Abstract
"Social autopsy" refers to an interview process aimed at identifying social, behavioral, and health systems contributors to maternal and child deaths. It is often combined with a verbal autopsy interview to establish the biological cause of death. Two complementary purposes of social autopsy include providing population-level data to health care programmers and policymakers to utilize in developing more effective strategies for delivering maternal and child health care technologies, and increasing awareness of maternal and child death as preventable problems in order to empower communities to participate and engage health programs to increase their responsiveness and accountability.
Through a comprehensive review of the literature, this paper examines the concept and development of social autopsy, focusing on the contributions of the Pathway Analysis format for child deaths and the Maternal and Perinatal Death Inquiry and Response program in India to social autopsy's success in meeting key objectives. The Pathway Analysis social autopsy format, based on the Pathway to Survival model designed to support the Integrated Management of Childhood Illness approach, was developed from 1995 to 2001 and has been utilized in studies in Asia, Africa, and Latin America. Adoption of the Pathway model has enriched the data gathered on care seeking for child illnesses and supported the development of demand- and supply-side interventions. The instrument has recently been updated to improve the assessment of neonatal deaths and is soon to be utilized in large-scale population-representative verbal/social autopsy studies in several African countries. Maternal death audit, starting with confidential inquiries into maternal deaths in Britain more than 50 years ago, is a long-accepted strategy for reducing maternal mortality. More recently, maternal social autopsy studies that supported health programming have been conducted in several developing countries. From 2005 to 2009, 10 high-mortality states in India conducted community-based maternal verbal/social autopsies with participatory data sharing with communities and health programs that resulted in the implementation of numerous data-driven maternal health interventions.
Social autopsy is a powerful tool with the demonstrated ability to raise awareness, provide evidence in the form of actionable data and increase motivation at all levels to take appropriate and effective actions. Further development of the methodology along with standardized instruments and supporting tools are needed to promote its wide-scale adoption and use.
Similar content being viewed by others
Introduction and background
In developing country settings with inadequate vital registration systems and where many deaths occur at home, verbal autopsy is the investigative method most often used to determine the prevailing biological causes of death. Health policymakers and programmers require these data to identify health priorities, allocate sparse resources, and evaluate the impact of health programs. Social autopsy consists of questions on modifiable social, cultural, and health system factors that contribute to the same deaths investigated by verbal autopsy. Because social autopsy studies are often conducted without a control group of survivors, it is important that the factors included be based on interventions of proven efficacy. Health care programmers and policymakers need these data to identify strategies for increasing health-promotive behaviors and access to and utilization of quality health care services. Two complementary purposes of social autopsy are to increase awareness of maternal and child mortality to empower communities to participate and to engage health programs to increase responsiveness and accountability; and to provide large-scale population-level data to support advocacy and securing of the necessary resources to tackle these problems.
Verbal autopsy instruments for child deaths have most often included only limited elements that could be termed "social autopsy," usually consisting of a few questions regarding whether and where care was sought for the fatal illness. In contrast, verbal autopsies for maternal deaths earlier on and more frequently have examined the social contributors to death alongside the medical causes. Factors influencing this approach include the success of the nationwide system of health facility-based confidential inquiry into maternal deaths conducted in the United Kingdom since 1952, which from the beginning recognized the importance of social factors and examined these by constructing illustrative vignettes of individual maternal deaths [1]; and later, the widespread adoption of the "Three Delays" model of maternal mortality [2], which highlights the social/behavioral causal chain linking the household, community, and health system and provides a clear framework for the development of maternal social autopsy tools. The World Health Organization (WHO) helped promote the spread of maternal death reviews using several methods, including verbal autopsy with a strong social element, with its Beyond the Numbers effort [3], which was highly influenced by the earlier work in Britain.
Similarly influenced by Mosley and Chen's 1984 framework for the study of child survival in developing countries, which posited a set of socioeconomic determinants underlying and operating through proximate biological factors to affect mortality [4], child survival strategies in the 1990s evolved in the same direction toward integrated approaches and an appreciation for the importance of household and community factors in health promotion, disease prevention, and treatment. This culminated in the development of the Pathway to Survival framework in 1995 [5]. In response, social autopsy efforts for fatally ill children emerged that holistically track the entire process and determinants of health care provision, care seeking (or not) from home to facility, and the quality of care provided.
The size and scope of the enhanced social autopsy efforts both for child and maternal deaths varied, but most were limited to studies at subdistrict, district, or country-region level. This was often appropriate, as important social factors may vary by site and many social autopsy studies were intended to support local health program implementation. But national level data, important for advocating and securing resources for community health approaches, as well as for developing regional and global estimates of social and behavioral determinants of health, were lacking. An anomaly emerged as well -- that, while the methodology grew from a programmatic approach that acknowledges the importance of community participation, few of the programs or researchers conducting social autopsies have sought participation below the level of health programmers and policymakers in sharing or utilizing the data for program or intervention development. However, a track did emerge among practitioners and external users of maternal death reviews, including those based on verbal autopsy, recognizing the power of the data to increase the visibility and awareness of the problem [6] and, in the process, to raise the demand for access to quality maternal health care as a human right [7]. In this way, social autopsy has made an important contribution to the political process and formation of health policy at the global, national, and subnational levels.
This paper undertakes a comprehensive review of the literature in order to examine the concept of social autopsy, the development of the methodology, and the quality of its execution in the pursuit of five key objectives. The analysis of study outcomes is organized around seminal efforts in which the authors have participated, while also assessing how widely and successfully the social autopsy method has been adopted.
Methods
Search strategy
We conducted computerized searches of Embase, PubMed, and SCOPUS databases using the keywords and phrases: (careseeking OR care-seeking OR care seeking) AND (death OR mortality), "social autopsy," and "verbal autopsy." We then manually searched references quoted in original publications for additional information.
Study inclusion and exclusion criteria
To be included in the review, studies had to fulfill the following criteria:
-
1.
Published after 1989 in a peer-reviewed journal or as a report accessible through a Web search;
-
2.
Examine the care-seeking process for fatal illnesses of children from birth to 5 years or for maternal deaths;
-
3.
Investigate a minimum of 50 child or maternal deaths;
-
4.
Include an abstract accessible through the search database; and
-
5.
Written in English or French.
Study characteristics
Standard information was abstracted from all eligible studies by two reviewers (AK and HDK). The information included the following: the dates the data were collected and published; the setting, i.e., the country and site in which the work was conducted; the group studied (maternal, child, or both); the number of deaths observed; the study objective and design; and the format (open-ended, closed-ended, or combined) and source of the social autopsy questionnaire.
Outcomes
Data were also extracted to assess whether the study met five key objectives of social autopsy, as follows: (i) essential elements of the care-seeking process were described, including recognition of the illness, whether adequate home care was provided, whether and what type of outside-the-home care was sought (informal, formal, or both), delays to formal health care seeking and related constraints (e.g., lack of knowledge of illness danger signs, seeking traditional care, lack of transportation, costs), and the quality of health care provided (from the client's perspective); (ii) a social diagnosis of the contributors to death was made, i.e., household (behavioral), community (social), and health system determinants of the deaths were identified; (iii) the study provided representative national or large area data; and the data were utilized to support (iv) health program or policy development; and/or (v) community empowerment.
Ethical considerations
The social autopsy studies conducted in Bolivia [8] and Guinea [9] that two of the authors participated in and that were central to the work described in this paper were programmatic efforts approved by the national and regional ministries of health (MOH) of the respective countries without undergoing formal ethical review. The Maternal and Perinatal Death Inquiry and Response (MAPEDIR) program in India [10], also central to this paper, was reviewed by the Johns Hopkins University institutional review board and found to be a programmatic effort, rather than research, and so was exempt from board oversight. Nevertheless, key Helsinki principles were upheld in the conduct of all these studies, including administering informed consent to all respondents and maintaining the confidentiality of the information they provided.
Results
The search of the databases using the keywords and phrases identified 14 articles and reports of child deaths and eight of maternal deaths that met the inclusion criteria (Table 1). Only three child studies were conducted prior to the development of the Pathway to Survival model in 1995, which positively influenced the scope of care-seeking factors considered by subsequent studies. Understanding the Pathway sets the context for examining the development of the social autopsy method.
Child social autopsy: providing evidence on failures in the Pathway to Survival
The multicountry assessment of WHO/UNICEF's Integrated Management of Childhood Illness (IMCI) approach found that, although IMCI health facilities provided the gold standard of child illness care in developing countries, the strategy failed to decrease child mortality. In part this was due to weak implementation of IMCI's family and community component, and assuming that quality health care services alone would lead to increased care seeking and appropriate home care practices [11]. Access, coverage, and utilization were all found to lag, resulting in ineffective delivery of appropriate child survival technologies.
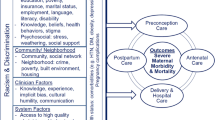
The Pathway to Survival conceptual framework (Figure 1) was designed to support the implementation and monitoring of IMCI, with the aim of highlighting the essential steps that need to be taken both inside the home and in the community to prevent child illness and return sick children to health. The pathway identifies and organizes modifiable social, cultural, and health system factors affecting home care practices, health care access and utilization, and the delivery of quality health care [12].
As seen in Table 1 (and Additional file 1, which provides more details), the three child social autopsy studies conducted prior to the development of the Pathway model [13–15], as well as the three non-Pathway studies conducted after the Pathway model was developed [16–18], examined, on average, three aspects of the care-seeking process. In contrast, the eight later studies that followed the Pathway model [8, 9, 19–24] on average assessed eight care-seeking elements, providing a more complete understanding of the care-seeking process and the factors affecting health care utilization for severely ill children in developing countries. Nevertheless, even the non-Pathway studies, with their limited set of data variables and none examining a representative sample of deaths at the district or higher level (two of the Pathway studies met this objective), attempted to form a social diagnosis of mortality determinants. More of the Pathway studies were also conducted by or in support of health programming or health policy development (5/8) and to support community participation and empowerment (4/8), compared, respectively, to 2/6 and 1/6 of the non-Pathway studies. Somewhat higher percentages of the Pathway than non-Pathway studies were also rated as strongly supporting health programs (3/8 versus 2/6) and communities (2/8 versus 1/6).
The first analysis of child deaths following the Pathway model was a survey conducted in 1995 of 271 child deaths from randomly selected census tracts over a then-recent nine-month period in El Alto, Bolivia [8]. The social autopsy format used in the Bolivia study, consisting of a separate sheet duplicating the same open-ended questions on possible problems along the pathway for each day of the illness, was found to be cumbersome both for data collection and analysis. Subsequent work produced a one-page social autopsy tool formatted as a matrix, with each row constituting one action taken for the illness, and columns for recording the action, the illness day the action was taken, the illness signs at the time the action was taken, reasons for the action being taken, and each of the remaining steps along the pathway. The Pathway Analysis social autopsy format was published online as part of a manual aimed at health programs describing how to undertake a child mortality study to determine the biological causes and social determinants of death [25]. Later work added a module for investigating perinatal deaths.
Subsequent social autopsy studies utilizing or based on this format and manual were conducted in Guatemala [19], Cambodia [21], and Guinea [9] with support from the group producing the materials, as well as by an independent group working in Uganda [24]. Figure 2 illustrates the type of information gathered by the social autopsy instrument with data from Guinea for 330 child deaths. It can be seen, for example, that while 290 (88%) of the children's caretakers recognized one or more signs of a severe illness, 34 (10%) of the children received no care whatsoever, 238 (72%) were taken for some outside-the-home care, on average 2.3 days after the illness began, and only 132 (40%) children received some formal health care, on average 3.5 days after the illness onset. The Guinea study identified only 13 referrals, perhaps because it used an early version of the social autopsy questionnaire that did not ask about this directly; a later refinement improved the assessment of referrals.
In 2009, the WHO/UNICEF-supported Child Health Epidemiology Reference Group (CHERG) [26] undertook to review and update the Pathway Analysis social autopsy format. The main issues considered were: 1) in response to the increased contribution of neonatal deaths to overall child mortality resulting from recent decreases in post-neonatal deaths [27], to improve the format's assessment of stillbirths and neonatal deaths and related care-seeking issues by adding modules on maternal and newborn care, including care seeking for maternal complications; 2) to strengthen the evaluation of child preventive care; 3) to examine a host of behavioral and social factors not previously considered; and 4) to include questions on the utilization of trained community health workers, in accord with the recent inclusion of these workers in some formal health systems. Most of the social, behavioral, and preventive factors that were added to the questionnaire (Table 2) were based on interventions included in the Lives Saved Tool [28], which undergo rigorous review for evidence of their efficacy. In addition, where possible, the questions were worded similarly to those in the Demographic and Health Surveys (DHS) [29] in order to facilitate comparisons of the social autopsy data with similar data for survivors in settings where a recent DHS was conducted.
CHERG integrated the updated social autopsy instrument with the Population Health Metrics Research Consortium verbal autopsy questionnaire, which is currently being extensively validated by studies described in other articles in this series of Population Health Metrics. While the updated Pathway Analysis format is considerably longer than the original version, CHERG is developing CAPI (computer-assisted personal interview) software for field-based data capture on a netbook or tablet computer with built-in consistency checks, automatic mapping of skip patterns, and correct question wording depending on who the respondent is and the child's age at death. This should significantly ease the interview process and increase the quality of the data. Software versions are being developed both for the integrated verbal/social autopsy (VASA) interview and for the social autopsy alone to enable using it with other verbal autopsy instruments. These tools will be available open access on the CHERG website in order to facilitate their widespread use.
The largest scale of the prior Pathway Analysis studies was at the provincial level. One last objective that CHERG is working to fulfill is to collaborate with government and international partners in several countries in Africa to develop national and other large-scale VASA studies. The purpose is to provide evidence of modifiable social, cultural, and health systems factors contributing to neonatal and child mortality for advocacy and health policy and planning exercises and to begin gathering the data needed to develop global estimates of these factors.
Maternal death inquiry and response
Maternal death audit has been undertaken in many forms, including clinical audit, which evaluates the quality of care provided in health facilities against an accepted standard; confidential inquiry of all or a sample of deaths in a population, most often focusing on medical factors but sometimes including community aspects; facility-based maternal death review, preferably augmented with information from the community; and community-based VASA, most useful in areas where many deaths occur outside of a health facility, and which can be combined with a facility review of cases that did access care for a more accurate assessment of medical factors.
From its beginnings with Great Britain's nationwide system of confidential inquiry into maternal deaths, to its promotion by WHO's Beyond the Numbers effort and beyond, several developing countries have implemented a system of maternal death audit. Examples include Sri Lanka [30] and Malaysia [31], which review both hospital and home deaths, and South Africa [32], which conducts confidential inquiries of hospital deaths. The most recent large-scale effort has been the MAPEDIR program undertaken in 10 high-mortality states of India with assistance from UNICEF [10]. Because up to half or more of maternal deaths in these states are thought to go unreported, and many of these are thought to occur at home, it was decided to initiate MAPEDIR with community-based VASA of maternal deaths. In 2010, this effort culminated in the Government of India announcing its plan to commence a nationwide program of facility- and community-based maternal death audits [33].
The rationale for maternal social autopsy is the same as for child deaths. There are several highly efficacious interventions against maternal mortality, including, for example, antibiotics for preterm premature rupture of the membranes to prevent maternal (and fetal) sepsis, a skilled birth attendant providing active management of the third stage of labor to prevent postpartum hemorrhage, and treatment of primary postpartum hemorrhage with rectal misoprostol. Yet, as illustrated by the findings of 800 VASA interviews in Orissa, India (Figure 3), many women in developing countries may die at home without ever seeking health care for their maternal complications, and many who do seek care never receive effective treatment. As in the India context, this may often be true despite the fact that multiple facilities at a level that should be capable of providing basic or comprehensive emergency obstetric care are visited during the fatal illness. To effectively tackle these problems, data are needed on the social, behavioral, and health system factors contributing to the deaths. And effective sharing of such data, in a setting where in its absence many of the deaths would not have even been registered much less investigated, can raise awareness of the magnitude, causes, and determinants of the problem and support the development of effective interventions with communities and health programs. Where programs and government are less responsive, the data can be used for advocacy to promote accountability.
Of the seven non-MAPEDIR studies included in the comprehensive review of maternal social autopsy, five strongly supported health programs and three provided some support to community participation and empowerment (Table 1). Two of the studies were either conducted or commissioned by the country's national maternal health program and their findings were used to help guide the country's reproductive health strategy [34, 35]. In such cases, it is evident that responsive programs are in place and making good use of the social autopsy data. Two additional papers included an author from the government health authority [36, 37], suggesting that practical use might also be made of their findings; one of these stressed the importance of disseminating the findings to policymakers, health planners, health professionals, and the community to ensure sensitization and action and recommended implementation of community- and hospital-based maternal death audits [37]. One other paper described the use of the social autopsy data in a participatory audit system consisting of periodic meetings of community and district health staff, with the audits of some deaths also involving community representatives [38]. The two remaining papers proposed health system or community interventions based on their study findings, but took the process no further [39, 40]. Similar to the child studies, all but one of these maternal studies made a social diagnosis of mortality determinants, although only two collected data on a representative sample of deaths from a district or larger area.
The eighth maternal study reviewed, the MAPEDIR program, collected data on a similar number of care-seeking variables (6) as the other seven studies (mean = 4.9), but was unique in its extensive sharing, interpretation, and use of the data for health planning and intervention development by the community, as well as health authorities and government officials (Additional file 1) [10]. The first level of data provided by MAPEDIR was a simple but powerful one in raising awareness and the visibility of the problem. MAPEDIR increased the reporting of maternal deaths by the community and local health providers, most highly in locales where reporting had previously lagged far behind. It accomplished this by first engaging health officials, talking about the problem, and highlighting the reluctance of first-line health workers to report maternal deaths for fear of being blamed and penalized. The importance of a nonblaming approach and a search for systemic causes for the deaths was discussed. Similar sensitization sessions were held with villagers as part of discussions on the need for birth preparedness, complication readiness, and reporting and investigating maternal deaths to discover what went wrong. Data from the resulting death inquiries were sometimes disturbing to health officials and spurred them to take action. For example, in several states it was found that a disproportionate share of maternal deaths occurred among women of lower castes. Data from the inquiries shared with communities empowered them to understand how future deaths could be prevented and to develop appropriate interventions. Table 3 lists some of the many interventions developed at multiple levels as part of the MAPEDIR response.
Discussion
Meeting the social autopsy objectives
The comprehensive review of the English and French literature found that adoption of the Pathway to Survival framework, starting with Aguilar et al's 1998 study in Bolivia [8], increased the richness of the data on the care-seeking process collected by child social autopsy. The Pathway studies provided valuable information and an increased understanding of the social, behavioral, and health systems factors affecting care seeking for severe neonatal and child illnesses in developing countries. Thus, while many of the non-Pathway studies made a social diagnosis of mortality determinants, it is likely that the Pathway studies were able to reach a more accurate diagnosis. The Pathway studies also were used somewhat more often to support health programs and communities, but even they fell short of fully achieving this objective -- fewer than half were rated as strongly supportive of health programs and only one-quarter were strongly supportive of communities.
The reviewed maternal social autopsy studies collected data on a range of care-seeking variables, with the MAPEDIR program ranking somewhat above average in the number of factors examined, perhaps enhancing its ability to reach an accurate social diagnosis of mortality determinants. However, while most of the maternal studies strongly supported health programs, only the MAPEDIR program also offered strong support to communities. Recent evidence suggests that this is more than a philosophical choice, that community participation and empowerment can strongly impact neonatal and perhaps maternal mortality [41].
Social autopsy serves varied purposes; among these are providing large-scale population-level data to contribute to country and global estimates of mortality determinants, and increasing awareness of maternal and child death as preventable problems in order to empower communities and engage health programs. While most of the reviewed studies did not meet the objective of selecting a representative sample of deaths at the district or larger area level, and so may not be generalizable to overall mortality in the study areas and thereby serve the first listed purpose of social autopsy, nonetheless several were found to strongly support health programs and communities in improving health interventions and access to care. However, this does not negate the importance of selecting cases in as representative a fashion as possible, within existing limitations. For example, if it is known that many deaths in the service area are occurring at home, then a social autopsy investigation should be designed to ensure that home deaths are included in the study sample.
The relationship of social autopsy to death audit
The term "social autopsy" implies that a social diagnosis is to be made of the most common or otherwise important social, behavioral, and health systems determinants of mortality. While data on social factors can play a role in audits of individual deaths, as in facility-based death reviews that include interviews of the deceased's family members, the term as used in this review refers to aggregate diagnoses made using quantitative data. Social autopsy can also provide qualitative data in the form of individual illness narratives, with the purpose of illustrating the overall care-seeking process, showing how several problems can conspire to cause a death, and putting a human face on the numbers. Sharing and discussion of these narratives, especially at the community level, provides a powerful learning opportunity, but the process must take care to preserve confidentiality and foster a nonblaming approach. Otherwise, there is the danger that the sharing session could deteriorate into a negative atmosphere, diverting attention from the necessary focus on systemic problems that can be fixed through collective action and discouraging community participation.
Supratikto et al. conducted community-based audits of local, individual maternal deaths, and discussed the challenge of preserving confidentiality and nonblaming in this setting [38]. In their research study of three different approaches to village-based audit of neonatal deaths, Patel et al. did not face this problem, though they observed that the bereaved family's presence at the audit could decrease participants' willingness to discuss the case, and cautioned that in other settings scrutinizing individual cases might adversely affect family and community relations [42]. The MAPEDIR program's approach to maintaining confidentiality while utilizing illness narratives was to share composite vignettes of cases illustrating common problems or actual cases from across borders so the participants would be unlikely to know the family of the case being discussed. In the end, the discussion would be brought back to the quantitative data to help prioritize problems illustrated by the individual stories within the context of the community's overall experience.
Limitations
Just as in the sharing of social autopsy data with the community, care must be taken in collecting and handling the data to ensure confidentiality of the highest possible level and the respondent's comfort with providing the information. There is potential for the information to be stigmatizing, for example, if the respondent or another family member delayed taking an action perceived as possibly life-saving. This could affect the respondent's openness during the interview and the accuracy of the illness reports. Limited recall for remote events is another potential problem, as sample size needs for child social autopsy may require interviewing families with a child death three or more years ago. This issue will be more exacerbated in a study of maternal deaths.
Technical issues
As with verbal autopsy, some challenges remain for social autopsy, both to improve its ease of use and assess the validity of the information it gathers. Item reduction might be possible, both in terms of the number of questions asked and the number of potential responses to multiple-choice questions. This would shorten the duration of the interview and simplify the questions, making it more practical to conduct social autopsy on the platform of national surveys and in the context of local health program planning and monitoring. An integrated VASA interview can take 60 to 90 minutes to complete, and some have argued that the interviews should therefore be separated. Counterarguments are that respondents would rather not undergo a second visit; that a return visit would be even more impractical on the platform of a national survey; that elements of the verbal autopsy, such as the illness signs and symptoms, must in any case be discussed as part of the social autopsy care-seeking questions; and that by following a more natural chronology an integrated interview promotes an improved interviewer-respondent dialogue and enhances recall of the illness events. The new CAPI software also promises to ease the interview process and shorten its duration.
Another argument in favor of separating the verbal and social autopsies is that this might help overcome the potential for the stigma of the social autopsy discussed above to affect disclosure of verbal autopsy information and hence determination of the biological diagnoses. This separation could also foster a specialized approach to social autopsy, enabling a more elaborate informed consent process and a dedicated cadre of interviewers trained to more effectively deal with feelings of anger, guilt, and shame over the death that might arise during the interview. Determining which of the implementation models works best will require additional experience and possibly experimentation.
Social autopsy analysis at its most basic level involves outputting frequency distributions of all the questionnaire's mortality determinants. However, many important questions can be answered only by cross tabulations, such as who the decision-makers were for facility and home delivery, and for which illness signs and symptoms particular actions were taken. Comparisons can also be made of women or children for whom care was and was not sought. This can enhance the identification of care-seeking constraining factors. Such analyses might also help with item reduction by identifying noninformative variables, and potentially expose needed areas of inquiry not covered by the questionnaire.
While there is a history of validating verbal autopsy, only one study included in the comprehensive review validated any aspect of the social autopsy. Bojalil et al. independently assessed the clinical competence of doctors mentioned in mothers' narratives of their child's fatal illness and found a high correlation between the quality of care they provided as assessed from the narratives and by the competence scores [23]. Jafarey et al. attempted to use medical records to validate third delays identified in narrative accounts of care received for maternal complications at tertiary facilities, but were not able to due to inadequate information in the medical records [37]. In addition to the quality of medical care received, other aspects of social autopsy to consider for validation include caregivers' reports of care sought or other actions taken, and care-seeking delays and constraining factors.
The way forward
It is apparent that the Pathway to Survival and Three Delays models are useful for organizing the care-seeking process for severe child and maternal illnesses. Future social autopsy studies should be guided by these models, and should also make use of social autopsy's other strengths of raising awareness through participatory data sharing and intervention development. Just as there have been international efforts to standardize verbal autopsy instruments and analytic methods for neonatal, child, and adult deaths, the utility and acceptability of social autopsy findings could be advanced by reaching agreement on a core dataset to be gathered and on standardized formats and methods for accomplishing this. CHERG's Pathway Analysis format has the advantage of having been reviewed and updated by scientists from several international organizations, including WHO, but the team was small, the instrument has not been officially endorsed, and there are other groups working to develop their own social autopsy instrument for child deaths, the most prominent being the INDEPTH Network. A process is needed to bring together interested parties, finalize these efforts, and reach agreement on a standardized format and data analysis plan.
Similarly, a standardized social autopsy format and analysis plan for maternal deaths is needed. WHO published suggested questions for maternal verbal autopsy, including questions on care seeking [43], that at least two of the papers in the present review used as the basis for their study instruments. UNICEF's MAPEDIR program developed a standardized VASA format for investigating maternal deaths as well as accompanying materials for training surveyors and sharing the findings with the community, but has not yet published these resources.
Developing standardized questionnaires and analysis plans for child and maternal deaths could promote the agenda of routinely collecting and utilizing quality social autopsy data. These instruments should be provided together with tools for country adaptation, fieldworker training, and community data sharing. These efforts will be enhanced by further work to develop the social autopsy method, such as identifying ways to minimize the stigmatizing effect of certain questions and assessing the optimal model for combining or sequencing the verbal and social autopsy interviews.
Conclusions
Social autopsy is a powerful tool for raising awareness and the visibility of child and maternal death as preventable problems in the community, among health workers, health authorities, and government officials. It provides evidence in the form of actionable data to communities, health programs, and health policymakers, and increases motivation at all levels to take appropriate and effective actions. Health systems and communities of implementing countries, individually and as partners, used the Pathway to Survival and MAPEDIR findings to develop appropriately focused interventions. Additional social autopsy studies reviewed for this paper were utilized by governments to improve health programming. Social autopsy data can also build institutional awareness and political commitment, thus helping to increase health system and governmental accountability and responsiveness. Community participation in the death inquiry and response process may in itself act as an intervention by increasing awareness and motivating communities to take action in a way that increases care seeking. Social autopsy studies conducted in representative, large-scale populations can provide data to develop national and global estimates of social, cultural, and health systems determinants of mortality and to advocate for the resources needed to overcome these problems. New neonatal and child VASA studies are being planned at the country or subnational level in several African countries. Further development of the social autopsy method and development and wide-scale adoption of standardized tools based on the Pathway to Survival and Three Delays models will promote social autopsy's overall objectives of providing evidence on failures in the pathway to survival and increasing awareness to empower communities and engage health programs in the battle against child and maternal mortality.
References
Why Mothers Die 2000-2002: The Sixth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. 2011, accessed 8 March.
Thaddeus S, Maine D: Too far to walk: maternal mortality in context. Social Science & Medicine 1994, 38: 1091-1110. 10.1016/0277-9536(94)90226-7
Beyond the Numbers: reviewing maternal deaths and complications to make pregnancy saferWorld Health Organization, Geneva; 2004, accessed 14 July 2011. [http://www.who.int/making_pregnancy_safer/documents/9241591838/en/index.html]
Mosley WH, Chen LC: An analytic framework for the study of child survival in developing countries. Popul Dev Rev 1984,10(Suppl):25-45.
Claeson M, Waldman RJ: The evolution of child health programmes in developing countries: from targeting diseases to targeting people. Bull World Health Organ 2000, 78: 1234-1255.
De Brouwere V, Tonglet R, Van Lerberghe W: Strategies for reducing maternal mortality in developing countries: what can we learn from the history of the industrialized West? Trop Med Internat Health 1998, 3: 771-782. 10.1046/j.1365-3156.1998.00310.x
Hunt P:Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of health. United Nations General Assembly; 2010, accessed 14 July 2011 A/HRC/14/20/Add.2. [http://www.unhcr.org/refworld/country,,,FACTFINDING,IND,,4c0367cf2,0.html]
Aguilar AM, Alvarado R, Cordero D, Kelly P, Zamora A, Salgado R:Mortality Survey in Bolivia: The Final Report. Investigating and Identifying the Causes of Death for Children Under Five. The Basic Support for Institutionalizing Child Survival (BASICS) Project. Arlington, VA; 1998, accessed 14 July 2011. [http://pdf.usaid.gov/pdf_docs/PNACF082.pdf]
Schumacher R, Swedberg E, Diallo MO, Keita DR, Kalter HD, Pasha O:Mortality study in Guinea: Investigating the causes of death for children under 5. The Basic Support for Institutionalizing Child Survival Project (BASICS II). Arlington, VA; 2002, accessed 14 July 2011. [http://www.basics.org/documents/pdf/guinea_mort.pdf]
Maternal and Perinatal Death Inquiry and Response: Empowering communities to avert maternal deaths in India. UNICEF, New Delhi; 2008, accessed 8 March 2011. [http://www.unicef.org/india/MAPEDIR-Maternal_and_Perinatal_Death_Inquiry_and_Response-India.pdf]
Bryce J, Victora CG, Habicht JP, Black RE, Scherpbier RW, the MCE-IMCI technical advisors: Programmatic pathways to child survival: results of a multi-country evaluation of Integrated Management of Childhood Illness. Health Policy Plan 2005,20(suppl 1):15-17.
Waldman R, Campbell CC, Steketee RW:Overcoming remaining barriers: the pathway to survival. Current issues in child survival series, The Basic Support for Institutionalizing Child Survival (BASICS) Project. Arlington, VA; 1996, accessed 14 July 2011. [http://pdf.usaid.gov/pdf_docs/PNABZ644.pdf]
Sustrisna B, Reingold A, Kresno S, Harrison G, Utomo B: Care-seeking for fatal illnesses in young children in Indramayu, West Java, Indonesia. Lancet 1993, 342: 787-780. 10.1016/0140-6736(93)91545-W
Gutiérrez G, Reyes H, Martinez H, Tomé P, Guiscafré H: Study of the disease-health seeking-death process: another use of the verbal autopsy. International Journal of Epidemiology 1994, 23: 427-428. 10.1093/ije/23.2.427
Sodemann M, Jakobsen MS, Molbak K, Alvarenga IC Jr, Aaby P: High mortality despite good care-seeking behavior: a community study of childhood deaths in Guinea-Bissau. Bull World Health Organ 1997, 75: 205-212.
Hinderaker SG, Olsen BE, Bergsjo PB, Gasheka P, Lie RT, Havnen J, Kvale G: Avoidable stillbirths and neonatal deaths in rural Tanzania. BJOG 2003, 110: 616-623. 10.1046/j.1471-0528.2003.02153.x
de Savigny D, Mayombana C, Mwageni E, Masanja H, Minhaj A, Mkilindi Y, Mbuya C, Kasale H, Reid G: Care-seeking patterns for fatal malaria in Tanzania. Malaria Journal 2004, 3: 27. 10.1186/1475-2875-3-27
Beiersmann C, Sanou A, Wladarsch E, De Allegri M, Kouyaté B, Müller O: Malaria in rural Burkina Faso: local illness concepts, patterns, traditional treatment and influence on health-seeking behaviour. Malaria Journal 2007, 6: 106. 10.1186/1475-2875-6-106
de Bocaletti E, Schumacher R, Hurtado E, Bailey P, Matute J, McDermott J, Moore J, Kalter HD, Salgado R:Perinatal mortality in Guatemala: Community study. MotherCare; 1999, accessed 14 July 2011. [http://pdf.usaid.gov/pdf_docs/PNACJ798.pdf]
Terra de Souza AC, Peterson KE, Andrade FMO, Gardner J, Ascherio A: Circumstances of post-neonatal deaths in Ceara, Northeast Brazil; mother's health care-seeking behaviors during their infant's fatal illness. Social Science & Medicine 2000, 51: 1675-1693. 10.1016/S0277-9536(00)00100-3
The Pathway to child health (Siem Reap, Pursat, Stung Treng, and Kampot). The Reproductive and Child Health Alliance (RACHA); accessed 14 July 2011, 2000. [http://rc.racha.org.kh/docDetails.asp?resourceID=32&categoryID=3]
Bandari N, Bahl R, Taneja S, Martines J, Bhan M: Pathways to infant mortality in urban slums of Delhi, India: implications for improving the quality of community- and hospital-based programmes. J Health Popul Nutr 2002, 20: 148-155.
Bojalil R, Kirkwood BR, Bobak M, Guiscafre H: The relative contribution of case management and inadequate care-seeking behaviour to childhood deaths from diarrhea and acute respiratory infections in Hidalgo, Mexico. Trop Med and International Health 2007, 12: 1545-1552. 10.1111/j.1365-3156.2007.01963.x
Waiswa P, Källander K, Peterson S, Tomson G, Pariyo GW: Using the three delays model to understand why newborn babies die in eastern Uganda. Trop Medicine and International Health 2010, 15: 964-972. 10.1111/j.1365-3156.2010.02557.x
Kalter HD, Salgado R, Gittelsohn J, Parades P:A Guide to Conducting Mortality Surveys and Surveillance. The Basic Support for Institutionalizing Child Survival Project (BASICS II). Arlington, VA; 2004, accessed 22 June 2011. [http://www.jsi.com/JSIInternet/Resources/Publications/childsurvival.cfm]
Child Health Epidemiology Reference Groupaccessed 8 March 2011. [http://cherg.org/main.html]
Lawn JE, Cousens S, Zupan J, for the Lancet Neonatal Survival Steering Team: 4 million neonatal deaths: When? Where? Why? Lancet 2005, 365: 891-900. 10.1016/S0140-6736(05)71048-5
Boschi-Pinto C, Young M, Black RE: The child health epidemiology reference group reviews of the effectiveness of interventions to reduce maternal, neonatal and child mortality. International J Epidemiol 2010, 39: i3-i6. 10.1093/ije/dyq018
Fisher AA, Way AA: The demographic and health surveys program: An overview. International Family Planning Perspectives 1988, 14: 15-19. 10.2307/2947652
Perera MALR: High maternal mortality and morbidity: the shame of the South-East Asia region. Regional Health Forum WHO South-East Asia Region 2006, accessed 21 March 2011.,6(2): [http://www.searo.who.int/en/Section1243/Section1310/Section1343/Section1344/Section1356_5336.htm]
Suleiman AB, Mathews A, Jegasothy R, Ali R, Kandiah N: A strategy for reducing maternal mortality. Bull World Health Organ 1999, 77: 190-3.
Saving Mothers 2005-2007: Fourth Report on Confidential Enquiries into Maternal Deaths in South Africa; Expanded Executive Summary. National Committee on Confidential Enquiries into Maternal Deaths; 2008, accessed 21 March 2011. [http://www.doh.gov.za/docs/reports/2007/savingmothers.pdf]
iGovernment: India announces audit of maternal deaths.accessed 8 March 2011. [http://igovernment.in/site/india-announces-audit-maternal-deaths-38295]
Bartlett LA, Mawji S, Whitehead S, Crouse C, Dalil S, Lonete D, Salama P, the Afghan Maternal Mortality Study Team: Where giving birth is a forecast of death: maternal mortality in four districts of Afghanistan, 1999-2002. Lancet 2005, 365: 864-870. 10.1016/S0140-6736(05)71044-8
Campbell O, Gipson R, Issa AH, Matta N, El Deeb B, El Mohandes A, Alwen A, Mansour E: National maternal mortality ratio in Egypt halved between 1992-93 and 2000. Bull World Health Organ 2005, 83: 462-471.
Castro R, Campero L, Hernández B, Langer A: A study on maternal mortality in Mexico through a qualitative approach. J of Women's Health & Gender-Based Medicine 2000, 9: 679-690. 10.1089/15246090050118206
Jafarey SN, Rizvi T, Koblinsky M, Kureshy N: Verbal autopsy of maternal deaths in two districts of Pakistan--filling information gaps. J Health Popul Nutri 2009, 27: 170-183.
Supratikto G, Wirth ME, Achadi E, Cohen S, Ronsmans C: A district-based audit of the causes and circumstances of maternal deaths in South Kalimantan, Indonesia. Bull World Health Organ 2002, 80: 228-234.
Fawcus S, Mbizvo M, Lindmark G, Nystrőm L: A community-based investigation of avoidable factors for maternal mortality in Zimbabwe. Studies in Family Planning 1996, 27: 319-327. 10.2307/2138027
D'Ambruoso L, Byass P, Qomariyah N, Quedraogo M: A lost cause? Extending verbal autopsy to investigate biomedical and socio-cultural causes of maternal death in Burkina Faso and Indonesia. Social Science & Medicine 2010, 71: 1728-1738. 10.1016/j.socscimed.2010.05.023
Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, Tamang S, Thapa S, Shrestha D, Thapa B, Shrestha JR, Wade A, Borghi J, Standing H, Manandhar M, Costello AM, de L, members of the MIRA Makwanpur trial team: Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster-randomized controlled trial. Lancet 2004, 364: 970-79. 10.1016/S0140-6736(04)17021-9
Patel Z, Kumar V, Singh P, Singh V, Yadav R, Baqui AH, Santosham M, Awasthi S, Singh JV, Darmstadt GL: Feasibility of community neonatal death audits in rural Uttar Pradesh, India. Journal of Perinatology 2007, 27: 556-64. 10.1038/sj.jp.7211788
Campbell O, Ronsmans C: Verbal autopsies for maternal deaths, report of a WHO workshop, London 10-13 January 1994. World Health Organization, Geneva; (WHO/FHE/MSM/95.15); 1995.
Acknowledgements and funding
The authors thank Save the Children for permission to present the data in Figure 2, which were collected by Save the Children in Guinea, and Eric Swedberg of Save the Children for his leadership in conducting the Pathway Analysis study at the Guinea project site. We also acknowledge the contributions of dozens of NGO project staff and health workers in Bolivia, Guinea, and India to the social autopsy studies that we participated in and led in those countries; and of the many Government of India MOHFW officials and health workers and UNICEF health officers and fieldworkers who helped bring the MAPEDIR program to life in order to overcome death. Most of all, we acknowledge the contributions of the thousands of family members of deceased children and women who gave of their time and energy to participate in the verbal/social autopsy inquiries of the deaths of their loved one, to increase our understanding so that we might increase theirs.
Support for the Bolivia and Guinea VASA studies as well as for development of the Pathway Analysis format was provided by the United States Agency for International Development through The BASICS Project. Support for updating the Pathway Analysis questionnaire and conducting integrated VASA studies in sub-Saharan Africa was provided by the Child Health Epidemiology Reference Group through a grant from the Bill & Melinda Gates Foundation to the US Fund for UNICEF. The conceptualization, piloting and scaling up of MAPEDIR were funded by UNICEF as part of the UNICEF-assisted Country Programme in India.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
HDK co-led the team that developed the Pathway Analysis questionnaire, led the teams that updated this instrument and developed the MAPEDIR questionnaire, participated in the design and conduct of the Pathway Analysis study in Guinea and the MAPEDIR program in India, drafted the manuscript, and co-conducted the comprehensive review of social autopsy studies. RS participated in the design and conduct of the Bolivia Pathway Analysis study, co-led the team that developed the Pathway Analysis questionnaire, and was a member of the team that updated the instrument. MB conceived of the MAPEDIR program in India and led UNICEF monitoring and technical assistance to the government. AK helped draft the methods section of the manuscript and co-conducted the comprehensive review of social autopsy studies. REB conceived of updating the Pathway Analysis questionnaire. All authors critically reviewed and approved the final manuscript.
Electronic supplementary material
12963_2011_167_MOESM1_ESM.XLS
Additional file 1:Studies and reports meeting the inclusion criteria of the comprehensive review (with detailed findings). CS: care seeking; SA: social autopsy; HH: household; ARI: acute respiratory infection; MOH: ministry of health; PHC: primary health care; AD: acute diarrhea; VA: verbal autopsy; DSS: demographic and surveillance site; PtoS: Pathway to Survival; SB: stillbirth; DHS: Demographic and Health Survey; CHW: community health worker; VHC: village health committee; ANC: antenatal care; IMCI: Integrated Management of Childhood Illness; MOHP: ministry of health and planning; GOWB: Government of West Bengal; NGO: non-governmental organization; PRI: panchayat raj institutions; Δ and □: studies ranked, respectively, as providing "any" and "strong" support to health programs and communities. (XLS 62 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kalter, H.D., Salgado, R., Babille, M. et al. Social autopsy for maternal and child deaths: a comprehensive literature review to examine the concept and the development of the method. Popul Health Metrics 9, 45 (2011). https://doi.org/10.1186/1478-7954-9-45
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1478-7954-9-45