Abstract
Background
The PHQ-15 is widely used as an open access screening instrument for somatization syndromes in different health care settings, thus far, normative data from the general population are not available. The objectives of the study were to generate normative data and to further investigate the construct validity of the PHQ-15 in the general population.
Methods
Nationally representative face-to face household surveys were conducted in Germany between 2003 and 2008 (n=5,031). The survey questionnaires included, the 15-item somatization module from the Patient Health Questionnaire (PHQ-15), the 9-item depression module (PHQ-9), the Satisfaction With Life Scale (SWLS), the SF-12 for the measurement of health related quality of life, and demographic characteristics.
Results
Normative data for the PHQ-15 were generated for both genders and different age levels including 5031 subjects (53.6% female) with a mean age (SD) of 48.9 (18.1) years. Somatization syndromes occured in 9.3% of the general population. Women had significantly higher mean (SD) scores compared with men [4.3 (4.1) vs. 3.4 (4.0)]. Intercorrelations with somatization were highest with depression, followed by the physical component summary scale of health related quality of life.
Conclusions
The normative data provide a framework for the interpretation and comparisons of somatization syndromes with other populations. Evidence supports reliability and validity of the PHQ-15 as a measure of somatization syndromes in the general population.
Similar content being viewed by others
Background
Somatization is one of the most common issues in health care services, associated with substantial functional impairment and health care utilization [1–3]. Their valid and reliable acquisition is urgently necessary. Somatoform symptoms often account for sick leave and are characterized by long duration and medically unexplained symptoms [4–7]. The most frequently reported symptoms are fatigue, low energy, sleeping trouble, and pain (back pain, headaches, abdominal pain, and chest pain) [8, 9]. Medically unexplained symptoms are one of the key features of somatoform disorders. Although they are currently treated as both categorical (in terms of the diagnosis of somatoform disorders) and dimensional (in terms of quantitative measures of somatization/somatic symptom reporting), little is known about the empirical latent structure of medically unexplained symptoms. Accordingly to recent study results, the latent structure of somatization/somatic symptom reporting as assessed by the PHQ-15 is dimensional in both primary care and student samples [10].
Estimated prevalence rates of undifferentiated somatoform disorders vary between 8.6%-25.6% in primary care, depending on the chosen screening instrument and whether pain is taken into account or not [8, 11–13]. Recent reported data on somatoform symptom clusters in the general population are still scarce [14]. Wittchen and colleagues (2011) reported in their systematic review a 12-month prevalence of somatoform disorders of 6.3% in the EU with little evidence for considerable cultural or country variation [15]. 4-week, 12-month and lifetime prevalence rates of any somatoform disorder in the German general population was reported with 7.5%, 11.0%, and respectively 16.2% [16].
Most clinicians nowadays evaluate, whether or not the reported somatoform complaints are associated with distress and psychological impairment, both predictors for somatoform disorders [17]. Screening instruments can add valuable diagnostic information, yet they vary considerably in length and diagnostic focus (for an overview of measures used in clinical trials of somatoform disorders see [18]). Patients often complain about the amount of items, which can lead to a difficult doctor-patient relationship and lower self-perception of quality of life and life satisfaction [1, 19–21]. The reported impairment of every day functioning can be even higher when the patients are affected by comorbid conditions as depression and/or anxiety, which occurs in up to 43% with increasing number of physical symptoms [11, 17, 22]. A difficult encounter, as perceived by the clinician, may be another predictor of psychiatric comorbidity in patients who have somatoform symptoms [22]. The collaboration between patients and their doctors might also carry the risk of shaping, reinforcing, and legitimizing somatoform syndromes [23]. Hence it is important to take standardized assessment of somatization into account. These measures can have a variety of uses, including screening, early pre-diagnosis, assessment of severity, and gauging treatment decisions of both clinicians and patients.
The PHQ-15 is a self-administered somatic symptoms subscale, derived from the full Patient-Health-Questionnaire [7, 24]. Relatively brief, it screens for 15 somatic symptoms that account for more than 90% of the physical complaints reported in the outpatient setting (exclusive of self-limited upper respiratory symptoms) [20]. The PHQ-15 is a valid measure, which has been used in 40 studies so far in different health care settings (for an overview see [11]). Valid and reliable measures for the assessment of somatic symptoms, as the PHQ-15, have been used in psychiatric research and routinely in clinical practice so far (i.e. primary care). Normative data, which could be used to compare a subject's scale score with those determined from a general population reference group, are still scarce and restraint to relative risk factors [25]. The obtained findings could be further utilized as reference categories in community studies and open-access web-based screening tools [15, 26, 27].
In this study we provide normative data for the PHQ-15 for different age groups and both genders. In addition we address the relations of somatic symptoms with depression, and quality of life and life satisfaction to provide further evidence for the construct validity in a general population. According to previous results, we expect that higher PHQ-15 scores will be associated with worsening quality of life and life satisfaction as well as with increased depression [11].
Methods
Study sample
Nationally representative face-to face household surveys were conducted in Germany between 2003 and 2008 (n=5,031), representative of the German general population, with the assistance of an institute specialized for demographic research (USUMA, Berlin) according to the German law of data protection (§30a BDSG) and with written consent. Previously ethics were weighted to the respective interests of the public and of the individuals concerned following §823 (BGB) of the Civil Code of Law and in accordance with the guidelines in the Declaration of Helsinki. Representativeness was assured through a weighting process. Age, gender, and educational level were the major criteria for representativeness according to the register of the Federal Elections. Two callbacks had to be without success before an address was considered a failure. The sampling procedure consisted of sample points, household, and persons in the last stage. Target households within the sample points were determined using the random-route procedure: choosing sample point areas within Germany, randomly choosing households within these areas, and randomly choosing target persons within these households.
Sample characteristics
Attempts were made to contact 8008 persons. The set of questionnaires was administered to a sample of 5031 persons. Therefore the response rate was 62.8%. The main reasons for non-participation (37.2%) were: the general information request was refused (15.8%), the interview request was refused (7.9%), or there was no one at home for three times in a row (7.3%).
Sociodemographic characteristics of the sample are reported in Table 1. The analysis of the distribution of the data yielded skewness and kurtosis values of somatization of 1.63 and 3.29, respectively. We therefore decided to investigate group differences for sociodemographic characteristics using non-parametric tests.
There were significant gender, age, education level, employment status, and income effects in the general population associated with a higher PHQ-15 score. The most marked group and the lowest groups were considered calculating the value of Cohen’s d using the means and standard deviations. As noted in Table 1, the calculated effect sizes were moderate for income and education, and high for age. Gender and employment status yielded small effect sizes.
Instruments
Somatization (PHQ-15)
Somatization was measured using the somatic symptom module of the PHQ, the PHQ-15 [7, 28]. The items include the most prevalent DSM-IV somatization disorder somatic symptoms [29]. Subjects were asked for the last 4 weeks to rate the severity of 13 symptoms as 0 (“not bothered at all”), 1 (“bothered a little”), or 2 (“bothered a lot”). Two additional physical symptoms - feeling tired or having little energy, and trouble sleeping – are contained in the PHQ-9 depression module. For scoring, response options for these two symptoms are coded as 0 (“not at all”), 1 (“several days”), or 2 (“more than half the days” or “nearly every day”).
Thus, the total PHQ-15 score ranges from 0 to 30 and scores of ≥5, ≥10, ≥15 represent mild, moderate and severe levels of somatization. The reliability and validity of the PHQ-15 are high in clinical and occupational health care settings [2, 7, 11].
Depression (PHQ-9)
Depression was assessed with the PHQ nine item depression module (PHQ-9) [30]. Each of the nine PHQ depression items corresponds to one of the DSM-IV Diagnostic Criterion A symptoms for major depressive disorder [29]. Subjects were asked how often, over the last two weeks, they have been bothered by each of the depressive symptoms. Response options are “not at all”, “several days”, “more than half the days”, and “nearly every day”, scored as 0, 1, 2 and 3, respectively. PHQ-9 scores range from 0 to 27, with scores of ≥5, ≥10, ≥15, representing mild, moderate and severe levels of depression severity [31]. Psychometric properties of the PHQ-9 are well documented (for an overview see [11]).
Quality of life (SF-12)
The SF-12 is an ubiquitary adopted generic questionnaire on the subjectively perceived health-related quality of life and records the overall subjective state of health of adults for different diseases, in relation to their physical, psychological, and social aspects [32]. A longer version of the SF-12, the SF-20, was already previously used to assess functional impairment in combination with the PHQ-15 [7, 17].
SF-12 scales are namely: general health, physical functioning, role physical, bodily pain, vitality, social functioning, mental health, role emotional, yielding the summary scales physical- and mental health.
Life satisfaction (SWLS)
Satisfaction with life was measured with the Satisfaction With Life Scale, designed to measure global cognitive judgments of satisfaction with one's life, and consists of five items [33, 34]: “In most ways my life is close to my ideal”, “The conditions of my life are excellent”, “I am satisfied with my life”, “So far I have gotten the important things I want in life”, and “If I could live my life over, I would change almost nothing”.
Respondents indicated the extent to which they agreed with each item on a seven-point Likert scale ranging from “strongly agree” to “strongly disagree”. Translations of the SWLS into various languages are available and psychometric properties have been reviewed [35].
Internal consistencies
The parameter of internal consistency (Cronbach’s α) for the PHQ15 scale reached the value of α =0.82, for the PHQ-9 α=0.88 respectively. The Satisfaction with Life Scale showed a very good Cronbach’s α of 0.91. Cronbach’s α for the mental component scale (MCS) was 0.84, 0.91 respectively for the physical component scale (PCS) of the SF-12.
Data analysis
For reliability, internal consistency of the PHQ-15 was assessed. Base rates for single symptoms were calculated using frequency analysis. Descriptive statistics included analyses of prevalence. To determine prevalence rates, a cut-off score of ≥10 was used on the PHQ-15 because the range of ≥10 up to 30 reflects medium and high somatic symptom severity, respectively [7]. The selection of this cut-off score resulted in previous studies in a sensitivity of 80.2% und specifity of 58.5% for a somatoform disorder [3]. For construct validity, we investigated PHQ-15 scale intercorrelations with the PHQ-9 [7, 30], the SF-12 [32], and the Satisfaction With Life Scale [33]. In addition, we investigated group differences for sociodemographic characteristics using χ 2 -test and Kruskal-Wallis-test, respectively. Based on results from previous studies with the PHQ-15, we expected that women would have higher somatization scores compared with men and that levels of somatization increase with age and lower levels of education [8]. To provide normative data for the PHQ-15, we generated age- and gender specific percentiles for the PHQ-15 total score. Sample size was sufficient to be divided into gender-specific age groups comprising 10 years each. Statistical analyses were conducted using SPSS with an α-level of 1%. According to previous other studies with the PHQ-15 [11, 17], missing values were replaced with the mean value of the remaining items if the number of missing items was below 20%. If the number of missing items in the scale exceeded 20%, the sum score was not computed and counted as missing.
Results
Prevalence of somatization syndromes
By using the cut-off scores described below, the total prevalence of somatization syndromes at a moderate to high level was estimated to be 9.3%; 8.1% of the men and 10.3% of women had a PHQ-15 sum score ≥10.
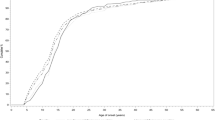
Base rates of single symptoms
The gender-stratified prevalence rates of the individual symptoms are shown in Figure 1. The most common symptoms were various types of pain (back pain, headache, pain of the joints and extremities) with prevalence rates >35%, if symptom reporting of any degree of severity was considered for both genders. Highest rates for severe symptom rating were found for the same symptoms (>4%). Further 2.4% of the total sample complained about sleeping trouble and 1.4% of a lack of energy nearly every day.
Construct validity
The intercorrelations between the PHQ-15 total score and the PHQ-9 depression scale, the SF-12 for the assessment of quality of life (physical and mental factor), and the Satisfaction with Life Scale are summarized in Table 2. Intercorrelations with somatization were highest with depression (r=0.75 p<0.001), followed by the physical component summary scale of health related quality of life (r=−0.64 p<0.001), and the subscale “bodily pain” respectively (r=−0.68 p<0,001). Intercorrelation of depression was higher with the mental component summary scale of health related quality of life (r=−0.68 p<0.001) than the physical component (r=−0.48 p<0,001) compared to somatization. Two items, “feeling tired or having little energy” and “trouble falling asleep, or sleeping too much” represent shared questions between the PHQ-9 and the PHQ-15. Omitted from the somatization scale, the intercorrelation reduced from 0.75 to 0.65 (p<0.001).
Both somatization and depression were significantly related to life satisfaction.
The associations of the PHQ-15 scores with demographic characteristics are shown in Table 1. As hypothezised, PHQ-15 scores increased with age, and women exhibited higher scores than men. Also in accordance with the hypotheses, scores for somatization syndromes were higher in subjects with lower educational levels compared to subjects with higher educational levels. No differences were found in terms of relationship or employment status.
Normative data
Table 3 summarizes the normative data for the different age levels and both genders. Percentiles from this table can be used to compare an individual subject’s PHQ-15 score with those determined from the general population reference group based on age and gender.
For example, a PHQ-15 score of 11 in a 30-year-old man indicates a percentile rank of 93.4% in the total population and of 98.9% in a group of subjects of the same age and gender. Likewise, a PHQ-15 score of 11 in a 30-year-old woman corresponds to a percentile rank of 93.4% in the total population and of 94.9% in the same age and gender group.
Discussion
A main result of this study was the standardization of the PHQ-15 with the provision of normative data from the general population. Given that age and gender specific comparative data were generated based on subgroups consisting of n=156 to 542 subjects each, the sample sizes were sufficient to provide normative data. Results of a standardization study of the Patient Health Questionnaire-4 (PHQ-4) on depression and anxiety, yielded that the German general population could be considered comparable to the American general population [36]. The prevalence rate of 9.3% for somatization syndromes corresponds to previous results of surveys in the general population reporting on any somatoform disorder [16] and can be considered for further exploration for the presence of the spectrum of subclinical to full somatoform disorder in clinical practice [3, 7]. Previous studies in the general population on base rates for somatoform symptoms report similar frequencies and dominance of various types of pain [9, 14]. In primary care the different pain symptoms are also the most prominent ones, accompanied by “lack of energy” and “trouble sleeping” as an indicator of exacerbation [8].
The present study, including more than 5000 subjects, gives evidence that the PHQ-15 is not only a reliable and valid self-report measure for somatization in health care settings but also in the general population. Specifically, the intercorrelations of the PHQ-15 with the PHQ-9 depression scale (r = 0.65-0.75), the SF-12 quality of life scale (r = −0.53-0.68), and the life satisfaction scale (r = −0.37) are similar to intercorrelations between these concepts in other studies suggesting further construct validity of the PHQ-15 [11]. In the original PHQ-15 validation study, which comprised of 6,000 unselected primary care patients, higher PHQ-15 scores were also strongly associated with worsening function on all six SF-20 scales - a longer version of the SF-12 used in the present study -, as well as increased disability days and health care utilization [7, 17]. The impact on the physical component scale of the SF-12 was higher for somatization than for depression. The expressed mental component scale showed higher associations with depression than somatization. The high association of somatization and depression in the present study might be partly explained by the overlap of two items in the PHQ-15 and PHQ-9 (“lack of energy”, “sleep disturbance”). Yet these results of concurrent validity are supported by a former study of the PHQ-15 in relation to depression and general mental health [37]. The comorbidity of somatic, anxiety and depressive symptoms (the “SAD” triad) is well-established [11, 20]. Still the concordance could not be found in immunological parameters, where results suggest different immune alterations in somatization syndrome and depression [38]. What is known, is that physiological activity (i.e. heart rate, tension) is high in patients with somatization and may interact with psychological processes [39].
The controverse discussion on the classifying of somatoform disorders, respectively syndromes, would have gone beyond the purpose of this study (for an overview see [18]). Although the PHQ-15 does not explicitly ask for “medically unexplained symptoms”, it is highly associated with clinician-rated somatoform disorder symptom counts [40].
Yet a potential limitation of this general population study is that it did not include standard criterion interviews, which would have allowed for calculating specificity and sensitivity for optimal cut point and construction of a receiver operating characteristic (ROC). The sensitivity and specificity of the PHQ-15, as measured by the concordance with the SCID-I diagnosis of somatoform disorders, has previously been established as 78% and 71%, respectively, in primary care [41]. Another limitation might be that normative data were not reported according to the socioeconomic status.
Reviews have identified effective behavioural and pharmacological interventions for somatoform disorders [42–45], and guidelines are close to be published (e.g. S3-guideline). Reported “green flags” or prognostic factors are so far: (a) proactive coping strategies of the patient, e.g. optimism, motivation for psychotherapy; (b) healthy lifestyle, e.g. balanced diet, relaxation, exercising, and enough sleep; (c) social support; and (d) a good doctor-patient relationship with shared decision making.
Reducing the burdens and enhancing early detection of mental disorders in general requires major shifts in research, clinical practice, and public health by incorporating multidisciplinary models of intervention. The good news is that such changes are under way, as reflected, for example by the experts drafting Research Roadmaps (see http://www.roamer-mh.org) for the European Union and the U.S. (see http://www.nihpromis.org).
Conclusions
Somatization is one of the most common issues in health care services, associated with substantial functional impairment and health care utilization. Somatization syndromes occur in 9.3% of the general population. Thus validate acquisition of somatoform symptoms is necessary in several health care settings. The PHQ-15 is a good basis for this task. Normative data for the PHQ-15 in the general population were generated for both genders and different age levels and can be used for the interpretation and comparisons with other populations.
References
Steinbrecher N, Koerber S, Frieser D: The prevalence of medically unexplained symptoms in primary care. Psychosom. 2011, 52: 263-71. 10.1016/j.psym.2011.01.007.
De Vroege L, Hoedeman R, Nuyen J: Validation of the PHQ-15 for somatoform disorder in the occupational health care setting. J Occup Rehabil. 2011, 22: 51-58.
Korber S, Frieser D, Steinbrecher N: Classification characteristics of the Patient Health Questionnaire-15 for screening somatoform disorders in a primary care setting. J Psychosom Res. 2011, 71: 142-7. 10.1016/j.jpsychores.2011.01.006.
Burton C, Weller D, Marsden W: A primary care symptoms clinic for patients with medically unexplained symptoms: pilot randomised trial. BMJ Open. 2012, 2: e000513-10.1136/bmjopen-2011-000513.
Hiller W, Fichter MM, Rief W: A controlled treatment study of somatoform disorders including analysis of healthcare utilization and cost-effectiveness. J Psychosom Res. 2003, 54: 369-80. 10.1016/S0022-3999(02)00397-5.
Hiller W, Fichter MM: High utilizers of medical care: a crucial subgroup among somatizing patients. J Psychosom Res. 2004, 56: 437-43. 10.1016/S0022-3999(03)00628-7.
Kroenke K, Spitzer RL, Williams JB: The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002, 64: 258-66.
Hanel G, Henningsen P, Herzog W: Depression, anxiety, and somatoform disorders: vague or distinct categories in primary care? Results from a large cross-sectional study. J Psychosom Res. 2009, 67: 189-97. 10.1016/j.jpsychores.2009.04.013.
Hiller W, Rief W, Brahler E: Somatization in the population: from mild bodily misperceptions to disabling symptoms. Soc Psychiatry Psychiatr Epidemiol. 2006, 41: 704-12. 10.1007/s00127-006-0082-y.
Jasper F, Hiller W, Rist F: Somatic symptom reporting has a dimensional latent structure: results from taxometric analyses. J Abnorm Psychol. 2012, 121: 725-38.
Kroenke K, Spitzer RL, Williams JB: The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010, 32: 345-59. 10.1016/j.genhosppsych.2010.03.006.
Mergl R, Seidscheck I, Allgaier AK: Depressive, anxiety, and somatoform disorders in primary care: prevalence and recognition. Depress Anxiety. 2007, 24: 185-95. 10.1002/da.20192.
Barkow K, Heun R, Ustun TB: Identification of somatic and anxiety symptoms which contribute to the detection of depression in primary health care. Eur Psychiatry. 2004, 19: 250-7. 10.1016/j.eurpsy.2004.04.015.
Rief W, Hessel A, Braehler E: Somatization symptoms and hypochondriacal features in the general population. Psychosom Med. 2001, 63: 595-602.
Wittchen HU, Jacobi F, Rehm J: The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011, 21: 655-79. 10.1016/j.euroneuro.2011.07.018.
Jacobi F, Wittchen HU, Holting C: Prevalence, co-morbidity and correlates of mental disorders in the general population: results from the German Health interview and examination Survey (GHS). Psychol Med. 2004, 34: 597-611. 10.1017/S0033291703001399.
Lowe B, Spitzer RL, Williams JB: Depression, anxiety and somatization in primary care: syndrome overlap and functional impairment. Gen Hosp Psychiatry. 2008, 30: 191-9. 10.1016/j.genhosppsych.2008.01.001.
Kroenke K: Somatoform disorders and recent diagnostic controversies. Psychiatr Clin North Am. 2007, 30: 593-619. 10.1016/j.psc.2007.08.002.
Schumacher S, Rief W, Brahler E: Disagreement in doctor's and patient's rating about medically unexplained symptoms and health care use. Int J Behav Med. 2011, 2011: 2011-
Kroenke K: Patients presenting with somatic complaints: epidemiology, psychiatric comorbidity and management. Int J Methods Psychiatr Res. 2003, 12: 34-43. 10.1002/mpr.140.
Hahn SR, Thompson KS, Wills TA: The difficult doctor-patient relationship: somatization, personality and psychopathology. J Clin Epidemiol. 1994, 47: 647-57. 10.1016/0895-4356(94)90212-7.
Kroenke K, Rosmalen JG: Symptoms, syndromes, and the value of psychiatric diagnostics in patients who have functional somatic disorders. Med Clin North Am. 2006, 90: 603-26. 10.1016/j.mcna.2006.04.003.
Stanley IM, Peters S, Salmon P: A primary care perspective on prevailing assumptions about persistent medically unexplained physical symptoms. Int J Psychiatry Med. 2002, 32: 125-40. 10.2190/AVM3-8GU8-JW70-5RX5.
Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999, 282: 1737-44. 10.1001/jama.282.18.1737.
Mewes R, Rief W, Brahler E: Lower decision threshold for doctor visits as a predictor of health care use in somatoform disorders and in the general population. Gen Hosp Psychiatry. 2008, 30: 349-55. 10.1016/j.genhosppsych.2008.04.007.
Härter M, Kentgens M, Brandes A, Bock T, Dirmaier J, Erzberger M, Fürstenberg W, Hillebrandt B, Karow A, Knesebeck O, König HH, Löwe B, Meyer HJ, Romer G, Rouhiainen T, Scherer M, Thomasius R, Watzke B, Wegscheider K, Lambert M: Rationale and content of psychenet: the Hamburg Network for Mental Health. Eur Arch Psychiatry Clin Neurosci. 2012, published online 13 September 2012
Inc P: PHQ-Screeners. 2002, http://www.phqscreeners.com. 19 March 2013
Löwe BSR, Zipfel S, Herzog W: Gesundheitsfragebogen für Patienten (PHQ D). Komplettversion und Kurzform. Testmappe mit Manual, Fragebögen, Schablonen. 2. Auflage. 2002, Karlsruhe: Pfizer
APA: Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (4th edition). 2000, Washington DC: American Psychiatric Press
Lowe B, Kroenke K, Herzog W: Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004, 81: 61-6. 10.1016/S0165-0327(03)00198-8.
Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001, 16: 606-13. 10.1046/j.1525-1497.2001.016009606.x.
Gandek B, Ware JE, Aaronson NK: Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998, 51: 1171-8. 10.1016/S0895-4356(98)00109-7.
Schumacher J: SWLS - Satisfaction With Life Scale. Diagnostische Verfahren zu Lebensqualität und Wohlbefinden. Edited by: Schumacher J, Klaiberg A, Brähler E. 2003, Göttingen: Hogrefe, 305-309.
Diener E, Emmons RA, Larsen RJ: The Satisfaction With Life Scale. J Pers Assess. 1985, 49: 71-5. 10.1207/s15327752jpa4901_13.
Pavot W, Diener E: Review of the Satisfaction With Life Scale. Psychol Assess. 1993, 5: 164-72.
Lowe B, Wahl I, Rose M: A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010, 122: 86-95. 10.1016/j.jad.2009.06.019.
Han C, Pae CU, Patkar AA: Psychometric properties of the Patient Health Questionnaire-15 (PHQ-15) for measuring the somatic symptoms of psychiatric outpatients. Psychosom. 2009, 50: 580-5.
Rief W, Pilger F, Ihle D: Immunological differences between patients with major depression and somatization syndrome. Psychiatry Res. 2001, 105: 165-74. 10.1016/S0165-1781(01)00338-9.
Rief W, Auer C: Is somatization a habituation disorder? Physiological reactivity in somatization syndrome. Psychiatry Res. 2001, 101: 63-74. 10.1016/S0165-1781(00)00240-7.
Interian A, Allen LA, Gara MA: Somatic complaints in primary care: further examining the validity of the Patient Health Questionnaire (PHQ-15). Psychosom. 2006, 47: 392-8. 10.1176/appi.psy.47.5.392.
van Ravesteijn H, Wittkampf K, Lucassen P: Detecting somatoform disorders in primary care with the PHQ-15. Ann Fam Med. 2009, 7: 232-8. 10.1370/afm.985.
Smith RC, Lein C, Collins C: Treating patients with medically unexplained symptoms in primary care. J Gen Intern Med. 2003, 18: 478-89. 10.1046/j.1525-1497.2003.20815.x.
Jackson JL, O'Malley PG, Kroenke K: Antidepressants and cognitive-behavioral therapy for symptom syndromes. CNS Spectr. 2006, 11: 212-22.
Kroenke K: Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med. 2007, 69: 881-8. 10.1097/PSY.0b013e31815b00c4.
Kleinstauber M, Witthoft M, Hiller W: Efficacy of short-term psychotherapy for multiple medically unexplained physical symptoms: a meta-analysis. Clin Psychol Rev. 2011, 31: 146-60. 10.1016/j.cpr.2010.09.001.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-244X/13/91/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RK participated in the study design, performed statistical analysis and drafted the manuscript. AH participated in the study design and advised for analysis. EB participated in the sequence alignment and acquisition of data and conceived of the study, and participated in its design and coordination. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kocalevent, RD., Hinz, A. & Brähler, E. Standardization of a screening instrument (PHQ-15) for somatization syndromes in the general population. BMC Psychiatry 13, 91 (2013). https://doi.org/10.1186/1471-244X-13-91
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-244X-13-91