articular cartilage by OPG has been described in the adjuvant arthritis model [36], it is weak in the collagen-induced arthritis model [37] and is completely absent in the TNF-transgenic model [15]. Expression of RANKL and RANK by chondrocytes has been described, but the function of these molecules in the cartilage is unknown [46]. Thus, it is as yet unclear whether OPG affects cartilage destruction and synovial inflammation to a relevant degree, whereas the effect on bone is unequivocally proven.
Conclusion
There is a bulk of evidence that osteoclasts have a central role in local and systemic bone loss of inflammatory arthritis. Furthermore, pharmacological doses of OPG inhibit the formation of local bone erosions and restore normal bone mass in experimental models of arthritis. OPG thus appears a promising agent to block bone loss in RA. Since there is only a weak effect, if any, of OPG on inflammation, it is probable that its potential use in RA patients needs to be flanked by sufficient anti-inflammatory treatment. Patients with a high risk of bone loss might profit substantially from OPG, and it will be a challenge to select such patients by current clinical, laboratory and radiological assessments.
Abbreviations
- IL:
-
interleukin
- OPG:
-
osteoprotegerin
- RA:
-
rheumatoid arthritis
- RANK:
-
receptor-activator of nuclear factor kappa B
- RANKL:
-
receptor-activator of nuclear factor kappa B ligand
- TNF:
-
tumor necrosis factor.
References
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, Medsger T, Mitchell DM, Neustadt DH, Pinals RS, Schaller JG, Sharp JT, Wilden RL, Hunder GG: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324.
Scott DL, Pugner K, Kaarela K, Doyle DV, Woolf A, Holmes J, Hieke K: The links between joint damage and disability in rheumatoid arthritis. Rheumatology. 2000, 39: 122-132. 10.1093/rheumatology/39.2.122.
van der Heijde D, Dankert T, Nieman F, Rau R, Boers M: Reliability and sensitivity to change of a simplification of the Sharp/ van der Heijde radiological assessment in rheumatoid arthritis. Rheumatology (Oxford). 1999, 38: 941-947. 10.1093/rheumatology/38.10.941.
Weichselbaum A: Die feineren Veränderungen des Gelenkknorpels bei fungöser Synovitis und Karies der Gelenkenden. Archiv Pathol Anat Physiol Klin Med. 1878, 73: 461-475.
Sugiyama M, Tsukazaki T, Yonekura A, Matsuzaki S, Yamashita S, Iwasaki K: Localization of apoptosis and expression of apoptosis related proteins in the synovium of patients with rheumatoid arthritis. Ann Rheum Dis. 1996, 55: 442-449.
Schett G, Tohidast-Akrad M, Smolen JS, Schmid BJ, Steiner CW, Bitzan P, Zenz P, Redlich K, Xu Q, Steiner G: Activation, differential localization, and regulation of the stress-activated protein kinases, extracellular signal-regulated kinase, c-JUN N-terminal kinase, and p38 mitogen-activated protein kinase, in synovial tissue and cells in rheumatoid arthritis. Arthritis Rheum. 2000, 43: 2501-2512. 10.1002/1529-0131(200011)43:11<2501::AID-ANR18>3.0.CO;2-K.
Pap T, Gay S, Schett G: Matrix metalloproteinases. In Targeted Therapies in Rheumatology. Edited by: Smolen JS, Lipsky P. 2003, London, New York: Martin Dunitz, 483-501.
Pap T, Aupperle KR, Gay S, Firestein GS, Gay RE: Invasiveness of synovial fibroblasts is regulated by p53 in the SCID mouse in vivo model of cartilage invasion. Arthritis Rheum. 2001, 44: 676-681. 10.1002/1529-0131(200103)44:3<676::AID-ANR117>3.3.CO;2-Y.
Bromley M, Woolley DE: Chondroclasts and osteoclasts at subchondral sites of erosion in the rheumatoid joint. Arthritis Rheum. 1984, 27: 968-975.
Gravallese EM, Harada Y, Wang JT, Gorn AH, Thornhill TS, Goldring SR: Identification of cell types responsible for bone resorption in rheumatoid arthritis and juvenile rheumatoid arthritis. Am J Pathol. 1998, 152: 943-951.
Pettit AR, Ji H, von Stechow D, Müller R, Goldring SR, Choi Y, Benoist C, Gravallese EM: TRANCE/RANKL knockout mice are protected from bone erosion in a serum transfer model of arthritis. Am J Pathol. 2001, 159: 1689-1699.
Kim N, Odgren PR, Kim DK, Marks SC, Choi Y: Diverse roles of the tumor necrosis factor family member TRANCE in skeletal physiology revealed by TRANCE deficiency and partial rescue by a lymphocyte-expressed TRANCE transgene. Proc Natl Acad Sci USA. 2000, 97: 10905-10910. 10.1073/pnas.200294797.
Grigoriadis AE, Wang ZQ, Cecchini MG, Hofstetter W, Felix R, Fleisch HA, Wagner EF: c-Fos: a key regulator of osteoclastmacrophage lineage determination and bone remodeling. Science. 1994, 266: 443-448.
Redlich K, Hayer S, Ricci R, David D, Tohidast-Akrad M, Kollias G, Günter Steiner S, Smolen JS, Wagner EF, Schett G: Osteoclasts are essential for TNF-α-mediated joint destruction. J Clin Invest. 2002, 110: 1419-1427. 10.1172/JCI200215582.
Redlich K, Hayer S, Maier A, Dunstan CR, Tohidast-Akrad M, Lang S, Türk B, Pietschmann P, Woloszczuk W, Kollias G, Steiner G, Smolen J, Schett G: Tumor necrosis factor α-mediated joint destruction is inhibited by targeting osteoclasts with osteoprotegerin. Arthritis Rheum. 2002, 46: 785-792. 10.1002/art.10097.
Valleala H, Laasonen L, Koivula MK, Mandelin J, Friman C, Risteli J, Konttinen YT: Two year randomized controlled trial of etidronate in rheumatoid arthritis: changes in serum aminoterminal telopeptides correlate with radiographic progression of disease. J Rheumatol. 2003, 30: 468-473.
Hasegawa J, Nagashima M, Yamamoto M, Nishijima T, Katsumata S, Yoshino S: Bone resorption and inflammatory inhibition efficacy of intermittent cyclical etidronate therapy in rheumatoid arthritis. J Rheumatol. 2003, 30: 474-479.
Eggelmeijer F, Papapoulos SE, van Paassen HC, Dijkmans BA, Valkema R, Westedt ML, Landman JO, Pauwels EK, Breedveld FC: Increased bone mass with pamidronate treatment in rheumatoid arthritis. Results of a three-year randomized, double-blind trial. Arthritis Rheum. 1996, 39: 396-402.
Yilmaz I, Ozoran K, Gunduz OH, Ucan H, Yucel M: Alendronate in rheumatoid arthritis patients treated with methothrexate and glucocorticoids. Rheumatol Int. 2001, 20: 65-69. 10.1007/s002960000080.
Lipsky PE, van der Heijde DM, St Clair EW, Furst DE, Breedveld FC, Kalden JR, Smolen JS, Weisman M, Emery P, Feldmann M, Harriman GR, Maini RN: Infliximab and methotrexate in the treatment of rheumatoid arthritis. Anti-Tumor Necrosis Factor Trial in Rheumatoid Arthritis with Concomitant Therapy Study Group. N Engl J Med. 2000, 343: 1594-1602. 10.1056/NEJM200011303432202.
Jiang Y, Genant HK, Watt I, Cobby M, Bresnihan B, Aitchison R, McCabe D: A multicenter, double-blind, dose-ranging, randomized, placebo-controlled study of recombinant human interleukin-1 receptor antagonist in patients with rheumatoid arthritis: radiologic progression and correlation of Genant and Larsen scores. Arthritis Rheum. 2000, 43: 1001-1009. 10.1002/1529-0131(200005)43:5<1001::AID-ANR7>3.0.CO;2-P.
Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, Elliott R, Colombero A, Elliott G, Scully S, Hsu H, Sullivan J, Hawkins N, Davy E, Capparelli C, Eli A, Qian YX, Kaufman S, Sarosi I, Shalhoub V, Senaldi G, Guo J, Delaney J, Boyle WJ: Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998, 93: 165-176. 10.1016/S0092-8674(00)81569-X.
Yasuda H, Shima N, Nakagawa N, Yamaguchi K, Kinosaki M, Mochizuki S, Tomoyasu A, Yano K, Goto M, Murakami A, Tsuda E, Morinaga T, Higashio K, Udagawa N, Takahashi N, Suda T: Osteoclast differentiation factor is a ligand for osteoprotegerin/ osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci USA. 1998, 95: 3597-3602. 10.1073/pnas.95.7.3597.
Kong YY, Yoshida H, Sarosi I, Tan HL, Timms E, Capparelli C, Morony S, Oliveira-dos-Santos AJ, Van G, Itie A, Khoo W, Wakeham A, Dunstan CR, Lacey DL, Mak TW, Boyle WJ, Penninger JM: OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature. 1999, 397: 315-323. 10.1038/16852.
Dougall WC, Glaccum M, Charrier K, Rohrbach K, Brasel K, De Smedt T, Daro E, Smith J, Tometsko ME, Maliszewski CR, Armstrong A, Shen V, Bain S, Cosman D, Anderson D, Morrissey PJ, Peschon JJ, Schuh J: RANK is essential for osteoclast and lymph node development. Genes Dev. 1999, 13: 2412-2424. 10.1101/gad.13.18.2412.
Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Luthy R, Nguyen HQ, Wooden S, Bennett L, Boone T, Shimamoto G, DeRose M, Elliott R, Colombero A, Tan HL, Trail G, Sullivan J, Davy E, Bucay N, Renshaw-Gegg L, Hughes TM, Hill D, Pattison W, Campbell P, Sander S, Van G, Tarpley J, Derby P, Lee R, Boyle WJ: Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell. 1997, 89: 309-319. 10.1016/S0092-8674(00)80209-3.
Bucay N, Sarosi I, Dunstan CR, Morony S, Tarpley J, Capparelli C, Scully S, Tan HL, Xu W, Lacey DL, Boyle WJ, Simonet WS: Osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev. 1998, 12: 1260-1268.
Kostenuik PJ, Capparelli C, Morony S, Adamu S, Shimamoto G, Shen V, Lacey DL, Dunstan CR: OPG and PTH-(1-34) have additive effects on bone density and mechanical strength in osteopenic ovariectomized rats. Endocrinology. 2001, 142: 4295-4304. 10.1210/en.142.10.4295.
Bekker PJ, Holloway D, Nakanishi A, Arrighi M, Leese PT, Dunstan CR: The effect of a single dose of osteoprotegerin in postmenopausal women. J Bone Miner Res. 2001, 16: 348-360.
Gravallese EM, Manning C, Tsay A, Naito A, Pan C, Amento E, Goldring SR: Synovial tissue in rheumatoid arthritis is a source of osteoclast differentiation factor. Arthritis Rheum. 2000, 43: 250-258. 10.1002/1529-0131(200002)43:2<250::AID-ANR3>3.0.CO;2-P.
Shigeyama Y, Pap T, Kunzler P, Simmen BR, Gay RE, Gay S: Expression of osteoclast differentiation factor in rheumatoid arthritis. Arthritis Rheum. 2000, 43: 2523-2530. 10.1002/1529-0131(200011)43:11<2523::AID-ANR20>3.0.CO;2-Z.
Lubberts E, Oppers-Walgreen B, Pettit AR, van den Bersselaar L, Joosten LAB, Goldring SR, Gravallese EM, Van den Berg WB: Increase in expression of receptor activator of nuclear factor kB at sites of bone erosion correlates with progression of inflammation in evolving collagen-induced arthritis. Arthritis Rheum. 2002, 46: 3055-3065. 10.1002/art.10607.
Feldmann M, Brennan FM, Maini RN: Role of cytokines in rheumatoid arthritis. Annu Rev Immunol. 1996, 14: 397-440. 10.1146/annurev.immunol.14.1.397.
Lubberts E, van den Bersselaar L, Oppers-Walgreen B, Schwarzenberger P, Coenen-de Roo CJ, Kolls JK, Joosten LA, van den Berg WB: IL-17 promotes bone erosion in murine collagen-induced arthritis through loss of the receptor activator of NF-kappa B ligand/osteoprotegerin balance. J Immunol. 2003, 170: 2655-2662.
Lam J, Takeshita S, Barker JE, Kanagawa O, Ross FP, Teitelbaum SL: TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J Clin Invest. 2000, 106: 1481-1488.
Kong YY, Feige U, Saros I, Bolon B, Tafuri A, Morony S, Capparelli C, Li J, Elliott R, McCabe S, Wong T, Campagnuolo G, Moran E, Bogoch ER, Van G, Nguyen LT, Ohashi PS, Lacey DL, Fish E, Boyle WJ, Penninger JM: Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprote-gerin ligand. Nature. 1999, 402: 304-309. 10.1038/46303.
Romas E, Sims NA, Hards DK, Lindsay M, Quinn JW, Ryan PF, Dunstan CR, Martin TJ, Gillespie MT: Osteoprotegerin reduces osteoclast numbers and prevents bone erosion in collagen-induced arthritis. Am J Pathol. 2002, 161: 1419-1427.
Lubberts E, Joosten LA, Chabaud M, van Den Bersselaar L, Oppers B, Coenen-De Roo CJ, Richards CD, Miossec P, van Den Berg WB: IL-4 gene therapy for collagen arthritis suppresses synovial IL-17 and osteoprotegerin ligand and prevents bone erosion. J Clin Invest. 2000, 105: 1697-1710.
Spector TD, Hall GM, McCloskey EV, Kanis JA: Risk of vertebral fracture in women with rheumatoid arthritis. BMJ. 1993, 306: 558.
Gough AK, Lilley J, Eyre S, Holder RL, Emery P: Generalized bone loss in patients with early rheumatoid arthritis. Lancet. 1994, 344: 23-27. 10.1016/S0140-6736(94)91049-9.
Kvien TK, Haugeberg G, Uhlig T, Falch JA, Halse JI, Lems WF, Dijkmans BA, Woolf AD: Data driven attempt to create a clinical algorithm for identification of women with rheumatoid arthritis at high risk of osteoporosis. Ann Rheum Dis. 2000, 59: 805-811. 10.1136/ard.59.10.805.
Gough A, Sambrook P, Devlin J, Huissoon A, Njeh C, Robbins S, Nguyen T, Emery P: Osteoclastic activation is the principal mechanism leading to secondary osteoporosis in rheumatoid arthritis. J Rheumatol. 1998, 25: 1282-1289.
Schett G, Redlich K, Hayer S, Zwerina J, Bolon B, Dunstan CR, Görtz B, Schulz A, Bergmeister H, Kollias G, Steiner G, Smolen J: Osteoprotegerin protects from generalized bone loss in TNF-transgenic mice. Arthritis Rheum. 2003,
Anderson DM, Maraskovsky E, Billingsley WL, Dougall WC, Tometsko ME, Roux ER, Teepe MC, DuBose RF, Cosman D, Galibert L: A homologue of the TNF receptor and its ligand enhance T-cell growth and dendritic-cell function. Nature. 1997, 390: 175-179. 10.1038/36593.
Shipman CM, Croucher PI: Osteoprotegerin is a soluble decoy receptor for tumor necrosis factor-related apoptosis-inducing ligand/Apo2 ligand and can function as a paracrine survival factor for human myeloma cells. Cancer Res. 2003, 63: 912-916.
Komuro H, Olee T, Kuhn K, Quach J, Brinson DC, Shikhman A, Valbracht J, Creighton-Achermann L, Lotz M: The osteoprotegerin/receptor activator of nuclear factor kappaB/receptor activator of nuclear factor kappaB ligand system in cartilage. Arthritis Rheum. 2001, 44: 2768-2776. 10.1002/1529-0131(200112)44:12<2768::AID-ART464>3.0.CO;2-I.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Schett, G., Redlich, K. & Smolen, J.S. The role of osteoprotegerin in arthritis. Arthritis Res Ther 5, 239 (2003). https://doi.org/10.1186/ar990
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar990