Abstract
Background
Cervical cancer is due to infection with specific high-risk types of human papillomavirus (HPV). Although the incidence of genital HPV infection in various population groups is high, most of these regress without intervention. Investigating genetic host factors and cellular immune responses, particularly cytokines, could help to understand the association between genital HPV infection and carcinogenesis. The tumor necrosis factor alpha (TNF-α) cytokine plays an important role in all stages of cervical cancer and has the ability to induce the regression of human tumors. Therefore the aim of the study was to investigate the allelic distribution of -308 TNF-α gene polymorphism in South African women with cervical cancer compared to control women.
Methods
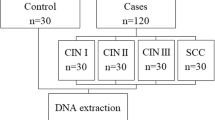
Included in our study were women with histologically proven cancer of the cervix (n = 244) and hospital-based controls (n = 228). All patients and controls were from mixed race and black population groups in South Africa. The detection of a bi-allelic -308 (A/G) polymorphism in the promoter region of TNF-α was investigated using the amplification refractory mutation system-polymerase chain reaction (ARMS-PCR) technique. The distributions of the allelic frequencies were stratified in both patients and controls into two South African ethnic population groups.
Results
In this study we observed no association between the distribution of -308 TNF-α polymorphism and the risk of developing cervical cancer even after combining the data from the two ethnic populations (X2 = 2.26). In addition, using the chi-squared test we found no significant association between the known risk factors for cervical cancer and the allele distribution of -308 TNF-α. However, the frequency of the rare high-producing allele -308A of TNF-α was significantly lower in the South African population when compared to Caucasians and Chinese population groups.
Conclusion
We demonstrated no association between -308 TNF-α polymorphism and the risk of cervical cancer among two South African ethnic population groups. However, as the distribution of the -308A TNF-α was notably different between the control groups of South Africa and other population groups this result suggests that ethnic disparity may influence the levels of TNF-α produced.
Similar content being viewed by others
Background
There is strong epidemiological and experimental data that have demonstrated a definite association of high-risk human papillomavirus (HR-HPV) infection and the development of cervical cancer [1]. Interestingly, although most sexually active women in the normal population have asymptomatic cervical HPV infections, most of these cervical infections are transient, with clearance in 70% to 90% of individuals positive for HPV DNA. In addition, only a small percentage develops long-term HPV infection, which is associated with an increased risk of developing cervical cancer [2]. Thus, an effective host immune response may be an important determinant for the persistence and progression of HPV induced cervical cancer. In particular, cell-mediated immunity (CMI) is important in controlling both HPV infections and HPV-associated neoplasms [3]. CMI is regulated by cytokines that are secreted primarily by T helper (Th) cells and macrophages.
Cytokines play a significant role in the defense against HPV induced infections, modulating viral replication and polarizing the immune response to a Th1 (cellular) or Th2 (humoral) pattern [1]. Th1 cells are immuno-stimulatory and are associated with the clearance of HPV infection and regression of cervical intraepithelial neoplasia [4] Th2 cells are immuno-inhibitory and are capable of stimulating tumor growth [5]. Investigating genetic host factors and immune responses could help to understand the association between genital HPV infection and carcinogenesis [6], as cervical cancer is the second most common female cancer worldwide and the most common cancer in South Africa among women, which continues to be a public health burden. Several candidate gene studies have demonstrated that genetic polymorphisms in cytokine genes contribute to the variation in the levels of cytokine produced and this variation may influence the severity of several infectious diseases [7–9]. Among them the pro-inflammatory cytokine, tumor necrosis factor-alpha (TNF-α) has been of particular interest as it was found to be located in the central major histocompatibility complex (MHC) and a possible genetic correlation between TNF alleles and disease susceptibility was hypothesized [10].
TNF-α is a multifunctional cytokine that was originally identified as a macrophage-derived serum protein that mediates necrosis of solid tumors in vitro and in vivo [11]. In addition, TNF has been shown to mediate carcinogenesis through induction of proliferation, invasion, and metastasis of tumor cells [12]. Furthermore, it was shown that the expression of TNF-α is regulated at the transcriptional level [13] and various polymorphisms within the TNF-α promoter region have been associated with the level of TNF-α produced [10, 14, 15]. Several investigators have studied the polymorphisms within the TNF-α promoter region to estimate the immune responses to a wide range of cancers [9, 16, 17] including cervical cancer [18, 19]. In particular, the biallelic polymorphism in the promoter region at position -308 relative to the transcriptional start site of the gene, representing a transition from the nucleotides guanine (G) to adenine (A) has been commonly studied. This -308G/A transition affects the expression of TNF-α where the less common -308A allele produces higher levels of TNF-α, while the -308G allele is linked to a reduced TNF-α production [10, 20]. Indeed, these observations presented the possibility that tumor development may be associated to the genetic predisposition of the host to produce higher levels of TNF-α. Numerous studies have investigated the association between the effect of TNF-α promoter region and cervical cancer, but the results have been contradictory [9, 18, 21, 22]. Notably, these findings are from different population groups and thus indicate that the variation in TNF-α production may be influenced by the genetic make-up of diverse population groups contributing to a disparity in disease outcome.
Therefore, given the importance of TNF-α in potentially contributing to the progression of cervical cancer with variations in the levels of TNF production in different population groups, we investigated the biallelic polymorphism in the -308 promoter region of the TNF-α gene using the ARMS-PCR methodology and examined its relationship to the development of cervical cancer among two South African ethnic groups.
Methods
Patients and control populations
Individuals were selected from a case-control study of cancer of the cervix and related risk factors conducted among colored (mixed racial descent) and black women residing in the Western Cape Province of South Africa, from January 1998 to December 2001 [23]. The Research Ethics Committee, Faculty of Health Sciences, University of Cape Town, South Africa, approved the case-control study. Cases were women with invasive cancer of the cervix attending Gynae-oncology clinics at 2 tertiary hospitals. The controls, who were hospital based, were women with primary diagnosis such as trauma or acute infections that were judged to be independent of contraceptive use and had no history or evidence of cervical disease and were identified at the 2 tertiary hospitals. The controls were series matched to cases for decade age, ethnic group and area of residence. Data on known risk factors and potential confounders were collected using a detailed questionnaire administered by trained nurse interviewers. Papanicoloau (Pap) smears were taken from all control women. Blood samples from randomly selected 244 eligible cervical cancer patients and 228 hospital-based controls were analysed for the -308 polymorphisms in the promoter region of TNF-α.
DNA extraction
Genomic DNA was extracted from 200 μl of whole blood using the QiAamp Spin Blood Kit (QIAGEN, Valencia, CA) in accordance with manufacturer's instructions.
Cytokine genotyping
The A and G alleles at position -308 in the promoter region of the TNF-α gene were identified using the amplification refractory mutation system polymerase chain reaction (ARMS-PCR) methodology as previously described [24]. A total of 2 ul (25–100 ng) of DNA was used in each ARMS-PCR reaction. The PCR primer sequences were as follows:
Generic primer (antisense): 5'-tctcggtttcttctccatcg-3'
Primer G, allele1 (sense): 5'-ataggttttgaggggcatgg-3'
Primer A, allele2 (sense): 5'-aataggttttgaggggcatga-3'
The amplified ARMS-PCR products (PCR product size = 184 bp) were identified by gel electrophoresis on 2 % agarose gels stained with ethidium bromide.
Statistical analysis
Statistical analyses were performed using STATA version 8. The allele frequency of the -308 TNF-α polymorphism was compared between the patients and control groups using the X 2 test. Unconditional logistic regression was used to estimate odds ratios (OR's) for developing cancer of the cervix in relation to the -308 TNF-α gene polymorphism. These OR's were adjusted for the following confounding factors; ethnic group, 5 year age group, years of education, age at first sexual intercourse, number of sexual partners, urban/rural living, number of Pap smears, injectable/oral contraceptive use, smoking, and parity.
Results
To evaluate the accuracy of the assigned TNF-α genotypes a total of twenty-five samples were randomly chosen and the results were confirmed by repeating the ARMS-PCR. Notably there were no discrepant results detected when the ARMS-PCR assay was repeated on the samples.
The genotype distribution of the polymorphism at position -308 of the TNF-α promoter region in the cases and controls among the two South African ethnic groups are shown in Table 1. There were no significant differences in the distribution of TNF-α allelic polymorphisms and the risk of developing cervical cancer in the mixed race group, (OR, 2.93; 95% CI, 0.51–16.72) or the black group (OR, 0.87; 95% CI, 0.27–2.76). In addition, when the data was adjusted for potential confounding factors (adjusted for 5 year age group, education, age at first sex, number of sexual partners, number of Pap smears, injectable/oral contraceptive use, smoking, and parity), no significant association was observed (data not shown).
As there were no significant differences in the distribution of the -308 TNF-α alleles in the cervical cancer patients among the two South African ethnic populations, the data was combined to compare allele distributions to other population groups (Table 2). Interestingly, the genotype distribution of the -308 TNF-a genotypes for the South African cancer cases were different to those reported in a Korean population group (homozygous GG 71% vs 90%; and heterozygous AG 26% vs 6%). In addition, the distributions of the -308 TNF-α alleles in the two South African control groups were combined to compare the genotype distribution to other population groups (Table 3). The genotype distribution for the homozygous GG and AA -308 genotypes for the combined South African data were similar to those reported in Zimbabwean [21], Chinese [25]; Italian [26] and Korean [14] populations. However, the distribution of the heterozygous AG genotype was notably different in the Chinese and Korean compared to the South African control group (8% versus 20 %). In addition, there was an increased frequency of the -308 TNF-α A allele and decrease in the G allele in the British Caucasoid group [24] when compared to the South African population group.
Discussion
Although the Pap smear screening has reduced cervical cancer mortality in developed countries, 35000 women die from this disease every year in the United States and Europe [27]. The current treatments for cervical cancer are invasive, costly, limited, uncomfortable, inefficient and recurrence is a common outcome [28]. There are several prophylactic and therapeutic clinical HPV vaccine trials that are in progress [29, 30], which may assist in reducing this disease burden worldwide. However, while these strategies are commendable it is important to investigate other host or viral markers that contribute to the different stages of cervical disease and thus may provide an effective tool for the treatment of cervical cancer. It is accepted that persistent HRHPV-induced infection is the hallmark of cervical cancer.
Indeed, other co-factors such as viral load, lifestyle factors, high parity, smoking, long-term use of contraceptives and other sexually transmitted diseases have also been established as risk cofactors for cervical cancer among women with persistent HPV infections [31]. In addition, several studies have indicated that the polymorphisms in the promoter region of -308 TNF-α may be a contributing factor for the development of cervical cancer [18, 21, 32]. However, the results of these studies have been contradictory. Thus in the present study we sought to identify the possible link between -308 A/G TNF-α allele polymorphism and the progression of cervical cancer among two ethnic population groups in South Africa. We found no significant differences between the -308TNF-α allele polymorphism and cervical cancer risk among the two South African ethnic population groups. In addition we observed no significant differences in the distribution of the high (AA), medium (AG) or low (GG) genotypes of TNF-α among the South African cervical cancer patients and healthy controls (and in the combined race groups) (X 2 = 2.26) even when the data were adjusted for potential confounders (data not shown).
The findings in our study are similar to those reported by Stanczuk et al., [21], who investigated the association of -308TNF-α gene polymorphism with cervical cancer among a Zimbabwean population [21]. They found no significant differences in the distribution of the high, medium or low producing alleles in the cervical cancer patients and healthy women. However, their study was based on a small sample size and the authors suggested that a larger cohort should be investigated to challenge this association, as their lack of association using a small sample size may have affected the statistical power of the study. Although our study included a large sample size we were unable to confirm this possibility and found no correlation between -308 TNF-α polymorphism and the risk of developing cervical cancer among the South African population. Similar reports were documented by others [9, 22, 33] and discordant with those previously reported in a population group from the United Kingdom [15]. In their study the authors demonstrated that the polymorphism in -308TNF-α gene significantly increased the susceptibility to cervical intraepithelial neoplasia 1 (CIN 1). However, as it is well-documented that most CIN1 regress spontaneously [34] it would have been beneficial if the authors extended the follow up screening to 36 months and thus the positive association demonstrated by the authors should be regarded with caution. In addition, CIN1 includes very mild to mild dysplasia, which is characterized by 20–25% replacement of the epithelium with immature cells and generally requires no treatment [29]. Furthermore, although in the same study the recruited subjects were age matched the authors did not provide the ethnic background for the population studied [15]. Thus, it is difficult to conclusively confirm or refute the possible ethnic disparity that may have contributed to the association differences observed between our study population and theirs.
Several reports in cervical cancer survival studies have indicated that the higher mortality rate in black populations is explained primarily by the more advanced clinical stage at time of diagnosis [35, 36]. It was found that the percentage of early diagnosis among blacks and Hispanics were significantly low for cervical and breast cancer compared to non-Hispanics whites. It was therefore suggested that screening programs should be managed differently for specific ethnic groups as there is a significant disparity in the outcome of disease between ethnic populations. [36]. Indeed, the high incidence of cervical cancer in certain population groups may be due to poor screening programs, a lack of stringent follow-up treatments and lower socioeconomic status in different population groups. In the present study, we compared our cervical cancer patient group with those from other populations (Table 2). Although there was a difference in the distribution of the GG and AG of TNF-α between our study and the Korean population, this result should be taken with caution as the sample size for the Korean population was very small. It would therefore be valuable if the samples size was increased to examine these relationships adequately. Nevertheless, 26% vs 6% is significant. Furthermore, we compared the distribution of our control study group to those of other populations to identifying whether the distribution of the TNF-α gene at position -308 is different in other healthy population groups (Table 3). The distribution of the AATNF-α, GGTNF-α and AGTNF-α genotypes at position -308 in the present control study group were similar to those observed in a Zimbabwean and Italian population and differed from those found in a Caucasian group. In addition, the distribution of the AGTNF-α genotype in the South African population group differed from that found in a Chinese and Korean population. These data highlight the possible variability of cytokine gene frequencies in different population groups and hence influence the disease outcome.
Conclusion
It is important to identify host or viral genetic markers that may facilitate the risk of developing cervical cancer. In addition, these markers would be useful in providing effective treatments and preventative strategies against HPV-induced infections. However, in this study we found no association between -308 TNF-α gene polymorphism and the risk of developing cervical cancer. Furthermore, our data highlight the need for further studies to clarify the association of ethnic variation and cytokine polymorphism as other potential confounding factors may contribute to the risk of developing cancer of the cervix.
References
zur Hausen H: Papillomaviruses causing cancer: evasion from host-cell host in early events in carcinogenesis. J Natl Cancer Inst. 2002, 92: 690-698. 10.1093/jnci/92.9.690.
Moscicki AB, Shiboski S, Broering J, Powell K, Clayton L, Jay N, Darragh TM, Brescia R, Kanowitz S, Miller SB, Stone J, Hanson E, Palefsky J: The natural history of human papillomavirus infection as measured by repeated DNA testing in adolescent and young women. J Pediatr. 1998, 132: 277-284. 10.1016/S0022-3476(98)70445-7.
Wu TC: Immunology of the human papillomavirus in relation to cancer. Curr Opin Immunol. 1994, 6: 746-754. 10.1016/0952-7915(94)90079-5.
Kadish AS, Ho GY, Burk RD, Wang Y, Romney SL, Ledwidge R, Angeletti RH: Lymphoproliferative responses to human papillomavirus (HPV) type 16 proteins E6 and E7: outcome of HPV infection and associated neoplasia. J Natl Cancer Inst. 1997, 89: 1285-1293. 10.1093/jnci/89.17.1285.
Clerici M, Merola M, Ferrario E, Trabattoni D, Villa Ml, Stefanon B, Venzon DJ, Shearer GM, De Palo G, Clerici E: Cytokine production patterns in cervical intraepithelial neoplasia: An association with human papillomavirus infection. J Natl Cancer Inst. 1997, 89: 245-250. 10.1093/jnci/89.3.245.
Govan VA, Carrara HRO, Sachs JA, Hoffman M, Stanczuk GA, Williamson AL: Ethnic differences in allelic distribution of IFN-g in South African women but no link with cervical cancer. J of Carcinogenesis. 2003, 2: 3-10.1186/1477-3163-2-3.
Wu MS, Huang SP, Chang YT, Shun CT, Chang MC, Lin MT, Wang HP, Lin JT: Tumor necrosis factor-alpha and interleukin-10 promoter polymorphisms in Epstein-Barr virus-associated gastric carcinoma. J Infect Dis. 2002, 185: 106-109. 10.1086/324771.
Shibata N, Ohnuma T, Takahashi T, Baba H, Ishizuka T, Ohtsuka M, Ueki A, Nagao M, Arai H: Effect of IL-6 polymorphism on risk of Alzheimer disease: Genotype-phenotype association study in Japanese cases. Am J Med Genet. 2002, 114: 436-439. 10.1002/ajmg.10417.
Calhoun ES, McGovern RM, Janney CA, Cerhan JR, Iturria SJ, Smith DI, Gostout BS, Persing DH: Host genetic polymorphism analysis in cervical cancer. Clin Chem. 2002, 48 (8): 1218-24.
Kroeger KM, Carville KS, Abraham LJ: The -308 tumor necrosis factor-alpha promoter polymorphism effects transcription. Mol Immunol. 1997, 34 (5): 391-9. 10.1016/S0161-5890(97)00052-7.
Carswell EA, Old LJ, Kassel RL, Green S, Fiore N, Williamson B: An endotoxin-induced serum factor that causes necrosis of tumors. Proc Natl Acad Sci. 1975, 72 (9): 3666-70.
Shishodia S, Majumdar S, Banerjee S, Aggarwal BB: Ursolic acid inhibits nuclear factor-κB activation induced by carcinogenic agents through suppression of IκBα kinase and p65 phosporylation: Correlation with down-regulation of cyclooxygenase 2, matrix metalloproteinase 9, and cyclin D1. Cancer Res. 2003, 63: 4375-4383.
Raabe T, Bukrinsky M, Currie RA: Relative contribution of transcription and translation to the induction of tumor necrosis factor-alpha by lipopolysaccharide. J Biol Chem. 1998, 273 (2): 974-80. 10.1074/jbc.273.2.974.
Jang WH, Yang YI, Yea SS, Lee YJ, Chun JH, Kim HI, Kim MS, Paik KH: The -238 tumor necrosis factor-alpha promoter polymorphism is associated with decreased susceptibility to cancers. Cancer Lett. 2001, 66 (1): 41-6. 10.1016/S0304-3835(01)00438-4.
Kirkpatrick A, Bidwell J, van den Brule AJ, Meijer CJ, Pawade J, Glew S: TNF alpha polymorphism frequencies in HPV-associated cervical dysplasia. Gynecol Oncol. 2004, 92 (2): 675-9. 10.1016/j.ygyno.2003.11.025.
Lee JY, Kim HY, Kim KH, Kim SM, Jang MK, Park JY, Kim JH, Yoo JY: Association of polymorphism of IL-10 and TNF-α genes with gastric cancer in Korea. Cancer Lett. 2005, 225 (2): 207-214. 10.1016/j.canlet.2004.11.028.
Azmy IA, Balasubramanian SP, Wilson AG, Stephenson TJ, Cox A, Brown NJ, Reed MW: Role of tumour necrosis factor gene polymorphisms (-308 and -238) in breast cancer susceptibility and severity. Breast Cancer Res. 2004, 6 (4): R395-400. 10.1186/bcr802.
Deshpande A, Nolan JP, White PS, Valdez YE, Hunt WC, Peyton CL, Wheeler CM: TNF-a promoter polymorphisms and susceptibility to human papillomavirus 16-associated cervical cancer. JID. 2005, 191: 969-976. 10.1086/427826.
Tjiong MY, van der Vange N, ter Schegget JS, Burger MPM, ten Kate FWJ, Out TA: Cytokines in cervicovaginal washing fluid from patients with cervical neoplasia. Cytokine. 2001, 14: 357-360. 10.1006/cyto.2001.0909.
Chen G, Wilson R, Wang SH, Zheng HZ, Walker JJ, McKillop JH: Tumor necrosis factor alpha (TNF-α) gene polymorphism and expression in pre-eclampsia. Clin Exp Immunol. 1996, 104: 154-159. 10.1046/j.1365-2249.1996.d01-647.x.
Stanczuk GA, Sibanda EN, Tswana SA, Bergstrom S: Polymorphism at the -308-promoter position of the tumor necrosis factor-alpha (TNF-alpha) gene and cervical cancer. Int J Gynecol Cancer. 2003, 13: 148-53. 10.1046/j.1525-1438.2003.13046.x.
Ghaderi M, Nikitina L, Peacock CS, Hjelmstrom P, Hallmans G, Wiklund F, Lenner P, Blackwell JM, Dillner J, Sanjeevi CB: Tumor necrosis factor a-11 and DR15-DQ6 (B*0602) haplotype increase the risk for cervical intraepithelial neoplasia in human papillomavirus 16 seropositive women in Northern Sweden. Epidemiol Biomarkers Prev. 2001, 9: 1067-1070.
Hoffman M, Cooper D, Carrara HRO, Rosenberg L, Kelly J, Stander I, Williamson A-L, De toit G, Shapiro S: Limited Pap screening associated with reduced risk of cervical cancer in South Africa. Int J Epidemiol. 2003, 32: 573-577. 10.1093/ije/dyg081.
Perrey C, Turner SJ, Pravica V, Howell WM, Hutchinson IV: ARMS-PCR methodologies to determine IL-10, TNK-alpha and TGF-beta-1 gene polymorphism. Transplant Immunol. 1999, 7: 127-128. 10.1016/S0966-3274(99)80030-6.
Lu W, Pan K, Zhang L, Lin D, Miao X, You W: Genetic polymorphisms of interleukin (IL)-1B, IL-1RN, IL-8, IL-10 and tumor necrosis factor {alpha} and risk of gastric cancer in a Chinese population. Carcinogenesis. 2005, 26 (3): 631-6. 10.1093/carcin/bgh349.
Perri F, Piepoli A, Bonvicini C, Gentile A, Quitadamo M, Di Candia M, Cotugno R, Cattaneo F, Zagari MR, Ricciardiello L, Gennarelli M, Bazzoli F, Ranzani GN, Andriulli A: Cytokine gene polymorphisms in gastric cancer patients from two Italian areas at high and low cancer prevalence. Cytokine. 2005, 30 (5): 293-302. 10.1016/j.cyto.2005.01.011.
Ferlay J, Bray F, Pisani P: GLOBOCAN 2002: cancer incidence, motality and prevalence worldwide. IARC Press. 2004
Robinson W: Management of cervical cancer neoplasia. Cancer Treat Res. 2001, 104: 287-302.
Brinkman JA, Caffrey AS, Muderspach I, Roman LD, Kast WM: The impact of anti HPV vaccination on cervical cancer incidence and HPV induced cervical cancer lesions: Consequences for clinical management. Eur J Oncol. 2005, 26: 129-142.
Govan VA: Strategies for Human Papillomavirus therapeutic vaccines and other therapies based on the E6 and E7 oncogenes. Annals NYA Sci. 2005 in press
Wacholder S: Chapter 18: Statistical Issues in the design and analysis of studies of human papillomavirus and cervical neoplasia. J Natl Cancer Inst Monogr. 2003, 31: 125-30.
Azar KK, Tani M, Yasuda H, Sakai A, Inoue M, Sasagawa T: Increased secretion patterns of interleukin-10 and tumor necrosis factor-alpha in cervical squamous intraepithelial lesions. Hum Pathol. 2004, 35 (11): 1376-84. 10.1016/j.humpath.2004.08.012.
Galloway DA: Papillomavirus vaccines in clinical trials. Lancet Infect Dis. 2003, 8: 469-75. 10.1016/S1473-3099(03)00720-5.
Gostout BS, Poland GA, Calhoun ES, Sohni YR, Giuntoli RL, McGovern RM, Sloan JA, Cha SS, Persing DH: TAP1, TAP2, and HLA-DR2 alleles are predictors of cervical cancer risk. Gynecol Oncol. 2003, 3: 326-32. 10.1016/S0090-8258(02)00074-4.
Shelton D, Paturzo D, Flannery J, Gregorio D: Race, stage of disease, and survival with cervical cancer. Ethn Dis. 1992, 2: 47-54.
Chen F, Trapido EJ, Davis K: Differences in stage at presentation of breast and gynecological cancers among whites, blacks, and Hispanics. Cancer. 1994, 73: 2838-2842.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/6/24/prepub
Acknowledgements
The United States National Cancer Institute supported the cancer case-control study (grant number 1 R01 C473985). We thank Shayne Loubsher for technical assistance. VAG was supported by FHS.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
VAG designed the study, carried out the study and drafted the manuscript. DC performed the statistical analysis for the study. MH participated in the design and coordination of the case control study. A-LW participated in the coordination of the study. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Govan, V.A., Constant, D., Hoffman, M. et al. The allelic distribution of -308 Tumor Necrosis Factor-alpha gene polymorphism in South African women with cervical cancer and control women. BMC Cancer 6, 24 (2006). https://doi.org/10.1186/1471-2407-6-24
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-6-24