Abstract
Introduction
Solitary fibrous tumors of the central nervous system usually present as dura-based masses and clinically resemble meningiomas. There are very few reported cases of intra-ventricular solitary fibrous tumors, particularly in the fourth ventricle.
Case presentation
Our patient was a 52-year-old African-American man, who presented to our facility with a two-month history of progressive weakness and numbness in all extremities. A computed tomography scan and brain magnetic resonance imaging scan revealed a homogeneous, avidly enhancing 4.5 × 3.7 × 2.7cm fourth ventricular mass, with compression of adjacent medulla and cerebellum and extension into the foramen of Luschka. Our patient underwent a suboccipital craniotomy and resection of the tumor. A histological examination showed a spindle cell neoplasm with prominent collagenized stroma. The neoplastic cells were strongly and diffusely positive for CD34, vimentin and Bcl-2, and negative for S-100, CD99 and epithelial membrane antigen. The molecular immunology Borstel-1 (MIB-1) proliferation index was low (1%). CD31 immunostain highlighted the endothelial cells but the spindle cells were negative. Reticulin stain demonstrated a moderate reticulin network but individual cells were not invested by reticulin fibers. The histological features and immunoprofile was consistent with a solitary fibrous tumor.
Conclusions
In the central nervous system, solitary fibrous tumors are usually indolent tumors, with only rare examples showing hypercellularity and increased mitotic activity; features that were absent in our patient’s case. We present an uncommon central nervous system neoplasm in a rare location. Although uncommon, solitary fibrous tumors should be included in the differential diagnosis of intra-ventricular tumors in adults.
Similar content being viewed by others
Introduction
Solitary fibrous tumors (SFTs) were originally described in pleura and subsequently in soft tissue and many other organs including the central nervous system. SFTs of the central nervous system are rare entities, usually presenting as dura-based masses predominantly in the posterior fossa and spinal region [1]. SFTs are composed of spindle cells in a collagenized stroma with characteristic immunohistochemical features: diffuse and strong reactivity to CD34, positive for vimentin, and often immunoreactive to CD99 and Bcl-2 [1]. Intra-ventricular SFTs are rare, and only six cases have been reported in the fourth ventricle [2–7].
Case presentation
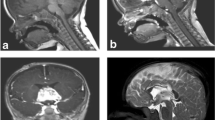
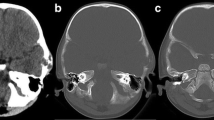
Our patient was a 52-year-old African-American man who presented to our facility with a two-month history of progressive weakness and numbness in all extremities. A computed tomography (CT) scan and a brain magnetic resonance imaging (MRI) scan revealed a 4.5 × 3.7 × 2.7cm, homogeneous, avidly enhancing mass located in the fourth ventricle, compressing adjacent medulla and cerebellum and extending into the foramen of Luschka (Figure 1). Angiography demonstrated multiple dysplastic-appearing branches from the right posterior inferior cerebellar artery supplying the neoplasm.
Our patient underwent a suboccipital craniotomy and resection of the tumor. During the operation, a cavitron ultrasonic surgical aspirator as well as bipolar cautery and suction were used to debulk the tumor, followed by a combination of RHOTON™ dissectors as well as microscissors to separate the tumor. The entire tumor was successfully removed.
Histological examination showed a spindle cell neoplasm with prominent collagenized stroma (Figure 2A). Mitotic figures were not readily found and the molecular immunology Borstel-1 (MIB-1) proliferation index was low (1%). Meningothelial whorls and psammoma bodies were absent. The neoplastic cells were strongly and diffusely positive for CD34 (Figure 2B), vimentin and Bcl-2 (Figure 3A); no immunoreactivity with S-100, CD99 and epithelial membrane antigen (EMA) was detected. A CD31 immunostain highlighted the endothelial cells but not the spindle tumor cells. A moderate reticulin network was demonstrated by reticulin staining, but individual cells were not invested by reticulin fibers (Figure 3B). The histological features and immunoprofile were consistent with SFT.
Our patient experienced no neurological deficit after surgery, and there were no signs of recurrence at one-year follow-up.
Discussion
Intraventricular tumors can have a wide spectrum of differential diagnosis based on radiological and histopathological features. A bland spindle cell tumor with collagenized stroma and avid contrast enhancement initially suggested a diagnosis of fibroblastic meningioma. However the immunoprofile of the neoplastic cells was typical of a solitary fibrous tumor (negative for EMA, strongly positive for CD34, vimentin and Bcl-2). In contrast, meningiomas are EMA positive and CD34 negative. Hemangiopericytomas can have histological overlap with solitary fibrous tumor, but CD34 and Bcl-2 staining is weak and patchy [8].
To the best of our knowledge, just 17 Intraventricular solitary fibrous tumors have been reported in the literature to date. Six of these tumors were located in the fourth ventricle [2–7], eight cases were in lateral ventricle location [1, 9–14], one tumor located in the third ventricle [15], one case occurred in the foramina of Monro [16] and one case was a recurrent SFT arising from the falx cerebri, extending to the bilateral lateral ventricles and the third ventricle [17]. The clinical and radiological features of these tumors are given in Table 1; the immunomorphological features are given in Table 2. The age of patients ranged from 11 to 75 years old, with the vast majority being over 40 years; there was no sex predominance. Based on the available data, all the tumors were less or equal to 5.0 cm in their greatest dimension. On MRI scans, the tumors are typically iso- to hypointense on T1-weighted images, and show intense and homogeneous enhancement after intravenous administration of gadolinium. Most of those SFTs had bland histological features except two tumors showed mild to marked pleomorphism [5, 11]. Intraventricular SFTs have an indolent clinical course and excellent prognosis after surgery; however, owing to the small number of cases and limited follow-up, more data is needed to better assess the biological behavior of these tumors and the long-term outcome after treatment.
Conclusions
We report a rare case of SFT in an unusual location. Though rare, SFTs should be considered in the histological differential diagnosis of intra-ventricular tumors particularly, spindle cell tumors with collagenized stroma, along with meningioma and schwannoma.
Consent
Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Tihan T, Viglione M, Rosenblum MK, Olivi A, Burger PC: Solitary fibrous tumors in the central nervous system. A clinicopathologic review of 18 cases and comparison to meningeal hemangiopericytomas. Arch Pathol Lab Med. 2003, 127: 432-439.
Clarençon F, Bonneville F, Sichez JP, Khalil I, Poirier J, Chiras J: Atypical location of a solitary fibrous tumor in the fourth ventricle. J Neuroradiol. 2006, 33: 279-280. 10.1016/S0150-9861(06)77281-9.
Cummings TJ, Burchette JL, McLendon RE: CD34 and dural fibroblasts: the relationship to solitary fibrous tumor and meningioma. Acta Neuropathol. 2001, 102: 349-354.
Gessi M, Lauretti L, Fernandez E, Lauriola L: Intraventricular solitary fibrous tumor: a rare location for a rare tumor. J Neurooncol. 2006, 80: 109-110. 10.1007/s11060-006-9154-9.
Kim KA, Gonzalez I, McComb JG, Giannotta SL: Unusual presentations of cerebral solitary fibrous tumors: report of four cases. Neurosurgery. 2004, 54: 1004-1009. 10.1227/01.NEU.0000115675.74366.87.
Montano N, Doglietto F, Lauriola L, Signorelli F, Pallini R: Solitary fibrous tumor of the IV ventricle. Br J Neurosurg. 2010, 24: 495-496. 10.3109/02688691003675226.
Sawauchi S, Arakawa H, Taya K, Terao T, Nakazaki H, Numoto RT, Yamaguchi Y, Hashimoto T, Yamaguchi Y, Abe T: Solitary fibrous tumor of the fourth ventricle: case report. No Shinkei Geka. 2003, 31: 551-555.
Perry A, Scheithauer BW, Nascimento AG: The imunophenotypic spectrum of meningeal hemangiopericytoma: A comparison with fibrous meningioma and solitary fibrous tumor of the meninges. Am J Surg Pathol. 1997, 21: 1354-1360. 10.1097/00000478-199711000-00010.
Clarençon F, Bonneville F, Chiras J, Kujas M, Cornu P: Cystic intraventricular solitary fibrous tumor. AJNR AM J Neuroradiol. 2007, 28: 1205-1206.
Liao QL, Lai RQ: Solitary fibrous tumor of right ventricle: report of a case. Zhonghua Bing Li Xue Za Zhi. 2009, 38: 710-711.
Mekni A, Kourda J, Hammouda KB, Tangour M, Kchir N, Zitouna M, Haouet S: Solitary fibrous tumor of the central nervous system: pathological study of eight cases and review of the literature. Pathology. 2009, 41: 649-654. 10.3109/00313020903071439.
Surendrababu NR, Chacko G, Daniel RT, Chacko AG: Solitary fibrous tumor of the lateral ventricle: CT appearances and pathologic correlation with follow-up. AJNR Am J Neuroradiol. 2006, 27: 2135-2136.
Vassal F, Manet R, Forest F, Camdessanche JP, Péoc’h M, Nuti C: Solitary fibrous tumors of the central nervous system: report of five cases with unusual clinicopathological and outcome patterns. Acta Neurochir (Wien). 2011, 153: 377-384. 10.1007/s00701-010-0866-4.
Wright DH, Naul LG, Hise JH, Bauserman SC: Intraventricular fibroma: MR and pathologic comparison. AJNR Am J Neuroradiol. 1993, 14: 491-492.
Koçak A, Cayli SR, Saraç K, Aydin NE: Intraventricular solitary fibrous tumor: an unusual tumor with radiological, ultrastructural, and immunohistochemical evaluation. Case report. Neurosurgery. 2004, 54: 213-217.
Kinfe TM, Tschan CA, Stan AC, Krauss JK: Solitary fibrous tumor of the foramen of Monro. Clin Neurol Neurosurg. 2008, 110: 404-407. 10.1016/j.clineuro.2007.12.015.
Teranishi K, Yamamoto T, Nakao Y, Osada H, Wada R, Mori K: Recurrent solitary fibrous tumor of the falx cerebri with intraventricular extension. Neurol Med Chir (Tokyo). 2007, 47: 269-272. 10.2176/nmc.47.269.
Acknowledgements
We acknowledge the cooperation of our patient, as well as our patient’s family. This paper was not funded by any external source.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CW performed the gross examination of the specimen, conceived the case report, searched the literature and drafted the manuscript. VM performed the histopathological evaluation of the slides and made substantial revisions to the manuscript. SF conducted the radiology examinations and made revisions to the manuscript. MW operated on our patient and made revisions to the manuscript. AM performed the histopathological evaluation of the slides and critical analyzed the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Wang, C., Manucha, V., Faro, S. et al. Fourth ventricular solitary fibrous tumor: a case report and review of the literature. J Med Case Reports 6, 205 (2012). https://doi.org/10.1186/1752-1947-6-205
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1947-6-205