Abstract
The Fourth Canadian Consensus Conference on the Diagnosis and Treatment of Dementia (CCCDTD4) was held 3 to 4 May 2012 in Montreal, Quebec, Canada. A group of neuroimaging experts were assigned the task of reviewing and summarizing the literature on clinical and research applications of different neuroimaging modalities in cognitive disorders. This paper summarizes the literature and recommendations made to the conference regarding the role of several emerging neuroimaging modalities in cognitive disorders. Functional magnetic resonance imaging (MRI), magnetic resonance spectroscopy, and diffusion tensor imaging are discussed in detail within this paper. Other emergent neuroimaging modalities such as positron emission tomography with novel ligands, high-field MRI, arterial spin labeling MRI and noncerebral blood flow single-photon emission computerized tomography are only discussed briefly. Neuroimaging modalities that were recommended at the CCCDTD4 for both clinical and research applications such as amyloid and flurodeoxyglucose positron emission tomography, computerized tomography and structural MRI are discussed in a separate paper by the same authors. A literature search was conducted using the PubMed database including articles in English that involved human subjects and covered the period from the last CCCDTD publication (CCCDTD3; January 2006) until April 2012. Search terms included the name of the specific modality, dementia, Alzheimer's disease, and mild cognitive impairment. A separate search used the same parameters but was restricted to review articles to identify recent evidence-based reviews. Case studies and small case series were not included. Papers representing current evidence were selected, reviewed, and summarized, and the results were presented at the CCCDTD4 meeting with recommendations regarding the utility of various neuroimaging modalities in cognitive disorders. The evidence was graded according to the Oxford Centre for Evidence Based Medicine guidelines. Due to the limitations of current evidence, the neuroimaging modalities discussed in this paper were not recommended for clinical investigation of patients presenting with cognitive impairment. However, in the research setting, each modality provides a unique contribution to the understanding of basic mechanisms and neuropathological markers of cognitive disorders, to the identification of markers for early detection and for the risk of conversion to dementia in the at-risk populations, to the differentiation between different types of cognitive disorders, and to the identification of treatment targets and indicators of treatment response. In conclusion, for all of the neuroimaging modalities discussed in this paper, further studies are needed to establish diagnostic utility such as validity, reliability, and predictive and prognostic value. More multicenter studies are therefore needed with standardized image acquisition, experimental protocols, definition of the clinical population studied, larger numbers of participants, and longer duration of follow-up to allow generalizability of the results to the individual patient.
Similar content being viewed by others
Introduction
Neuroimaging plays a central role in the clinical research of cognitive disorders. A group of Canadian neuroimaging experts were asked to review and summarize the literature, and to provide recommendations regarding the clinical and research applications of different neuroimaging modalities in patients with cognitive impairment to the Fourth Canadian Consensus Conference on the Diagnosis and Treatment of Dementia (CCCDTD4) held 3 to 4 May 2012 in Montreal, Quebec. Other groups have published similar guidelines and recommendations, most recently the European Federation of Neurological Societies guidelines on the use of neuroimaging in the diagnosis of dementia [1].
The group built on other published guidelines, updated the evidence, and presented a rationale for the recommendations to CCCDTD4 in two papers. One paper by the same authors covered neuroimaging modalities currently indicated for clinical use in addition to research in cognitive disorders including [18F]flurodeoxyglucose and [11C]-labeled Pittsburgh compound-B amyloid positron emission tomography (PET), computerized tomography and structural magnetic resonance imaging (MRI). The current paper covers promising neuroimaging modalities that remain in the research realm but are not yet recommended for the clinical investigation of cognitive disorders.
For any medical test to have a diagnostic value in the individual patient, it must have established validity (having being tested across the spectrum of severity with appropriate randomization and compared with a golden diagnostic standard by an independent blinded rater), and to have established sensitivity, specificity, predictive value, and test-retest and inter-rater reliability (Appraisal of Diagnostic Test 2010 [2]). Most of these elements are still lacking for the neuroimaging modalities discussed in this paper. On the other hand, these modalities have important roles in addressing several research questions, such as: identification of the basic mechanisms of cognitive impairment and basic neuropathological markers of cognitive disorders; identification of markers for early detection and differentiation between normal aging, risk state, and dementia; identification of markers for differentiating between different types of cognitive disorders; understanding the neurobiological course of cognitive disorders (for example, changes in neuronal networks as a result of neurodegeneration and brain injury); identification of therapeutic targets and evaluation of the mechanism of action of different therapies in cognitive disorders; and enriching patient selection for therapeutic trials by identifying reliable neuropathological markers for different types of cognitive disorders.
There is significant variability in individuals presenting with cognitive disorders. The variability could be specific to the neuroimaging modality used but it could also be a general variability affecting most test results whether it is clinical, biological or from neuroimaging. In addition to the expected general variability (for example, demographic characteristics, stage of illness, and co-morbidity), there is emerging evidence regarding the impact of cognitive reserve on various test results. This effect was demonstrated in recent neuroimaging studies where regional cerebral blood flow measured by PET scanning was inversely related to the level of education and occupational attainment, indicating higher resiliency in those with higher cognitive reserve in the face of Alzheimer's pathology [3]. Issues related to sources of variability such as cognitive reserve have not been considered adequately in neuroimaging studies at this stage.
The modalities discussed in greatest detail in this expert consensus review are: functional magnetic resonance imaging (fMRI), magnetic resonance spectroscopy (MRS), and diffusion tensor imaging (DTI). Other modalities such as PET imaging with novel ligands, arterial spin-labeling perfusion MRI, high-field MRI, and noncerebral blood flow single-photon emission computerized tomography (SPECT) are only discussed briefly due to the limited literature.
Methodology
A literature search of the PubMed database was performed and covered the period from the last CCCDTD publication (CCCDTD3; January 2006) until April 2012, so as not to duplicate the reviews already performed in the previous meetings [4, 5]. Search terms included the name of the specific neuroimaging modality (fMRI, MRS, or DTI) combined with the terms 'dementia', 'Alzheimer's disease' (AD), or 'mild cognitive impairment' (MCI). The search was limited to 'English' and 'Humans'. A separate search used the same parameters but restricted it to review articles to identify recent evidence-based reviews. The purpose of this process was to summarize the evidence for the consensus meeting and make recommendations regarding the role of emerging neuroimaging modalities in cognitive disorders. This review was therefore focused and selective rather than a systematic review, and the search was not defined by statistical parameters but rather by a series of decisions by the authors to include or not include papers based on the pertinence of the information they contained. This approach resulted in some selected papers being included from the period preceding the interval mentioned above, if they were deemed necessary for a better understanding of the recommendations being made.
The evidence was summarized, and recommendations were submitted to the CCCDTD4 meeting for deliberation towards the goal of reaching a final expert consensus recommendation regarding the role of each selected emerging neuroimaging modality in cognitive disorders based on a majority vote on each of the recommendations by the attending members.
We graded the evidence based on the Oxford CEBM level of evidence grading guidelines (Levels of Evidence, March 2009 [2]). The evidence for the three main neuroimaging modalities discussed in this paper (fMRI, MRS and DTI) is mainly driven from well-designed case-controlled studies with significant heterogeneity of participants and methodology. Therefore, the evidence for these modalities could be graded as 3b.
Functional magnetic resonance imaging
fMRI techniques identify brain activity level based on endogenous blood oxygen level-dependent (BOLD) image contrast. The BOLD signal is the product of the integrated synaptic activity of neurons and is mainly detected by MRI based on hemodynamic change in the oxyhemoglobin/deoxyhemoglobin ratio. An increased BOLD signal is usually interpreted as activation and a negative BOLD response as deactivation of the underlying brain areas [6].
There are mainly two types of fMRI studies used in cognitive disorders: those evaluating brain activation during episodic memory encoding and retrieval, and those evaluating the default mode network.
Studies evaluating brain activation during episodic memory encoding and retrieval in Alzheimer's disease and mild cognitive impairment patients
Typically fMRI experiments compare the MRI signal during one cognitive condition with a control condition such as visual fixation [7].
Episodic memory encoding function is most commonly investigated because of its early and consistent involvement in AD. Successful memory formation and retrieval requires coordinated and reciprocal activation of medial temporal lobe (MTL) structures and deactivation in areas connected to MTL areas such as the posterior cingulate cortex and parietal cortex [8].
During episodic memory encoding, AD patients consistently show lower activation in MTL structures, particularly the hippocampus [9–11], failure of the normal deactivation in posteromedial cortical areas such as the posterior cingulate and medial parietal cortex [12, 13], and increased activation in the prefrontal cortex, probably as a compensation mechanism [14, 15]. Similar pattern emerges during episodic memory retrieval (especially the lower activation of MTL).
In patients with MCI, which is a risk state for AD, the findings are mixed. During episodic memory encoding, some studies reported decreased activity [9, 16, 17] while others reported increased activity in the MTL area. This discrepancy is probably due to several factors such as differences in clinical definition of MCI, severity of cognitive impairment, and level of task performance [18].
Few fMRI studies followed MCI patients longitudinally. In one such study, baseline hyperactivation in MTL structures during episodic encoding correlated with future cognitive decline [19]. Another study showed that this activation declines over time, creating a U-curve pattern from hyperactivation to pseudo-normalization and finally to hypoactivation [20]. Table 1 summarizes the key findings of fMRI studies in AD and MCI patients during episodic memory encoding and retrieval based on published meta-analysis and evidence-based reviews [21–23].
Studies evaluating the default mode network in Alzheimer's disease and mild cognitive impairment patients
The brain network referred to as the default mode network includes several cortical areas that are particularly active at rest and deactivate during cognitive tasks. This network includes the medial prefrontal cortex, posterior cinculate cortex, precuneus, anterior cingulate cortex and parietal cortex. The hippocampus is functionally connected to this network. Recently, the correlation between the intrinsic oscillations or time courses of activity in the hippocampus and different brain regions of the default mode network in cognitive disorders has received significant attention [24]. This technique is feasible in patients with cognitive impairment because of the ease of acquisition and the lack of task performance confounding [25].
A significant alteration in the intrinsic functional connectivity between the hippocampus and areas in the default mode network at rest and during cognitive tasks in patients with MCI and AD has been reported [26–28]. Table 2 summarizes the findings of default mode network imaging studies in the resting state and deactivation during cognitive tasks based on a recent published review [29].
Evaluation of the effect of pharmacological treatment using functional MRI
Cholinergic therapy has been the mainstay for the treatment of cognitive disorders for over two decades. fMRI was used to evaluate the underlying mechanism of cholinergic therapy in healthy subjects and in patients with cognitive disorders. These studies evaluated the changes in the fMRI signal after a single dose and after short-term or long-term exposure to cholinergic agents. There is evidence for changes in the brain activation pattern in key memory, and especially attentional networks in response to cholinergic agents in healthy controls and in patients with MCI and AD during cognitive tasks. On the other hand, a significant variability in the results is observed - most probably due to heterogeneity of treatment response, variability in the pharmacokinetics and pharmacodynamics of these agents, and the inherent test-retest variability in fMRI studies [30]. More recently, a study by Li and colleagues demonstrated enhanced resting state functional connectivity and cerebral blood flow in patients with AD in response to long-term cholinergic treatment [31].
Functional MRI in asymptomatic apolipoprotein E ε4 carriers
fMRI studies in asymptomatic genetically at-risk subjects carrying apolipoprotein E ε4 documented differences in BOLD signal during different cognitive tasks compared with noncarriers, although the direction of this difference and the factors affecting it are quite variable [32]. There are differences in resting state functional connectivity between apolipoprotein E ε2 and ε4 carriers on one end and apolipoprotein E ε3 carriers on the other - the implications of this finding for cognitive disorders remains unclear [33]
Functional MRI in differentiating Alzheimer's disease from non-Alzheimer's disease dementia
Few fMRI studies compared AD with other forms of dementia. A differential pattern of resting state functional connectivity and task-induced BOLD signal has been identified between patients with AD patients compared with those with Lewy body dementia [34, 35]. Other studies identified differential BOLD signal during cognitive tasks between AD patients and those with subcortical vascular cognitive impairment [36] and those with fronto-temporal dementia [37].
Advantages and limitations of functional MRI in cognitive disorders
There are several advantages for fMRI in cognitive disorders as a noninvasive and radioactivity-free modality allowing safe repeated scanning, with relatively high spatial and temporal resolution, and measurement of brain activity during specific behavior (like memory encoding).
On the other hand, fMRI is limited by sensitivity to head motion, effect of task performance, brain atrophy, and transient brain and body states at the time of scanning (for example, arousal, attention, and effort). fMRI is highly dependent on neurovascular coupling, resulting from neuronal and glia activity. This dependency makes fMRI especially vulnerable to the effect of conditions that affect vascular coupling, such as vascular insufficiency, change in blood gas levels, and exposure to substances. Furthermore, a change in activation in one area during a task might be related to a pathological change in other functionally connected areas [38]. Finally, test-retest reliability data for fMRI are just beginning to emerge in cognitive disorders [39].
Conclusion/recommendations
Owing to several limitations, such as variability in image-acquisition protocols and experimental paradigms used, heterogeneity of the clinical population studied, limited data in other forms of dementia, small sample size, limited longitudinal data, limited test-retest reliability data, and inverted U-curve activation patter in the MTL in the people with MCI, fMRI is not currently recommended for the clinical investigation of patients presenting with cognitive impairment (level of evidence 3b).
On the other hand, fMRI holds promise in several areas such as early detection of dementia and predicting conversion of MCI to AD, distinguishing between AD and non-AD dementia, identifying treatment target and changes in brain activation in response to intervention, and evaluating neuropsychiatric and behavioral symptoms in the context of preclinical and clinical dementia. Standardization of image-acquisition protocols and experimental paradigms and establishing validity and reliability data with large number of participants and longer follow-up periods are needed. Resting state methodology is a feasible and promising methodology and can be easily integrated into current large multicenter neuroimaging studies.
[1H]Magnetic resonance spectroscopy
[1H]Magnetic resonance spectroscopy in Alzheimer disease
[1H]MRS is a noninvasive technique used to measure the concentration of low molecular weight metabolites in vivo, with a detection threshold of approximately 1 mmol/l (1 mM). Although MRS data are acquired using a MRI scanner, the method is limited by a low signal to noise ratio resulting in volumes of interest typically ranging between 1 and 8 cm3. Data analysis also involves removal of line-shape distortions, removal of macromolecule/lipid contributions if needed, and fitting of the data to mathematical model functions to increase the accuracy of metabolite-level estimates [40]. The most commonly reported in vivo brain metabolites include N- acetylaspartate (NAA), glutamate, glutamine, choline-containing compounds (Cho), creatine (Cr) compounds and myo-inositol. Altered levels of NAA or NAA/Cr are the most common finding reported in subjects with AD [41–49] and MCI, although alterations in other metabolites including myo-inositol [50], scyllo-inositol [51], and glutamate [52] have been reported. Decreased NAA has been documented in subjects with AD in the occipital lobe [53], temporal lobe [54], parietal lobe [55], and frontal lobe [56].
NAA is an amino acid located primarily within neurons in the central nervous system. The concentration of NAA is among the highest of the free amino acids in the brain (8 to 10 mM in brain tissue) and it normally produces the largest peak in the magnetic resonance spectrum [57]. NAA is considered a marker of neuronal density and/or viability. Reduced NAA may therefore imply neuronal death, or it may indicate neurometabolic impairment based on the known correlation between the rate of mitochondrial activity and NAA synthesis [58]. NAA and myo-inositol change has been noted in the hippocampus in AD, and this change has been associated with cognitive measures [59]. In fact, the NAA/myo-inositol ratio has been shown in several studies to be the most robust marker for discriminating AD patients from age-matched normal older controls [60, 61]. NAA/myo-inositol ratios have also been previously shown to correlate with Mini-Mental State Examination scores [60]. Interested readers are directed to the review by Griffith and colleagues for a detailed description of MRS findings in the dementias [48].
Longitudinal studies in subjects with mild cognitive impairment
The value of MRS as a prognostic indicator of impending dementia in subjects with MCI can only be answered by longitudinal studies. Since 2005 there have been nine longitudinal MRS studies performed in subjects with MCI. Subjects were typically followed for 1 to 3 years to identify a cohort that converted to dementia. The results from these studies are summarized in Table 3.
The most consistent finding reported in MCI subjects that convert to dementia compared with MCI subjects that remain stable is lower NAA or NAA/Cr. Lower levels of NAA/Cr have been noted in several brain regions, including the occipital cortex [62], paratrigonal white matter [63], temporoparietal lobe [64], posterior cingulate [65, 66], and posteriomedial cortex [67]. In the study by Rami and colleagues, lower NAA/Cr was observed in subjects that were classified as prodromal AD and later converted to AD [64]. Kantarci and colleagues demonstrated that NAA/Cr measured from the posterior cingulate added predictive value for conversion to dementia when combined with hippocampal volume [66]. Furthermore, of these studies listed, three have included receiver operator curve analysis. Modrego and colleagues demonstrated that receiver operator curve analysis for NAA/Cr <1.61 predicted conversion with 100% sensitivity and 75% specificity [62]. The area under the curve was 0.91 with a positive predictive value of 83% and a negative predictive value of 100%. Similarly, Fayed and colleagues showed that NAA/Cr <1.40 in the posterior cingulate predicted conversion of MCI to probable AD with sensitivity of 82% and specificity of 72% and an area under the curve of 0.82 [65]. Finally, Modrego and colleagues showed that NAA/Cr <1.43 in the posteromedial parietal cortex predicted conversion to probable AD with 74% sensitivity and 84% specificity and an area under the curve of 0.84 [67].
Despite the consistency of the studies listed above, two studies reported no baseline differences in [1H]MRS between MCI stable patients and MCI converters in the bilateral posterior cingulate and inferior precuneus [68, 69] or in the parietal white matter [69]. Another study showed no differences in the medial temporal lobe in cognitively impaired not demented (CIND) stable patients and CIND converters in the medial temporal lobe [70].
Although current studies show an emerging trend of lower NAA/Cr in MCI subjects that convert to dementia compared with MCI subjects that remain stable, further study is needed. Variability in participant selection, the criteria for conversion to dementia, and methodological inconsistencies in the brain region studied, the spectroscopy acquisition protocol, and the spectroscopy analysis procedures limits the generalizability of the current studies.
Conclusion/recommendations
MRS is not currently recommended for clinical investigation of patients presenting with cognitive impairment due to several limitations discussed above (level of evidence 3b).
On the other hand, [1H]MRS remains a promising technique as a research tool especially for the identification of subjects with MCI who will convert to dementia. Further multisite longitudinal studies should be conducted to establish normative values. Such studies should utilize standardized enrollment criteria, diagnosis criteria and data-acquisition methods, and include automated analysis of spectra that incorporates proper prior knowledge of metabolite line shapes. Future [1H] MRS studies to demonstrate clinical effectiveness should utilize 3 T MRI where available to increase data quality.
Diffusion tensor imaging
Volumetric MRI measures of the MTL or hippocampus have been validated as markers of neuronal damage and can support the diagnosis of early AD [71]. As gray matter atrophy is presumably a relatively downstream event, efforts to detect earlier changes at the micro-structural level are worth pursuing as part of the general effort to define the earliest measurable changes that lead to AD.
Diffusion-weighted imaging has been used clinically over the past 10 to 20 years, mainly to detect acute stroke. This imaging modality can provide a window into the structural integrity of cerebral tissue beyond what is visible on standard MRI. Molecular diffusion refers to the random movements of molecules, which can be described statistically given the size of the molecule and the temperature and nature of the medium through which it travels [72]. In pure water, molecules move in all directions with equal probability (isotropy). Diffusion-weighted imaging uses information derived from the random movements of water molecules through biological tissues; white matter tracts with their neuronal membranes and myelin sheaths interfere with the random movements of water molecules, thus rendering the movements an-isotropic. The main measures obtained are mean diffusivity (MD) and fractional anisotropy (FA). These measures provide indirect information on the microscopic structural properties of white matter fibers [73].
With recent advances in diffusion data modeling, it is now possible to determine in vivo the location of white matter nerve bundles using algorithms that estimate the likelihood that two adjacent voxels are connected (DTI tractography). This type of analysis can provide exquisite detail of the white matter tracts that connect different areas of the brain, including the large-scale neural networks that underlie all cognitive functions [74]. Analysis of DTI data becomes more complex at fiber intersections, and estimates of white matter voxels containing crossing fibers range from 63 to 90% depending on the estimation method used [75]. This implies that most first-generation DTI studies are limited in their power in at least two-thirds of the voxels, enabling clear visualization of only the most prominent white matter tracts such as the cortico-spinal tract. With the emergence of new high angular resolution diffusion imaging methods, it has been possible to manage the problem of crossing fibers and the complex configurations of bundles of white matter [76, 77], enabling much more detailed visualization of smaller white fiber bundles. These tools are well suited to study large-scale brain anatomical connectivity and are particularly well suited for the study of complex brain disorders such as AD.
Several studies in the past decade have focused on the value of DTI measures in the differentiation of MCI and AD from controls; 55 studies comprising close to 2,800 subjects were included in a recent meta-analysis. This analysis compared the contribution of FA and MD to the better established imaging measures of MTL atrophy in the diagnosis of MCI and AD using the magnitude of effect sizes as the method of comparison. Studies using FA measures at the level of regions of interests showed significant differences between AD and controls, with the largest effect sizes in the cingulum, splenium of the corpus callosum, uncinate fasciculus, superior longitudinal fasciculus and frontal lobes. For studies using MD, the regions of interest most useful to distinguish AD from controls were the hippocampus, splenium of the corpus callosum, parietal lobes and temporal lobes. In general, effect sizes were superior for the volumetric MTL measures compared with the DTI measures for the discrimination between controls and AD subjects. Predictably, the differences between MCI and controls were of less magnitude, with only regions of the cingulum showing moderate effect sizes using FA. However, in the comparison between MCI and controls, studies using hippocampal MD showed superior effect sizes compared with volumetric MTL measures [78].
Another recent review, using pooled analysis of regional mean FA and MD values, showed that MD values are different in all white matter regions of the brain between controls and AD subjects, and that FA showed similar results except for the parietal lobe and internal capsule [79]. Furthermore, a few studies in healthy older subjects at risk for AD showed abnormalities in MD values in regions known to be affected in AD [80, 81]. In addition to showing early alterations in MCI patients, DTI appears to correlate with cognitive performance independent of cortical atrophy, which suggests access to an upstream process in the neurodegenerative cascade [82].
The search for appropriate DTI and high angular resolution diffusion imaging parameters for the diagnosis of cognitive impairment is still a work in progress [83]. Various parameters behave in different ways according to localization [84]. In addition to the choice of diffusion parameters, recent tractography studies illustrate the superiority of analysis methods that can manage crossing fibers [85, 86]. The analysis of large-scale networks involved in cognitive functions might enable more specific correlations between brain structure and function [87]. Table 4 summarizes DTI findings in AD and MCI based on the two recently published meta-analyses [78, 79].
Conclusion/recommendations
The DTI technique shows promise as a potential imaging biomarker in the early diagnosis of high-risk states for AD, and has similar accuracy to volumetric hippocampal measures for the diagnosis of established AD. However, due to significant heterogeneity in studies in terms of patient characteristics and image-acquisition parameters, DTI is not currently recommended for the clinical investigation of patients presenting with cognitive impairment (level of evidence 3b).
Potential clinical applications of tractography include support for the diagnosis of neurodegenerative diseases [88], but also identification of amnestic MCI [82, 89] and prediction of progress to AD in risk groups [90, 91]. Further studies with standardized image-acquisition and analysis protocols, a standardized definition of participants, a larger number of participants across age and gender distributions, and a longer follow-up period will increase validity and reliability of the data and allow better generalization of results to the individual patient.
Other emerging neuroimaging modalities used in the evaluation of cognitive disorders
In this section we briefly discuss neuroimaging modalities that hold promise as research tools in cognitive disorders but have less published literature, which limits conclusions and recommendations at this time.
Scanning with emerging PET ligands
PET imaging offers a variety of techniques that have a significant role in investigating patients with cognitive impairment. Amyloid imaging with [11C]-labeled Pittsburgh compound-B amyloid and [18F]flurodeoxyglucose PET are covered elsewhere.
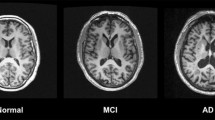
Several novel amyloid ligands are being developed to enhance sensitivity and specificity of PET amyloid imaging and to increase feasibility of scanning by having a longer half-life (see Figure 1 for an example of amyloid binding with the novel ligand [18F]florbetapir). Amyloidbinding SPECT agents are being considered, which will offer another feasible method of imaging amyloid [92].
Amyloid binding with the novel ligand [18F]florbetapir. Axial, sagittal and coronal [18F]florbetapir average images show typical amyloid images in controls and Alzheimer's disease (AD) patients. Blue arrows, cortical uptake; red arrows, white matter (WM) uptake. A negative [18F] florbetapir scan is characterized by a low cortical uptake and high uptake in the adjacent WM. An abnormal scan is characterized by a focal increase of cortical [18F]florbetapir uptake. Increased cortical uptake is evidenced by the reduction between cortical to WM contrast in at least two brain areas. A negative scan indicates sparse to no neuritic plaques, and is inconsistent with a neuropathological diagnosis of AD at the time of image acquisition. A negative scan thus implies reduced likelihood of clinical AD. A positive [18F]florbetapir scan indicates a neuropathology consistent with the presence of moderate to frequent amyloid neuritic plaques. However, the interpretation of a positive scan should take into consideration that amyloid neuritic plaques may also be found in patients with other types of neurologic conditions as well as older people with normal cognition. Images obtained from Alzheimer's Disease Neuroimaging Initiative (ADNI) and processed at PR-N's laboratory.
A molecular probe with high affinity to tubulin associated unit (TAU) fibrils and a low affinity for synthetic amyloid-β1-42 fibrils is in the early phase of development [93].
There is evidence for regional neurotransmitter alteration in AD. Imaging the dopamine system with PET tracers can help to differentiate AD from Lewy Body Dementia (LBD) and LBD from Parkinson's disease. Several PET ligands are available to image the serotonin system; for example, 5-HT1A imaging can reveal hippocampal neurodegeneration in AD, and reduction in 5-HT2A binding has been demonstrated in AD and in MCI patients.
Imaging the cholinergic system offers better understanding of the basic mechanism of cognitive symptoms and response to cholinergic therapies in AD, Parkinson's disease dementia, LBD and other dementia. Cholinergic nicotinic declines have been measured with PET nicotine receptor ligands. Reduced acetyl cholinesterase activity has been shown in MCI converters, AD, LBD and Parkinson's disease dementia compared with healthy controls, and basal acetyl cholinesterase activity predicts therapeutic effects of cholinesterase inhibitors.
Neuroinflammation is a neuropathological feature of numerous neurodegenerative conditions. PET allows for in vivo quantification of various aspects of neuroinflammatory responses, which may serve to monitor the effects of pharmacological interventions. Using PET ligands, high phospholipase enzymatic and high astrocytic activity has been described in the AD brain [94, 95]. Finally, microglial activation detected via specific PET ligand binding has been described in several neurodegenerative conditions. Biomarkers of tissue pathology have potential applications for monitoring disease progression and evaluating the effects of new pharmacological interventions, accumulation abnormal proteins in the brain, neurodegeneration, neuroinflammation and neurotransmission. Table 5 presents common PET ligands used to delineate different neurobiological processes in cognitive disorders. Interested readers are referred to recent published reviews for more details [96, 97].
Arterial spin labeling perfusion magnetic resonance imaging
In this technique, the water content in arterial blood is labeled to detect change in perfusion. This method is similar to [18F]flurodeoxyglucose PET as it detects perfusion change but with no exposure to radioactivity. Recent studies using this method have shown hypoperfusion in some brain areas in MCI and AD patients compared with controls, including the right inferior parietal, bilateral posterior cingulate gyri, and bilateral middle frontal gyri, a pattern of hypoperfusion that is similar the one seen with PET and SPECT scan studies in this population [98, 99].
Noncerebral blood flow-based single-photon emission computerized tomography
Noncerebral blood flow studies can be performed to differentiate LBD from AD with SPECT agents targeting the dopamine cell membrane transporter. [123I]-labeled ioflupane is useful in differentiating Lewy body dementia from AD with high specificity over 90% [100].
Another noncerebral blood flow SPECT approach is based on imaging of the norepinephrine transporter on the plasma membrane of sympathic terminals in the heart, which are lost early in LBD and Parkinson's disease, but not in AD using the ligand iodine-131 metaiodobenzylguanidine. This tracer is approved for human use mostly for the diagnosis and treatment of paragangliomas. Results in small studies have demonstrated above 90% accuracy for the diagnosis of LBD [101, 102].
Ultra-high-field magnetic resonance imaging
The use of ultra-high-field (>3 T) human MRI has increased over the past two decades. The advantages of ultra-high-field MRI include greater signal to noise ratio, reduced scan times, increased image resolution, increased spectral dispersion, and novel contrast. However, there are technical and logistic challenges including increased magnetic field distortions, decreased radio-frequency field homogeneity, increased power deposition, and the unknown safety profile of most surgical implants at field strengths above 3 T. These issues need to be addressed but initial studies have demonstrated the advantages of this technology for the study of the human brain, and AD in particular [103–105].
Discussion
In this expert consensus review, we summarize the literature regarding emerging neuroimaging modalities used to study patients with cognitive impairment that are not currently recommended for the clinical investigation of this population. These modalities have a role in identifying indicators of neuropathology, which has the potential to inform research by providing better markers for inclusion/exclusion in clinical and research protocols in the future. For these neuroimaging modalities to have diagnostic value in the individual patient, they must have established validity and to have established sensitivity, specificity, predictive value, and test-retest and interrater reliability. Most of these elements are still lacking for the modalities discussed in this paper.
International multicenter neuroimaging initiatives are well underway and provide the opportunity for multimodal standardized protocols allowing combining neuroimaging modalities together with clinical and other biological markers (for example, genetics and cerebrospinal fluid) [106]. Some of the neuroimaging modalities discussed in this paper - such as DTI, resting-state fMRI, and MRS - are quite feasible to acquire during MRI studies. Furthermore, post-acquisition processing and analysis is getting more accessible with the advances in image processing and analysis software. Larger longitudinal studies with improved homogeneity of participants and methods, combining neuroimaging and other diagnostic data, will probably give modalities discussed in this paper clinical utility in the near future.
Conclusion
For neuroimaging modalities discussed in this paper, further studies are needed to establish diagnostic utility. Larger, multicenter, multimodal studies with better homogeneity of the clinical population and methodology are therefore needed to establish diagnostic value for the individual patient.
Abbreviations
- AD:
-
Alzheimer's disease
- BOLD:
-
blood oxygen level dependent
- CCCDTD4:
-
Fourth Canadian Consensus Conference on the Diagnosis and Treatment of Dementia
- CIND:
-
cognitively impaired not demented
- Cr:
-
creatine
- DTI:
-
diffusion tensor imaging
- FA:
-
fractional anisotropy
- fMRI:
-
functional magnetic resonance imaging
- LBD:
-
Lewy Body Dementia
- MCI:
-
mild cognitive impairment
- MD:
-
mean diffusivity
- MRI:
-
magnetic resonance imaging
- MRS:
-
magnetic resonance spectroscopy
- MTL:
-
medial temporal lobe
- NAA:
-
N-acetylaspartate
- PET:
-
positron emission tomography
- SPECT:
-
single-photon emission computerized tomography.
References
Filippi M, Agosta F, Barkhof F, Dubois B, Fox NC, Frisoni GB, Jack CR, Johannsen P, Miller B, Nestor PJ, Scheltens P, Sorbi S, Teipel S, Thompson PM, Wahlund L-O: EFNS task force: the use of neuroimaging in the diagnosis of dementia. Eur J Neurol. 2012, 19: 1487-1501. 10.1111/j.1468-1331.2012.03859.x. PMID:22900895
Oxford Centre of Evidence Based Medicine. [http://www.cebm.net]
Stern Y: Cognitive reserve in ageing and Alzheimer's disease. Lancet Neurol. 2012, 11: 1006-1012. 10.1016/S1474-4422(12)70191-6. PMID:23079557
Chow T: Structural neuroimaging in the diagnosis of dementia. Alzheimers Dement. 2007, 3: 333-335. 10.1016/j.jalz.2007.07.016. PMID:19595954
Borrie M: Functional neuroimaging in the diagnosis of dementia. Alzheimers Dement. 2007, 3: 336-340. 10.1016/j.jalz.2007.07.004. PMID:19595955
Logothetis NK, Pauls J, Augath M, Trinath T, Oeltermann A: Neurophysiological investigation of the basis of the fMRI signal. Nature. 2001, 412: 150-157. 10.1038/35084005. PMID:11449264
Malonek D, Grinvald A: Interactions between electrical activity and cortical microcirculation revealed by imaging spectroscopy: implications for functional brain mapping. Science. 1996, 272: 551-554. 10.1126/science.272.5261.551. PMID:8614805
Miller SL, Celone K, DePeau K, Diamond E, Dickerson BC, Rentz D, Pihlajamäki M, Sperling RA: Age-related memory impairment associated with loss of parietal deactivation but preserved hippocampal activation. Proc Natl Acad Sci USA. 2008, 105: 2181-2186. 10.1073/pnas.0706818105. PMID:18238903
Machulda MM, Ward HA, Borowski B, Gunter JL, Cha RH, O'Brien PC, Petersen RC, Boeve BF, Knopman D, Tang-Wai DF, Ivnik RJ, Smith GE, Tangalos EG, Jack CR: Comparison of memory fMRI response among normal, MCI, and Alzheimer's patients. Neurology. 2003, 61: 500-506. 10.1212/01.WNL.0000079052.01016.78. PMID:12939424
Golby A, Si lverberg G, Race E, Gabrieli S, O'Shea J, Knierim K, Stebbins G, Gabrieli J: Memory encoding in Alzheimer's disease: an fMRI study of explicit and implicit memory. Brain. 2005, 128: 773-787. 10.1093/brain/awh400. PMID:15705615
Sperling RA, Bates JF, Chua EF, Cocchiarella AJ, Rentz DM, Rosen BR, Schacter DL, Albert MS: fMRI studies of associative encoding in young and elderly controls and mild Alzheimer's disease. J Neurol Neurosurg Psychiatry. 2003, 74: 44-50. 10.1136/jnnp.74.1.44. PMID:12486265
Miettinen P S, Pihlajamäki M, Jauhiainen AM, Niskanen E, Hänninen T, Vanninen R, Soininen H: Structure and function of medial temporal and posteromedial cortices in early Alzheimer's disease. Eur J Neurosci. 2011, 34: 320-330. 10.1111/j.1460-9568.2011.07745.x. PMID:21692882
Lustig C, Snyder AZ, Bhakta M, O'Brien KC, McAvoy M, Raichle ME, Morris JC, Buckner RL: Functional deactivations: change with age and dementia of the Alzheimer type. Proc Natl Acad Sci USA. 2003, 100: 14504-14509. 10.1073/pnas.2235925100. PMID:14608034
Solé-Padullés C, Bartrés-Faz D, Junqué C, Vendrell P, Rami L, Clemente IC, Bosch B, Villar A, Bargalló N, Jurado MA, Barrios M, Molinuevo JL: Brain structure and function related to cognitive reserve variables in normal aging, mild cognitive impairment and Alzheimer's disease. Neurobiol Aging. 2009, 30: 1114-1124. 10.1016/j.neurobiolaging.2007.10.008. PMID:18053618
Grady CL, McI ntosh AR, Beig S, Keightley ML, Burian H, Black SE: Evidence from functional neuroimaging of a compensatory prefrontal network in Alzheimer's disease. J Neurosci. 2003, 23: 986-993. PMID:12574428
Johnson SC, Schmitz TW, Moritz CH, Meyerand ME, Rowley HA, Alexander AL, Hansen KW, Gleason CE, Carlsson CM, Ries ML, Asthana S, Chen K, Reiman EM, Alexander GE: Activation of brain regions vulnerable to Alzheimer's disease: the effect of mild cognitive impairment. Neurobiol Aging. 2006, 27: 1604-1612. 10.1016/j.neurobiolaging.2005.09.017. PMID:16226349
Petrella JR, Krishnan S, Slavin MJ, Tran TT, Murty L, Doraiswamy PM: Mild cognitive impairment: evaluation with 4-T functional MR imaging. Radiology. 2006, 240: 177-186. 10.1148/radiol.2401050739. PMID:16684919
Dickerson BC, Sperling RA: Functional abnormalities of the medial temporal lobe memory system in mild cognitive impairment and Alzheimer's disease: insights from functional MRI studies. Neuropsychologia. 2008, 46: 1624-1635. 10.1016/j.neuropsychologia.2007.11.030. PMID:18206188
Miller SL, Fenstermacher E, Bates J, Blacker D, Sperling RA, Dickerson BC: Hippocampal activation in adults with mild cognitive impairment predicts subsequent cognitive decline. J Neurol Neurosurg Psychiatry. 2008, 79: 630-635. PMID:17846109
O'Brien JL, O'Keefe KM, LaViolette PS, DeLuca AN, Blacker D, Dickerson BC, Sperling RA: Longitudinal fMRI in elderly reveals loss of hippocampal activation with clinical decline. Neurology. 2010, 74: 1969-1976. 10.1212/WNL.0b013e3181e3966e. PMID:20463288
Schwindt GC, Black SE: Functional imaging studies of episodic memory in Alzheimer's disease: a quantitative meta-analysis. NeuroImage. 2009, 45: 181-190. 10.1016/j.neuroimage.2008.11.024. PMID:19103293
Ries ML, Carlsson CM, Rowley HA, Sager MA, Gleason CE, Asthana S, Johnson SC: Magnetic resonance imaging characterization of brain structure and function in mild cognitive impairment: a review. J Am Geriatr Soc. 2008, 56: 920-934. 10.1111/j.1532-5415.2008.01684.x. PMID:18410325
Dickerson BC, Sperling RA: Large-scale functional brain network abnormalities in Alzheimer's disease: insights from functional neuroimaging. Behav Neurol. 2009, 21: 63-75. 10.1155/2009/610392. PMID:19847046
Biswal B, Yetkin FZ, Haughton VM, Hyde JS: Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med. 1995, 34: 537-541. 10.1002/mrm.1910340409. PMID:8524021
Fleisher AS, Sherzai A, Taylor C, Langbaum JB, Chen K, Buxton RB: Restingstate BOLD networks versus task-associated functional MRI for distinguishing Alzheimer's disease risk groups. Neuroimage. 2009, 47: 1678-1690. 10.1016/j.neuroimage.2009.06.021. PMID:19539034
Rombouts SA, Barkhof F, Goekoop R, Stam CJ, Scheltens P: Altered resting state networks in mild cognitive impairment and mild Alzheimer's disease: an fMRI study. Hum Brain Mapp. 2005, 26: 231-239. 10.1002/hbm.20160. PMID:15954139
Gili T, Cercignani M, Serra L, Perri R, Giove F, Maraviglia B, Caltagirone C, Bozzali M: Regional brain atrophy and functional disconnection across Alzheimer's disease evolution. J Neurol Neurosurg Psychiatry. 2011, 82: 58-66. 10.1136/jnnp.2009.199935. PMID:20639384
Wang Z, Yan C, Zhao C, Qi Z, Zhou W, Lu J, He Y, Li K: Spatial patterns of intrinsic brain activity in mild cognitive impairment and Alzheimer's disease: a resting-state functional MRI study. Hum Brain Mapp. 2011, 32: 1720-1740. 10.1002/hbm.21140. PMID:21077137
Hafkemeijer A, van der Grond J, Rombouts SA: Imaging the default mode network in aging and dementia. Biochim Biophys Acta. 2012, 1822: 431-441. 10.1016/j.bbadis.2011.07.008. PMID:21807094
Venneri A: Imaging treatment effects in Alzheimer's disease. Magn Reson Imaging. 2007, 25: 953-968. 10.1016/j.mri.2007.02.004. PMID:17446028
Li W, Antuono PG, Xie C, Chen G, Jones JL, Ward BD, Franczak MB, Goveas JS, Li SJ: Changes in regional cerebral blood flow and functional connectivity in the cholinergic pathway associated with cognitive performance in subjects with mild Alzheimer's disease after 12-week donepezil treatment. NeuroImage. 2012, 60: 1083-1091. 10.1016/j.neuroimage.2011.12.077. PMID:22245641
Trachtenberg AJ, Filippini N, Mackay CE: The effects of APOE-epsilon4 on the BOLD response. Neurobiol Aging. 2012, 33: 323-334. 10.1016/j.neurobiolaging.2010.03.009. PMID:20409610
Trachtenberg AJ, Fil ippini N, Ebmeier KP, Smith SM, Karpe F, Mackay CE: The effects of APOE on the functional architecture of the resting brain. NeuroImage. 2012, 59: 565-572. 10.1016/j.neuroimage.2011.07.059. PMID:21851856
Galvin JE, Price JL, Yan Z, Morris JC, Sheline YI: Resting bold fMRI differentiates dementia with Lewy bodies vs Alzheimer disease. Neurology. 2011, 76: 1797-1803. 10.1212/WNL.0b013e31821ccc83. PMID:21525427
Sauer J, ffytche DH, Ballard C, Brown RG, Howard R: Differences between Alzheimer's disease and dementia with Lewy bodies: an fMRI study of task-related brain activity. Brain. 2006, 129: 1780-1788. 10.1093/brain/awl102. PMID:16670180
Li C, Zheng J, Wang J, Gui L: Comparison between Alzheimer's disease and subcortical vascular dementia: attentional cortex study in functional magnetic resonance imaging. J Int Med Res. 2011, 39: 1413-1419. 10.1177/147323001103900428. PMID:21986142
Rombouts SA, van Swieten JC, Pijnenburg YA, Goekoop R, Barkhof F, Scheltens P: Loss of frontal fMRI activation in early frontotemporal dementia compared to early AD. Neurology. 2003, 60: 1904-1908. 10.1212/01.WNL.0000069462.11741.EC. PMID:12821731
Sperling R: Potential of functional MRI as a biomarker in early Alzheimer'sdisease. Neurobiol Aging. 2011, 32 (Suppl 1): S37-S43. PMID:22078171
Clement F, Belleville S: Test-retest reliability of fMRI verbal episodic memory paradigms in healthy older adults and in persons with mild cognitive impairment. Hum Brain Mapp. 2009, 30: 4033-4047. 10.1002/hbm.20827. PMID:19492301
Bartha R, Drost DJ, Williamson PC: Factors affecting the quantification of short echo in-vivo 1H MR spectra: prior knowledge, peak elimination, and filtering. NMR Biomed. 1999, 12: 205-216. 10.1002/(SICI)1099-1492(199906)12:4<205::AID-NBM558>3.0.CO;2-1. PMID:10421912
Rapoport SI: Hydrogen magnetic resonance spectroscopy in Alzheimer's disease. Lancet Neurol. 2002, 1: 82-10.1016/S1474-4422(02)00035-2. PMID:12849509
Loos C, Achten E, Santens P: Proton magnetic resonance spectroscopy in Alzheimer's disease, a review. Acta Neurol Belg. 2010, 110: 291-298. PMID:21305856
Kantarci K: 1H magnetic resonance spectroscopy in dementia. Br J Radiol. 2007, 80 (Spec No 2): S146-S152. PMID:18445744
Lehericy S, Marjanska M, Mesrob L, Sarazin M, Kinkingnehun S: Magnetic resonance imaging of Alzheimer's disease. Eur Radiol. 2007, 17: 347-362. 10.1007/s00330-006-0341-z. PMID:16865367
Modrego PJ: Predictors of conversion to dementia of probable Alzheimer type in patients with mild cognitive impairment. Curr Alzheimer Res. 2006, 3: 161-170. 10.2174/156720506776383103. PMID:16611017
Jones RS, Waldman AD: 1H-MRS evaluation of metabolism in Alzheimer's disease and vascular dementia. Neurol Res. 2004, 26: 488-495. 10.1179/016164104225017640. PMID:15265265
Valenzuela MJ, Sachdev P: Magnetic resonance spectroscopy in AD. Neurology. 2001, 56: 592-598. 10.1212/WNL.56.5.592. PMID:11261442
Griffith HR, Stewart CC, den Hollander JA: Proton magnetic resonance spectroscopy in dementias and mild cognitive impairment. Int Rev Neurobiol. 2009, 84: 105-131. PMID:19501715
Fayed N, Modrego PJ, Salinas GR, Gazulla J: Magnetic resonance imaging based clinical research in Alzheimer's disease. J Alzheimers Dis. 2012, 31 (Suppl 3): S5-S18. PMID:22233763
Siger M, Schuff N, Z hu X, Miller BL, Weiner MW: Regional myo-inositol concentration in mild cognitive impairment using 1H magnetic resonance spectroscopic imaging. Alzheimer Dis Assoc Disord. 2009, 23: 57-62. 10.1097/WAD.0b013e3181875434. PMID:18725861
Griffith HR, den Hollander JA, Stewart CC, Evanochko WT, Buchthal SD, Harrell LE, Zamrini EY, Brockington JC, Marson DC: Elevated brain scyllo-inositol concentrations in patients with Alzheimer's disease. NMR Biomed. 2007, 20: 709-716. 10.1002/nbm.1132. PMID:17295394
Rupsingh R, Borrie M, Smith M, Wells JL, Bartha R: Reduced hippocampal glutamate in Alzheimer disease. Neurobiol Aging. 2011, 32: 802-810. 10.1016/j.neurobiolaging.2009.05.002. PMID:19501936
Moats RA, Ernst T, S honk TK, Ross BD: Abnormal cerebral metabolite concentrations in patients with probable Alzheimer disease. Magn Reson Med. 1994, 32: 110-115. 10.1002/mrm.1910320115. PMID:8084225
Kantarci K, Jack CR, Xu YC, Campeau NG, O'Brien PC, Smith GE, Ivnik RJ, Boeve BF, Kokmen E, Tangalos EG, Petersen RC: Regional metabolic patterns in mild cognitive impairment and Alzheimer's disease: a 1H MRS study. Neurology. 2000, 55: 210-217. 10.1212/WNL.55.2.210. PMID:10908893
Miller BL, Moats RA, Shonk T, Ernst T, Woolley S, Ross BD: Alzheimer disease: depiction of increased cerebral myo-inositol with proton MR spectroscopy. Radiology. 1993, 187: 433-437. PMID:8475286
Deicken RF, Zhou L, Schuff N, Fein G, Weiner MW: Hippocampal neuronal dysfunction in schizophrenia as measured by proton magnetic resonance spectroscopy. Biol Psychiatry. 1998, 43: 483-488. 10.1016/S0006-3223(97)00490-3. PMID:9547926
Pouwels PJ, Frahm J: Regional metabolite concentrations in human brain as determined by quantitative localized proton MRS. Magn Reson Med. 1998, 39: 53-60. 10.1002/mrm.1910390110. PMID:9438437
Bates TE, Strangward M, Keelan J, Davey GP, Munro PM, Clark JB: Inhibition of N-acetylaspartate production: implications for 1H MRS studies in vivo. Neuroreport. 1996, 7: 1397-1400. 10.1097/00001756-199605310-00014. PMID:8856684
Jessen F, Block W, T räber F, Keller E, Flacke S, Lamerichs R, Schild HH, Heun R: Decrease of N-acetylaspartate in the MTL correlates with cognitive decline of AD patients. Neurology. 2001, 57: 930-932. 10.1212/WNL.57.5.930. PMID:11552037
Rose SE, de Zubicaray GI, Wang D, Galloway GJ, Chalk JB, Eagle SC, Semple J, Doddrell DM: A 1H MRS study of probable Alzheimer's disease and normal aging: implications for longitudinal monitoring of dementia progression. Magn Reson Imaging. 1999, 17: 291-299. 10.1016/S0730-725X(98)00168-4. PMID:10215485
Parnetti L, Tarducci R, Presciutti O, Lowenthal DT, Pippi M, Palumbo B, Gobbi G, Pelliccioli GP, Senin U: Proton magnetic resonance spectroscopy can differentiate Alzheimer's disease from normal aging. Mech Ageing Dev. 1997, 97: 9-14. 10.1016/S0047-6374(97)01877-0. PMID:9223122
Modrego PJ, Fayed N, Pina MA: Conversion from mild cognitive impairment to probable Alzheimer's disease predicted by brain magnetic resonance spectroscopy. Am J Psychiatry. 2005, 162: 667-675. 10.1176/appi.ajp.162.4.667. PMID:15800137
Metastasio A, Rinaldi P, Tarducci R, Mariani E, Feliziani FT, Cherubini A, Pelliccioli GP, Gobbi G, Senin U, Mecocci P: Conversion of MCI to dementia: role of proton magnetic resonance spectroscopy. Neurobiol Aging. 2006, 27: 926-932. 10.1016/j.neurobiolaging.2005.05.002. PMID:15936850
Rami L, Gómez-Anson B, Sanchez-Valle R, Bosch B, Monte GC, Lladó A, Molinuevo JL: Longitudinal study of amnesic patients at high risk for Alzheimer's disease: clinical, neuropsychological and magnetic resonance spectroscopy features. Dement Geriatr Cogn Disord. 2007, 24: 402-410. 10.1159/000109750. PMID:17934274
Fayed N, Davila J, Oliveros A, Castillo J, Medrano JJ: Utility of different MR modalities in mild cognitive impairment and its use as a predictor of conversion to probable dementia. Acad Radiol. 2008, 15: 1089-1098. 10.1016/j.acra.2008.04.008. PMID:18692749
Kantarci K, Weigand SD, Przybelski SA, Shiung MM, Whitwell JL, Negash S, Knopman DS, Boeve BF, O'Brien PC, Petersen RC, Jack CR: Risk of dementia in MCI: combined effect of cerebrovascular disease, volumetric MRI, and 1H MRS. Neurology. 2009, 72: 1519-1525. 10.1212/WNL.0b013e3181a2e864. PMID:19398707
Modrego PJ, Fayed N, Sarasa M: Magnetic resonance spectroscopy in the prediction of early conversion from amnestic mild cognitive impairment to dementia: a prospective cohort study. BMJ Open. 2011, 1: e000007-10.1136/bmjopen-2010-000007. PMID:22021723
Kantarci K, Weigand SD, Petersen RC, Boeve BF, Knopman DS, Gunter J, Reyes D, Shiung M, O'Brien PC, Smith GE, Ivnik RJ, Tangalos EG, Jack CR: Longitudinal 1H MRS changes in mild cognitive impairment and Alzheimer's disease. Neurobiol Aging. 2007, 28: 1330-1339. 10.1016/j.neurobiolaging.2006.06.018. PMID:16860440
Pilatus U, Lais C, Rochmont Adu M, Kratzsch T, Frölich L, Maurer K, Zanella FE, Lanfermann H, Pantel J: Conversion to dementia in mild cognitive impairment is associated with decline of N-actylaspartate and creatine as revealed by magnetic resonance spectroscopy. Psychiatry Res. 2009, 173: 1-7. 10.1016/j.pscychresns.2008.07.015. PMID:19427767
Chao LL, Schuff N, Kramer JH, Du AT, Capizzano AA, O'Neill J, Wolkowitz OM, Jagust WJ, Chui HC, Miller BL, Yaffe K, Weiner MW: Reduced medial temporal lobe N-acetylaspartate in cognitively impaired but nondemented patients. Neurology. 2005, 64: 282-289. 10.1212/01.WNL.0000149638.45635.FF. PMID:15668426
Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, Delacourte A, Galasko D, Gauthier S, Jicha G, Meguro K, O'Brien J, Pasquier F, Robert P, Rossor M, Salloway S, Stern Y, Visser PJ, Scheltens P: Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria. Lancet Neurol. 2007, 6: 734-746. 10.1016/S1474-4422(07)70178-3. PMID:17616482
Le Bihan D, Johansen-Berg H: Diffusion MRI at 25: exploring brain tissue structure and function. NeuroImage. 2012, 61: 324-341. 10.1016/j.neuroimage.2011.11.006. PMID:22120012
Assaf Y, Pasternak O: Diffusion tensor imaging (DTI)-based white matter mapping in brain research: a review. J Mol Neurosci. 2008, 34: 51-61. 10.1007/s12031-007-0029-0. PMID:18157658
Mesulam MM: Large-scalen eurocognitive networks and distributed processing for attention, language, and memory. Ann Neurol. 1990, 28: 597-613. 10.1002/ana.410280502. PMID:2260847
Jeurissen B, Leemans A, T ournier JD, Jones DK, Sijbers J: Investigating the prevalence of complex fiber configurations in white matter tissue with diffusion magnetic resonance imaging. Hum Brain Mapp. 2012, doi: 101002/hbm22099. PMID:22611035
Descoteaux M, Deriche R, Knosche TR, Anwander A: Deterministic and probabilistic tractography based on complex fibre orientation distributions. IEEE Trans Med Imaging. 2009, 28: 269-286. PMID:19188114
Tournier JD, Mori S, Leemans A: Diffusion tensor imaging and beyond. Magn Reson Med. 2011, 65: 1532-1556. 10.1002/mrm.22924. PMID:21469191
Clerx L, Visser PJ, Verhey F, Aalten P: New MRI markers for Alzheimer's disease: a meta-analysis of diffusion tensor imaging and a comparison with medial temporal lobe measurements. J Alzheimers Dis. 2012, 29: 405-429. PMID:22330833
Sexton CE, Kalu UG, Filippini N, Mackay CE, Ebmeier KP: A meta-analysis of diffusion tensor imaging in mild cognitive impairment and Alzheimer's disease. Neurobiol Aging. 2011, 32: 2322.e5-e18. 10.1016/j.neurobiolaging.2010.05.019. PMID:20619504
Bendlin BB, Ries ML, Canu E, Sodhi A, Lazar M, Alexander AL, Carlsson CM, Sager MA, Asthana S, Johnson SC: White matter is altered with parental family history of Alzheimer's disease. Alzheimers Dement. 2010, 6: 394-403. 10.1016/j.jalz.2009.11.003. PMID:20713315
Gold BT, Johnson NF, Powe ll DK, Smith CD: White matter integrity andvulnerability to Alzheimer's disease: preliminary findings and future directions. Biochim Biophys Acta. 2012, 1822: 416-422. 10.1016/j.bbadis.2011.07.009. PMID:21803153
Grambaite R, Reinvang I, Selnes P, Fjell AM, Walhovd KB, Stenset V, Fladby T: Pre-dementia memory impairment is associated with white matter tract affection. J Int Neuropsychol Soc. 2011, 17: 143-153. 10.1017/S1355617710001360. PMID:21092388
Bozoki AC, Korolev IO, Davis NC, Hoisington LA, Berger KL: Disruption of limbic white matter pathways in mild cognitive impairment and Alzheimer's disease: a DTI/FDG-PET study. Hum Brain Mapp. 2012, 33: 1792-1802. 10.1002/hbm.21320. PMID:21674695
Wang PN, Chou KH, Lirng J F, Lin KN, Chen WT, Lin CP: Multiple diffusivities define white matter degeneration in amnestic mild cognitive impairment and Alzheimer's disease. J Alzheimers Dis. 2012, 30: 423-437. PMID:22430530
Douaud G, Jbabdi S, Behre ns TE, Menke RA, Gass A, Monsch AU, Rao A, Whitcher B, Kindlmann G, Matthews PM, Smith S: DTI measures in crossingfibre areas: increased diffusion anisotropy reveals early white matter alteration in MCI and mild Alzheimer's disease. Neuroimage. 2011, 55: 880-890. 10.1016/j.neuroimage.2010.12.008. PMID:21182970
Raffelt D, Tournier JD, Rose S, Ridgway GR, Henderson R, Crozier S, Salvado O, Connelly A: Apparent fibre density: a novel measure for the analysis of diffusion-weighted magnetic resonance images. Neuroimage. 2012, 59: 3976-3994. 10.1016/j.neuroimage.2011.10.045. PMID:22036682
Bosch B, Arenaza-Urquijo EM, Rami L, Sala-Llonch R, Junqué C, Solé-Padullés C, Peña-Gómez C, Bargalló N, Molinuevo JL, Bartrés-Faz D: Multiple DTI index analysis in normal aging, amnestic MCI and AD. Relationship with neuropsychological performance. Neurobiol Aging. 2012, 33: 61-74. 10.1016/j.neurobiolaging.2010.02.004. PMID:20371138
Ciccarelli O, Catani M, Johansen-Berg H, Clark C, Thompson A: Diffusionbased tractography in neurological disorders: concepts, applications, and future developments. Lancet Neurol. 2008, 7: 715-727. 10.1016/S1474-4422(08)70163-7. PMID:18635020
Cui Y, Wen W, Lipnicki DM, Beg MF, Jin JS, Luo S, Zhu W, Kochan NA, Reppermund S, Zhuang L, Raamana PR, Liu T, Trollor JN, Wang L, Brodaty H, Sachdev PS: Automated detection of amnestic mild cognitive impairment in community-dwelling elderly adults: a combined spatial atrophy and white matter alteration approach. NeuroImage. 2012, 59: 1209-1217. 10.1016/j.neuroimage.2011.08.013. PMID:21864688
Oishi K, Akhter K, Mielke M, Ceritoglu C, Zhang J, Jiang H, Li X, Younes L, Miller MI, van Zijl PC, Albert M, Lyketsos CG, Mori S: Multi-modal MRI analysis with disease-specific spatial filtering: initial testing to predict mild cognitive impairment patients who convert to Alzheimer's disease. Front Neurol. 2011, 2: 54-PMID:21904533
Persson J, Lind J, Larsson A, Ingvar M, Cruts M, Van Broeckhoven C, Adolfsson R, Nils son LG, Nyberg L: Altered brain white matter integrity in healthy carriers of the APOE epsilon4 allele: a risk for AD?. Neurology. 2006, 66: 1029-1033. 10.1212/01.wnl.0000204180.25361.48. PMID:16606914
Cheng Y, Ono M, Kimura H, Ueda M, Saji H: Technetium-99m labeled pyridyl benzofuran derivatives as single photon emission computed tomography imaging probes for beta-amyloid plaques in Alzheimer's brains. J Med Chem. 2012, 55: 2279-2286. 10.1021/jm201513c. PMID:22364445
Fodero-Tavoletti MT, Okamura N, Furumoto S, Mulligan RS, Connor AR, McLean CA, Cao D, Rigopoulos A, Cartwright GA, O'Keefe G, Gong S, Adlard PA, Barnham KJ, Rowe CC, Masters CL, Kudo Y, Cappai R, Yanai K, Villemagne VL: 18F-THK523: a novel in vivo tau imaging ligand for Alzheimer's disease. Brain. 2011, 134 (Pt 4): 1089-1100. PMID:21436112
Esposito G, Giovacchini G, Liow JS, Bhattacharjee AK, Greenstein D, Schapiro M, Hallett M, Herscovitch P, Eckelman WC, Carson RE, Rapoport SI: Imaging neuroinflammation in Alzheimer's disease with radiolabeled arachidonic acid and PET. J Nucl Med. 2008, 49: 1414-1421. 10.2967/jnumed.107.049619. PMID:18703605
Santillo AF, Gambini JP, Lannfelt L, Långström B, Ulla-Marja L, Kilander L, Engler H: In vivo imaging of astrocytosis in Alzheimer's disease: an (1)(1) C-L-deuteriodeprenyl and PIB PET study. Eur J Nucl Med Mol Imaging. 2011, 38: 2202-2208. 10.1007/s00259-011-1895-9. PMID:21853308
Herholz K, Carter SF, Jones M: Positron emission tomography imaging in dementia. Br J R adiol. 2007, 80 (Spec No 2): S160-S167. PMID:18445746
Mori T, Maeda J, Shimada H, Higuchi M, Shinotoh H, Ueno S, Suhara T: Molecular imaging of dementia. Psychogeriatrics. 2012, 12: 106-114. 10.1111/j.1479-8301.2012.00409.x. PMID:22712644
Johnson NA, Jahng GH, Weiner MW, Miller BL, Chui HC, Jagust WJ, Gorno-Tempini ML, Schuff N: Pattern of cerebral hypoperfusion in Alzheimer disease and mild cognitive impairment measured with arterial spinlabeling MR imaging: initial experience. Radiology. 2005, 234: 851-859. 10.1148/radiol.2343040197. PMID:15734937
Alsop DC, Detre JA, Grossman M: Assessment of cerebral blood flow in Alzheimer's disease by spin-labeled magnetic resonance imaging. Ann Neurol. 2000, 47: 93-100. 10.1002/1531-8249(200001)47:1<93::AID-ANA15>3.0.CO;2-8. PMID:10632106
Cummings JL, Henchcliffe C, Schaier S, Simuni T, Waxman A, Kemp P: The role of dopaminergic imaging in patients with symptoms of dopaminergic system neurodegeneration. Brain. 2011, 134 (Pt 11): 3146-3166. PMID:21810889
Hanyu H, Shimizu S, Hirao K, Kanetaka H, Iwamoto T, Chikamori T, Usui Y, Yamashina A, Koizumi K, Abe K: Comparative value of brain perfusion SPECT and [(123)I]MIBG myocardial scintigraphy in distinguishing between dementia with Lewy bodies and Alzheimer's disease. Eur J Nucl Med Mol Imaging. 2006, 33: 248-253. 10.1007/s00259-005-1921-x. PMID:16328506
Suzuki M, Kurita A, Hashimoto M, Fukumitsu N, Abo M, Ito Y, Urashima M, Inoue K: Impaired myocardial 123I-metaiodobenzylguanidine uptake in Lewy body disease: comparison between dementia with Lewy bodies and Parkinson's disease. J Neurol Sci. 2006, 240: 15-19. 10.1016/j.jns.2005.08.011. PMID:16199056
Kerchner GA: Ultra-high field 7T MRI: a new tool for studying Alzheimer's disease. J Alzheimers Dis. 2011, 26 (Suppl 3): 91-95. PMID:21971453
van der Kolk AG, Hendrikse J, Zwanenburg JJ, Visser F, Luijten PR: Clinical applications of 7T MRI in the brain. Eur J Radiol. 2013, 82: 708-718. 10.1016/j.ejrad.2011.07.007. PMID:21937178
Thomas BP, Welch EB, Niederhauser BD, Whetsell WO, Anderson AW, Gore JC, Avison MJ, Creasy JL: High-resolution 7T MRI of the human hippocampus in vivo. J Magn Reson Imaging. 2008, 28: 1266-1272. 10.1002/jmri.21576. PMID:18972336
Carrillo MC, Bain LJ, Frisoni GB, Weiner MW: Worldwide Alzheimer's disease neuroimaging initiative. Alzheimers Dement. 2012, 8: 337-342. 10.1016/j.jalz.2012.04.007. PMID:22748939
Acknowledgements
RB would like to acknowledge the Ivey-BMO Financial Group Scientist in Brain Disorders Imaging Award. PR-N acknowledges support from the Le Fonds de recherche du Québec - Santé (FRQS) chercheurs-boursiers program, Canadian Institutes of Health Research, Alzheimer's Association and Aisenstadt Foundation.
Declarations
This article has been published as part of Alzheimer's Research & Therapy Volume 5 Supplement 1, 2013: Background documents to the 4th Canadian Consensus Conference on the Diagnosis and Treatment of Dementia (CCCDTD4). The full contents of the supplement are available online at http://alzres.com/supplements/5/S1
Publication charges for the supplement were funded by the Canadian Consensus Conference on the Diagnosis and Treatment of Dementia (CCCDTD). Although residual conference funds used include contributions from pharmaceutical companies, no commercial organization has been involved in the selection of participants, choice of topics, preparation of background papers or recommendations. In kind support was also provided by the Canadian Dementia Knowledge Translation Network, and the offices of Drs Serge Gauthier (McGill University), Christopher Patterson (McMaster University) and Howard Chertkow (McGill University), whose role as Guest Editors involved the coordination of the project without involvement in the journal's standard peer review process which applied for all articles.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
RB is co-founder and Chief Scientific Officer of Bioscape Imaging Solutions Inc. AMB received consultation fees from industry, including Pfizer and Lundbeck Canada. PR-N has ongoing scientific collaborations with NAVIDEA biopharmaceuticals (nonfinancial competing interests). The remaining authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Burhan, A.M., Bartha, R., Bocti, C. et al. Role of emerging neuroimaging modalities in patients with cognitive impairment: a review from the Canadian Consensus Conference on the Diagnosis and Treatment of Dementia 2012. Alz Res Therapy 5 (Suppl 1), S4 (2013). https://doi.org/10.1186/alzrt200
Published:
DOI: https://doi.org/10.1186/alzrt200