Abstract
Background
Recent qualitative research has shown that stiffness is an important symptom for patients to identify remission. However, it is unclear how to measure stiffness in low disease activity. This systematic review aims to summarise the existing literature on validity of patient reported outcomes to measure stiffness in RA low disease activity states, to aid the choice for a measurement instrument.
Methods
An extensive pubmed-search was undertaken, identifying measurement instruments for patient perceived stiffness used in low disease activity. Eligible studies reported on 1) stiffness as an outcome in relation to other core set measures, 2) development of a patient reported tool to measure stiffness, or 3) comparison of two different tools to measure aspects of stiffness, all in low disease activity.
Results
Of 788 titles, only two studies report on validity of stiffness measures within low disease activity. Morning stiffness (MS) is reported in 44 to 80% of patients in low disease activity. A difference of 40 to 60 minutes in duration until maximum improvement is observed between active and inactive patients. Severity of MS might discriminate better between high and low disease activity compared to measurement of duration of MS.
Conclusions
There is insufficient data on measurement of stiffness in the spectrum of low disease activity or remission.
Similar content being viewed by others
Background
Patients with rheumatoid arthritis (RA) often experience stiffness of joints, especially in the morning or after prolonged rest. Morning stiffness (MS) in RA can be attributed to the disrupted circadian rhythm of pro-inflammatory cytokine release in RA [1]. As a consequence, symptoms that follow the circadian rhythm like joint stiffness and pain are most severe in the early mornings [2].
Duration of MS was part of the American classification criteria for RA [3]. However, it was excluded from the recent update, as it was felt the instruments to measure it yielded data of insufficient reliability to include stiffness in the classification criteria [4–9]. Still, impaired morning function as a result of MS has considerable impact on the patients’ life. Severe stiffness in RA has been identified as the most important predictor of early retirement, apart from baseline working status [10]. A qualitative study showed significant impact of impaired morning function on quality of life, resulting in frustration and distress [11]. In addition, a strong inverse correlation between age and MS has been identified, with younger patients assessing their disease as more severe [12], pointing towards a higher burden of MS for younger patients compared to elderly patients. A qualitative study by Lineker et al. developed a patient-centered definition of MS in RA: 'slowness or difficulty moving the joints when getting out of bed or after staying in one position too long, which involves both sides of the body and gets better with movement’ [13].
Clearly, stiffness, either in the morning or during the day, is an important aspect of RA disease activity.
However, not much is known about the role of stiffness in low disease activity or remission. MS was part of the original ACR remission criteria [14], but is not a component of the new remission criteria for RA [15]. However, a recent qualitative study into the patients’ perspective on remission in RA showed that stiffness is an important aspect of the disease that needs to be reduced before one would feel to be in remission [16].
To investigate stiffness in low disease activity states, a valid measurement instrument is required. Cutolo recently published a bibliographic study of current assessment of morning stiffness, pain and function in RA [17]. Whilst a good overview of the current assessment and reporting of stiffness, this study did not report on performance of instruments in low disease activity.
With the current systematic review, we aim to summarise the existing literature on validity of patient reported outcomes to measure stiffness in RA low disease activity or remission, to aid the choice for a measurement instrument.
Methods
An extensive literature search identified existing, feasible measurement instruments or subscales of existing instruments for patient perceived stiffness, developed or used within RA research. Identified studies were manually reviewed for evidence on performance of instruments in low disease activity states.
Search strategy
We conducted a systematic literature search of Pubmed on 20-11-2012 to identify studies presenting patient reported measurement instruments that assess stiffness. No limitations for language or year of publication were used. The search was composed of three groups of search terms. The first group described the construct to be measured, ie stiffness. The second group described the disease, ie rheumatoid arthritis; the third group described the type of instrument, ie patient reported measurement instrument. These three groups were combined with a sensitive, validated filter that was specifically designed to identify studies on measurement properties in PubMed [18]. Finally, an exclusion filter was added, to remove non-relevant studies such as case reports, letters etc. The search strategy was composed by one author (LvT) in consultation with a medical information specialist (Table 1). See Additional file 1 for the detailed search strategy.
Selection process and inclusion criteria
The selection of abstracts and full-text articles was done in four phases; first, one author (LvT) screened all titles and abstracts and selected titles that reported on either stiffness or function, on measurement of patient reported outcomes (PRO) or the development or validation of PRO instruments. Secondly, two authors (LvT and MB) independently from each other evaluated the remaining abstracts of the possibly relevant studies by specifically selecting on populations with RA and reporting of measurement properties of stiffness.
Thirdly, potentially relevant full articles were retrieved and independently evaluated by the above authors. Articles were selected when they reported on stiffness in one of the following ways:
-
1.
stiffness as an outcome in relation to other core set disease activity measures
-
2.
the development of a patient reported tool to measure stiffness
-
3.
a comparison of two or more different tools to measure aspects of stiffness
The references of all studies included in the third phase, as well as reviews on measures of stiffness were checked for eligible studies.
Finally, the remaining articles, all reporting on aspects of validity of stiffness measures, were searched for information on performance in low disease activity or remission states by one author (LvT). See flowchart in Figure 1.
Data was extracted and summarised by one author (LvT) and reviewed by a second author (MB).
Results
Of 788 titles, only 2 studies provide data on stiffness in low disease activity and are included in this review. Measurements are restricted to stiffness in the morning and include measures of duration (both studies) and severity (one study). Another 14 studies examined validity of stiffness as a PRO in RA disease activity in general (Additional file 2) [6, 10, 19–30]. The two studies in low disease activity included in this review are summarized below.
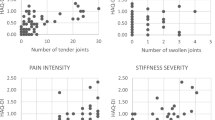
Hazes et al. (1993) investigated different measures of MS in 78 RA patients of median 60 years of age and a median disease duration of 9 years [31]. Two measures of MS severity and three measures of MS duration were compared (Table 2). Patients were grouped as 'active’ and 'inactive’ based on the physicians subjective impression of active joint inflammation.
MS was reported by 89% of patients in active and 81% in inactive disease. The duration of MS between the two groups was similar, with no significant differences between the groups, pointing to a lack of discriminative power of the three measures of MS duration. However, patients with active disease reported more severe MS than patients with inactive disease as measured by both severity scales, reflecting better discriminative properties for measures of severity vs measures of duration.
The sensitivity and specificity of the visual analogue scale (VAS) to distinguish between active and inactive disease was 85% and 44% respectively at a cut off of VAS > 2. In other words, with a MS VAS score of ≤2, there is a 44% chance to classify a patient correctly as inactive.
Khan et al. (2009) [32] investigated the utility of MS in assessing RA disease activity on data of the QUEST-RA database. A total of 5439 RA patients from 24 different countries and a mean disease duration of 11 years reported on MS duration from time of waking to time of maximal improvement. MS was studied separately for 4 different disease activity states classified according to DAS28 cut-offs for remission (<2.6), low (2.6 to ≤3.2), moderate (3.2 < to ≤ 5.1), and high (>5.1). In addition, the role of MS in Routine Assessment of Patient Index Data 3 (RAPID3, composed of the core set PROs pain, global health and physical functioning) to predict disease activity according to the DAS28 was explored.
MS duration was significantly different for each disease activity state, with the smallest difference (9 minutes) between low disease activity and remission. Although the duration of MS increased with disease activity, even patients whose disease seemed to be under control reported considerable duration of morning stiffness: of the 1594 patients with a DAS28 ≤ 3.2, 16% experienced morning stiffness of more than half an hour, of which 46% with a duration of more than one hour. Positive likelihood ratios of having active disease for different MS duration categories rose from 0.35 (0 min) to 4 (>60 min).
The accuracy of MS to differentiate between active and inactive disease (DAS28 cut off 3.2) was moderate, represented by the area under the receiver operating curve: 0.74 (0.72-0.75).
The relationship between RAPID3 and DAS28 was significantly different for each MS duration category. Interestingly, MS duration was especially valuable for RAPID3 scores representing low disease activity, where patients with low RAPID3 scores but a DAS28 > 3.2 were identified by presence of MS.
Discussion
This review identified 2 studies that investigated measures of stiffness in RA low disease activity states, both focussed on morning stiffness. There are large differences between the 2 studies in patient characteristics as well as in collection of outcome measures, making it difficult to draw overarching conclusions. Most importantly, this review highlights the lack of scientific data on the performance of stiffness measures in low disease activity states.
Both studies included in this review show that despite suppressed disease activity, morning stiffness is still present; in the Hazes study, 89 vs 80% and in the Khan study 79 vs 44% of active vs inactive patients report MS.
The study of Hazes et al. concludes that severity of MS measured with a VAS or NRS scale can discriminate between active and inactive disease, in contrast to measures of duration. On the other hand, Khan et al., show that the same measure of duration (measured in minutes from time of awaking to time of maximal improvement), in a much larger sample of RA patients, does show moderate discrimination between active and inactive RA. As the two studies differ in several ways, conflicting conclusions are not surprising. However, when looking closely, both studies show a similar difference in MS duration between active and inactive RA patients, with a difference of 60 minutes in the Hazes-study and 40 minutes in the Khan-study. This means that the most likely explanation for the difference in observations is the statistical power of the studies to detect differences in duration of MS between active and inactive patients, with the Hazes-study including 78 patients and the Khan-study 5439 patients; however, differences can also be attributed to differences in cut-off points for active and inactive RA (physician based vs DAS28 based); or to a change in patients perception of stiffness over the years in comparison to other RA symptoms and outcomes, as the Hazes study was published in 1993 and the Khan study in 2009. More research is needed to identify the best instrument to measure MS in low disease activity; not only focused on discrimination between active and inactive RA, but also on construct validity (whether low MS scores correlate with low scores on other disease activity measures) and sensitivity to pick up changes between low disease activity and remission states.
A limitation of this review of the literature is the decision not to document evidence of response of stiffness measures to therapy. As many studies do not mention stiffness in title, abstract or keywords this would have required a full-text review of almost every RA intervention study. Therefore, a specific search strategy was adopted in combination with a sensitive methodological PubMed search filter that is specially designed and validated for finding studies on measurement properties of measurement instruments [18].
Several studies provide evidence for validity of both duration as well as severity scales to measure stiffness, as both generally show good correlation with core set measures (especially pain and function) [19–22, 27, 28, 30]. However, problems arise when these measures are used to discriminate RA from non-inflammatory conditions or osteoarthritis [12, 24, 26, 31]. Yet, this is only relevant when it is used as a diagnostic criterion, which justifies the removal of stiffness as a component of the ACR classification criteria.
In general, studies comparing measures of duration with severity of stiffness show better measurement properties for severity in terms of sensitivity to change over time, responsiveness to therapy and reliability [10, 29, 31]. This is confirmed by the Hazes study included in this review, that shows discrimination between active and inactive disease of severity scales but not for measurement of duration of MS.
Qualitative studies investigating the concept of stiffness in RA point to the strong connection between aspects of stiffness and aspects of pain and physical functioning [25, 31]. This is confirmed by the Khan study, where MS correlates better with physical function, pain and global health than with joint counts or ESR. However, no specific measurement instruments have been developed from these qualitative explorations on the concept of stiffness. The observation that MS duration adds important information to predicting disease activity specifically at low RAPID3 scores is highly interesting, pointing to a possible distinguishing role for MS in classification of remission. To evaluate the contribution of MS to the newly developed ACR/EULAR remission criteria, new prospective studies on the performance of different MS measures in the spectrum of low disease activity are needed.
Conclusion
In conclusion: while patients in low disease activity frequently report stiffness, the tools to measure stiffness are of unknown validity due to a lack of data on performance of patient reported measures of stiffness in RA low disease activity or remission.
References
Straub RH, Cutolo M: Circadian rhythms in rheumatoid arthritis: implications for pathophysiology and therapeutic management. Arthritis Rheum. 2007, 56: 399-408. 10.1002/art.22368.
Cutolo M, Seriolo B, Craviotto C, Pizzorni C, Sulli A: Circadian rhythms in RA. Ann Rheum Dis. 2003, 62: 593-6. 10.1136/ard.62.7.593.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al: The American rheumatism association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-24. 10.1002/art.1780310302.
Anderson JJ, Felson DT, Meenan RF, Williams HJ: Which traditional measures should be used in rheumatoid arthritis clinical trials?. Arthritis Rheum. 1989, 32: 1093-9. 10.1002/anr.1780320907.
Anderson JJ, Firschein HE, Meenan RF: Sensitivity of a health status measure to short-term clinical changes in arthritis. Arthritis Rheum. 1989, 32: 844-50.
Buchbinder R, Bombardier C, Yeung M, Tugwell P: Which outcome measures should be used in rheumatoid arthritis clinical trials? clinical and quality-of-life measures’ responsiveness to treatment in a randomized controlled trial. Arthritis Rheum. 1995, 38: 1568-80. 10.1002/art.1780381108.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, et al: 2010 Rheumatoid arthritis classification criteria: an American college of rheumatology/european league against rheumatism collaborative initiative. Ann Rheum Dis. 2010, 69: 1580-8. 10.1136/ard.2010.138461.
Funovits J, Aletaha D, Bykerk V, Combe B, Dougados M, Emery P, et al: The 2010 American college of rheumatology/European league against rheumatism classification criteria for rheumatoid arthritis: methodological report phase I. Ann Rheum Dis. 2010, 2010 (69): 1589-95.
Neogi T, Aletaha D, Silman AJ, Naden RL, Felson DT, Aggarwal R, et al: The 2010 American college of rheumatology/European league against rheumatism classification criteria for rheumatoid arthritis: phase 2 methodological report. Arthritis Rheum. 2010, 2010 (62): 2582-91.
Westhoff G, Buttgereit F, Gromnica-Ihle E, Zink A: Morning stiffness and its influence on early retirement in patients with recent onset rheumatoid arthritis. Rheumatology (Oxford). 2008, 47: 980-4. 10.1093/rheumatology/ken137.
da Silva JA, Phillips S, Buttgereit F: Impact of impaired morning function on the lives and well-being of patients with rheumatoid arthritis. Scand J Rheumatol Suppl. 2011, 125: 6-11.
Yazici Y, Erkan D, Peterson MG, Kagen LJ: Morning stiffness: how common is it and does it correlate with physician and patient global assessment of disease activity?. J Rheumatol. 2001, 28: 1468-9.
Lineker S, Badley E, Charles C, Hart L, Streiner D: Defining morning stiffness in rheumatoid arthritis. J Rheumatol. 1999, 26: 1052-7.
Pinals RS, Masi AT, Larsen RA: Preliminary criteria for clinical remission in rheumatoid arthritis. Arthritis Rheum. 1981, 24: 1308-15. 10.1002/art.1780241012.
Felson DT, Smolen JS, Wells G, Zhang B, van Tuyl LH, Funovits J, et al: American college of rheumatology/European league against rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Ann Rheum Dis. 2011, 70: 404-13. 10.1136/ard.2011.149765.
van Tuyl LH, Hewlett S, Stamm T, Davis B, Flurey C, Hoogland W, et al: “Back to being normal”: the patient perspective on remission in rheumatoid arthritis [abstract]. Ann Rheum Dis. 2013, 72 (Suppl3): 562-
Cutolo M: How should morning function in rheumatoid arthritis be assessed? bibliographic study of current assessment. Scand J Rheumatol. 2011, 125 (Suppl): 17-22.
Terwee CB, Jansma EP, Riphagen II, de Vet HC: Development of a methodological PubMed search filter for finding studies on measurement properties of measurement instruments. Qual Life Res. 2009, 18: 1115-23. 10.1007/s11136-009-9528-5.
Borstlap M, Zant JL, van Soesbergen RM, van der Korst JK: Quality of life assessment: a comparison of four questionnaires: for measuring improvements after total hip replacement. Clin Rheumatol. 1995, 14: 15-20. 10.1007/BF02208079.
El Miedany Y, El GM, Youssef SS, Palmer D: Incorporating patient reported outcome measures in clinical practice: development and validation of a questionnaire for inflammatory arthritis. Clin Exp Rheumatol. 2010, 28: 734-44.
Fransen J, Langenegger T, Michel BA, Stucki G: Feasibility and validity of the RADAI, a self-administered rheumatoid arthritis disease activity index. Rheumatology (Oxford). 2000, 39: 321-7. 10.1093/rheumatology/39.3.321.
Hazes JM, Hayton R, Burt J, Silman AJ: Consistency of morning stiffness: an analysis of diary data. Br J Rheumatol. 1994, 33: 562-5. 10.1093/rheumatology/33.6.562.
Houssien DA, McKenna SP, Scott DL: The Nottingham health profile as a measure of disease activity and outcome in rheumatoid arthritis. Br J Rheumatol. 1997, 36: 69-73. 10.1093/rheumatology/36.1.69.
Leeb BF, Sautner J, Andel I, Rintelen B: SACRAH: a score for assessment and quantification of chronic rheumatic affections of the hands. Rheumatology (Oxford). 2003, 42: 1173-8. 10.1093/rheumatology/keg319.
Rhind VM, Unsworth A, Haslock I: Assessment of stiffness in rheumatology: the use of rating scales. Br J Rheumatol. 1987, 26: 126-30. 10.1093/rheumatology/26.2.126.
Wolfe F: Determinants of WOMAC function, pain and stiffness scores: evidence for the role of low back pain, symptom counts, fatigue and depression in osteoarthritis, rheumatoid arthritis and fibromyalgia. Rheumatology (Oxford). 1999, 38: 355-61. 10.1093/rheumatology/38.4.355.
Yazici Y, Pincus T, Kautiainen H, Sokka T: Morning stiffness in patients with early rheumatoid arthritis is associated more strongly with functional disability than with joint swelling and erythrocyte sedimentation rate. J Rheumatol. 2004, 31: 1723-6.
Sarzi-Puttini P, Fiorini T, Panni B, Turiel M, Cazzola M, Atzeni F: Correlation of the score for subjective pain with physical disability, clinical and radiographic scores in recent onset rheumatoid arthritis. BMC Musculoskelet Disord. 2002, 19: 18-
Vliet Vlieland TP, Zwinderman AH, Breedveld FC, Hazes JM: Measurement of morning stiffness in rheumatoid arthritis clinical trials. J Clin Epidemiol. 1997, 50: 757-63. 10.1016/S0895-4356(97)00051-6.
Ward MM: Clinical measures in rheumatoid arthritis: which are most useful in assessing patients?. J Rheumatol. 1994, 21: 17-27.
Hazes JM, Hayton R, Silman AJ: A reevaluation of the symptom of morning stiffness. J Rheumatol. 1993, 20: 1138-42.
Khan NA, Yazici Y, Calvo-Alen J, Dadoniene J, Gossec L, Hansen TM, et al: Reevaluation of the role of duration of morning stiffness in the assessment of rheumatoid arthritis activity. J Rheumatol. 2009, 36: 2435-42. 10.3899/jrheum.081175.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2474/15/28/prepub
Acknowledgements
This study was supported by an unconditional grant from Pfizer.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors have no competing interest concerning this study.
Authors’ contributions
All authors (LH, WF, MB) have made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; have been involved in drafting the manuscript and have given final approval of the version to be published.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
van Tuyl, L.H., Lems, W.F. & Boers, M. Measurement of stiffness in patients with rheumatoid arthritis in low disease activity or remission: a systematic review. BMC Musculoskelet Disord 15, 28 (2014). https://doi.org/10.1186/1471-2474-15-28
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2474-15-28