Abstract
Background
Rash, liver dysfunction, and diarrhea are known major adverse events associated with erlotinib and gefitinib. However, clinical trials with gefitinib have reported different proportions of adverse events compared to trials with erlotinib. In an in vitro study, cytochrome P450 (CYP) 2D6 was shown to be involved in the metabolism of gefitinib but not erlotinib. It has been hypothesized that CYP2D6 phenotypes may be implicated in different adverse events associated with gefitinib and erlotinib therapies.
Methods
The frequency of each adverse event was evaluated during the period in which the patients received gefitinib or erlotinib therapy. CYP2D6 phenotypes were determined by analysis of CYP2D6 genotypes using real-time polymerase chain reaction techniques, which can detect single-nucleotide polymorphisms. The CYP2D6 phenotypes were categorized into 2 groups according to functional or reduced metabolic levels. In addition, we evaluated the odds ratio (OR) of the adverse events associated with each factor, including CYP2D6 activities and treatment types.
Results
A total of 232 patients received gefitinib therapy, and 86 received erlotinib therapy. Reduced function of CYP2D6 was associated with an increased risk of rash of grade 2 or more (OR, 0.44; 95% confidence interval [CI], 0.21–0.94; *p = 0.03), but not diarrhea ≥ grade 2 (OR, 0.49; 95% CI, 0.17–1.51; *p = 0.20) or liver dysfunction ≥ grade 2 (OR, 1.08; 95% CI, 0.52–2.34; *p = 0.84) in the gefitinib cohort. No associations were observed between any adverse events in the erlotinib cohort and CYP2D6 phenotypes (rash: OR, 1.77; 95% CI, 0.54–6.41; *p = 0.35/diarrhea: OR, 1.08; 95% CI, 0.21–7.43; *p = 0.93/liver dysfunction: OR, 0.93; 95% CI, 0.20–5.07; *p = 0.93).
Conclusions
The frequency of rash was significantly higher in patients with reduced CYP2D6 activity who treated with gefitinib compared to patients with functional CYP2D6. CYP2D6 phenotypes are a risk factor for the development of rash in response to gefitinib therapy.
Similar content being viewed by others
Background
Compared to cytotoxic agents, gefitinib and erlotinib are orally available epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKI) that prolong survival, have few hematological adverse events, and improve the quality of life in non-small cell lung cancer (NSCLC) patients with EGFR-active gene mutations [1–6]. The major adverse events that occur with gefitinib and erlotinib therapy are rash, liver dysfunction and diarrhea [1–5, 7–10]. We are always faced with a decision to select between these drugs in clinical practice for patients with EGFR-active mutations. In general, erlotinib is associated with higher toxicity and lower tolerability than gefitinib because the dose of erlotinib used is nearly equal to the maximum tolerated dose, whereas the dose of gefitinib used is close to the minimum active dose [11, 12].
Recent in vitro studies have reported different metabolic profiles of gefitinib and erlotinib for human cytochrome P450 (CYP) enzymes [13–15]. CYP3A4, CYP3A5, and CYP1A1 metabolize both erlotinib and gefitinib. However, CYP2D6 is involved in the metabolism of gefitinib but not erlotinib. It has been hypothesized that gefitinib therapy results in different adverse events compared to erlotinib therapy due to the CYP2D6 phenotype. To test this, we evaluated the adverse events of treatment with gefitinib and erlotinib. CYP2D6 phenotypes were determined from the CYP2D6 genotypes using real-time polymerase chain reaction (PCR) techniques, which are able to detect single-nucleotide polymorphisms (SNPs).
Methods
Study subjects and data collection
Patients with advanced NSCLC who were treated with either gefitinib or erlotinib were retrospectively identified by analysis of patient information for subjects prospectively enrolled in the Medical Information System within Osaka City University Hospital between January 1999 and February 2012. This study protocol was approved by the ethics committee of Osaka City University (approval number, 1700). In our study, all patients received a single agent EGFR-TKI therapy. The frequency of each adverse event was evaluated during the period in which the patients received EGFR-TKI therapy. All living participants provided written informed consent. Formalin-fixed and paraffin-embedded tissues or blood samples (when tissues were not available) were collected. If the patients were dead, formalin-fixed and paraffin-embedded tissues were collected with the permission of the ethics committee. Adverse events were assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events (version 3.0). We defined liver dysfunction as one or more events of increased levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), or blood bilirubin. The frequency and severity of 3 major non-hematological toxicities, including rash, diarrhea, and liver dysfunction, were evaluated.
Genotyping methods
Genomic DNA was extracted from peripheral blood or formalin-fixed and paraffin-embedded (FFPE) tissues using a QIAGEN QIAamp® DNA Blood Mini Kit (QIAGEN K.K., Tokyo, Japan) and a QIAGEN QIAamp® DNA FFPE Tissue Kit (QIAGEN K.K.), according to the manufacturer’s instructions. Extracted DNA samples were stored at −80°C before use. The DNA concentration was determined by measuring the optical density at 260 nm (Nano Drop® ND-1000, Thermo Fisher Scientific, Inc., Wilmington, DE, USA). In order to determine the CYP2D6 polymorphisms, 4 SNPs of the CYP2D6 gene, including rs1065852 (100C>T), rs5030865 (1758 G>A), rs16947 (2850C>T), and rs1135840 (4180 G>C), were measured by real-time PCR in order to evaluate the 5 mutated alleles: CYP2D6*1, CYP2D6*2, CYP2D6*10, CYP2D6*14A, and CYP2D6*14B. Genotyping was performed using Taqman® Drug Metabolism Genotyping Assays™ (Applied Biosystems Japan Ltd., Tokyo, Japan), according to the manufacturer’s instructions. The following reagents were used for amplification in a 10 μL reaction volume: 4.5 μL of DNA (around 50 ng), 0.5 μL of each CYP2D6 primer and probe mixture (20×), and 5 μL of GTXexpress™ Master Mix. The thermal cycling conditions consisted of an initial 20 seconds at 95°C, followed by 40 cycles at 95°C for 15 seconds and at 60°C for 1 minute. Primers and probes were supplied by Applied Biosystems, Japan, Ltd as Drug Metabolism Genotyping Assays™. The assay IDs were C__11484460_40 for rs1065852, C_30634117D_30 for rs5030865, C__27102425_10 for rs16947, and C__27102414_10 for rs1135840. All assays were performed in 96-well plates. Plates were read on an Applied Biosystems 7500 Real-time PCR system using the Sequence Detection System Software (Applied Biosystems Japan Ltd.).
CYP2D6 phenotype
The metabolic functions of CYP2D6 are generally categorized into 4 groups: ultra-rapid metabolizer (UM), extensive metabolizer (EM), intermediate metabolizer (IM), and poor metabolizer (PM) [16]. UM and EM result in normal or better function, and IM and PM result in reduced functions. CYP2D6 alleles were assigned based on the determination of the appropriate key mutations. CYP2D6*1 and CYP2D6*2 have normal activities, CYP2D6*10 and CYP2D6*14B have impaired activities, and CYP2D6*5 and CYP2D6*14A have no activities [17–20]. Alleles containing additional copies of functional CYP2D6 genes were categorized as UM. The EM included a combination of 1 or 2 functional alleles, such as CYP2D6*1 or CYP2D6*2, the IM phenotype included 2 impaired alleles, and the PM phenotype included two non-functional alleles. In this study, the CYP2D6 phenotype was categorized into 2 groups according to the metabolic levels: functional (UM and EM) or reduced groups (IM and PM). Unknown phenotypes with a combination of impaired and undetermined alleles, or 2 undetermined alleles, were excluded.
Statistical analysis
Comparisons of the characteristics between patients treated with gefitinib or erlotinib were performed using Fisher’s exact tests. Hardy-Weinberg equilibrium was tested for with a goodness-of-fit χ2-test with 2 degree of freedom to compare the observed genotype frequencies among the subjects with the expected genotype frequencies. In order to identify the risk factors for the adverse events, gender, age, CYP2D6 activity, and stage were selected and estimated for their potential confounding effects on rash, diarrhea, and liver dysfunction by multivariate analysis. Unconditional logistic regressions were used to compute the odds ratios (ORs) and their 95% confidence intervals (CIs). All analyses were two-sided, and p values of less than 0.05 were considered statistically significant. The statistical analyses were performed with JMP 9 software (SAS Institute, Inc., Cary, NC, USA) and software R version 2.10.0 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
The study profile is illustrated in Figure 1. A total of 256 patients with advanced NSCLC who were treated with gefitinib, and a total of 94 patients with advanced NSCLC who were treated with erlotinib, were enrolled in the study. DNA samples were collected from 289 patients, including 232 patients who received gefitinib and 86 patients who received erlotinib. Among them, 29 patients who were treated with gefitinib were also treated with erlotinib at different times. DNA samples were not obtained from 24 patients who were treated with gefitinib and 8 patients who were treated with erlotinib because of screen failure. Genomic DNA was extracted from 232 samples, including 16 blood samples and 216 tissues, in the gefitinib group, and from 86 samples, including 15 blood samples and 71 tissues, in the erlotinib group.
The distributions of the patient characteristics among the study subjects are summarized in Table 1. Comparisons of the gefitinib and erlotinib groups that were representative of the cohort indicated that the gefitinib group had a higher rate of EGFR mutation-positive patients (gefitinib group, 95.6%; erlotinib group, 70.6%; *p < 0.001), and a higher rate of poor performance status (≥2) patients (gefitinib group, 25.4%; erlotinib group, 8.2%; *p = 0.001). There were no significant differences between the gefitinib and erlotinib groups in terms of age, sex ratio, histology, smoking status, stages, CYP2D6 functions, infection with the hepatitis B or C virus, or pretreatment liver function tests.
Comparison of the adverse events of gefitinib and erlotinib
Figure 2 shows the frequencies and severities of rash, diarrhea, and liver dysfunction. In the gefitinib treatment group, the rates of rash of all grades and of grade 2 or greater were 66.8% and 19.8%, those of diarrhea were 25.9% and 9.1%, and those of liver dysfunction were 48.3% and 25.0%, respectively. In the erlotinib treatment group, the rates of rash of all grades and of grade 2 or greater were 83.7% and 46.5%, those of diarrhea were 43.0% and 16.3%, and those of liver dysfunction were 33.7% and 17.4%, respectively. The patients treated with gefitinib had a significantly higher frequency of liver dysfunction than the patients treated with erlotinib (*p = 0.02). In contrast, the patients treated with erlotinib had a significantly higher frequency of rash and diarrhea than did the patients treated with gefitinib (*p = 0.003 and 0.04, respectively). Sixteen pneumonitis patients were observed only in the gefitinib group, and pneumonitis-related death was observed in 7 patients.
Comparison of adverse events between the gefitinib and erlotinib groups. The graphs show the proportion of adverse events in all grade (A), and in grade ≥ 2 (B). In all grade, the patients treated with gefitinib had a significantly higher frequency of liver dysfunction than did patients treated with erlotinib (*p = 0.003). In grade ≥ 2, liver dysfunction occurred significantly more often in the gefitinib group than in the erlotinib group (*p = 0.04).
CYP2D6alleles, genotype, and phenotype
The genomic DNA from a total of 289 patients was analyzed (Table 2). The distributions of CYP2D6 alleles were as follows: CYP2D6*1, 236 alleles (40.8%); CYP2D6*2, 63 alleles (10.9%); CYP2D6*10, 211 alleles (36.5%); CYP2D6*14A, 1 allele (0.2%); and undetermined, 67 alleles (11.6%). In a total of 201 patients, genotyping predicted the normal function of CYP2D6*1/*1 in 67 patients, CYP2D6*1/*2 in 22 patients, CYP2D6*1/*10 in 72 patients, CYP2D6*1/*14A in 1 patient, CYP2D6*1/undetermined allele in 7 patients, CYP2D6*2/*2 in 9 patients, CYP2D6*2/*10 in 20 patients, and CYP2D6*2/undetermined allele in 3 patients. In a total of 58 patients, genotyping predicted reduced function associated with CYP2D6*10/*10. In a total of 30 patients, the genotypes was unknown with results of CYP2D6*10/ undermined allele in 3 patients, and 2 undermined alleles in 27 patients. The frequencies of CYP2D6*1, CYP2D6*2, and CYP2D6*10 were compared to the data previously reported in Japanese [21–23]. Compared to the Kubota’s, Nishida’s, and Tateishi’s reports, the genotype distributions of each phenotype among the patients were in Hardy-Weinberg equilibrium (*p = 0.69, 0.92, and 0.63, respectively).
Comparison of adverse events among CYP2D6 phenotypes
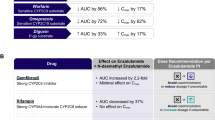
Figure 3 shows forest plots of the odds ratio for risk factors determined by multiple logistic regression models. Each adverse event was divided into 2 groups: grade 0, 1 or grade ≥ 2. In the gefitinib cohort, the genotypes of 156 patients predicted normal function, and the genotypes of 50 patients predicted reduced function. Reduced function was associated with an increased risk of rash (rash: OR, 0.44; 95% CI, 0.21–094; *p = 0.03). Reduced function was not associated with an increased risk of diarrhea or liver dysfunction (diarrhea: OR, 0.49; 95% CI, 0.17–1.51; *p = 0.20, liver dysfunction: OR, 1.08, 95% CI, 0.52–2.34; *p = 0.84).
The odds ratio of each adverse event in EGFR-TKIs. The graphs show the forest plots for gefitinib (A), and for erlotinib (B). In the gefitinib cohort, reduced function was associated with an increased risk of rash (*p = 0.03). In the erlotinib cohort, there were no associations between any adverse events and CYP2D6 phenotypes.
In the erlotinib cohort, the genotypes of 64 patients predicted normal function, and the genotypes of 16 patients predicted reduced function. There were no associations between any adverse events and CYP2D6 phenotypes (rash: OR, 1.77; 95% CI, 0.54–6.41; *p = 0.35, diarrhea: OR, 1.08; 95% CI, 0.21–7.43; *p = 0.93, liver dysfunction: OR, 0.93; 95% CI, 0.20–5.07; *p = 0.93).
Discussion
We have demonstrated that reduced function of CYP2D6 in the gefitinib cohort was associated with an increased risk of rash of grade 2 or more. No associations were observed in the erlotinib cohort between any adverse events and CYP2D6 phenotypes.
Almost all patients received appropriate supportive care in their treatment. In our study, gefitinib treatment showed different characteristics to erlotinib treatment. In a previous report without patient selection, treatment with gefitinib was not associated with a significant improvement in survival compared to placebo therapy [4, 5]. However, erlotinib has been shown to prolong survival in unselected and EGFR wild-type patients with NSCLC after first-line or second-line chemotherapy [6, 24]. For these reasons, gefitinib is administered to EGFR mutation-positive patients and patients with a higher rate of poor performance status (≥2).
In our study, gefitinib treatment showed different adverse events to erlotinib treatment. Compared to the side effects of erlotinib, patients treated with gefitinib had a significantly higher frequency of liver dysfunction. In the gefitinib group, the rate of liver dysfunction of all grades in our study was 45.3%, including 19.0% of grade 1, 10.5% of grade 2, 14.7% of grade 3, and 1.1% of grade 4. In the erlotinib group, the rate of liver dysfunction in our study was 21.3%, including 8.2% of grade 1, 8.2% of grade 2, 4.9% of grade 3, and 0% of grade 4. With respect to gefitinib therapy, Maemondo et al. reported a rate of 55% of all grades of increased levels of aminotransferases, and the rate of grade 3 or 4 was 21.5% in a Japanese cohort [2]. Mitsudomi et al. reported a rate of 70.1% of all grades and a rate of 16.1% of grade 3 or 4 [25]. With respect to erlotinib therapy, an Asian phase III study showed a rate of 37% for all grades of increased levels of ALT, and a rate of 4% of grade 3 or 4 [26]. Our results were similar to those found in previous gefitinib and erlotinib phase III clinical trials in Asian subjects.
Liver dysfunctions induced by gefitinib were reported in a few cases in which hepatotoxicity caused by gefitinib declined when gefitinib was changed to erlotinib. First, Kijima et al. suggested the possibility that CYP2D6 polymorphisms were related to gefitinib-induced hepatotoxicity. Their study described 3 cases with gefitinib-related hepatotoxicity whose genotypes were CYP2D6*1/*10, CYP2D6*10/*10, and CYP2D6*1/*5, with phenotypes of EM, IM and EM, respectively. Second, Takeda et al. reported a case and suggested that liver dysfunction was attributable to a gefitinib allergy on the basis of a positive drug lymphocyte stimulation test (DLST) [27]. In our study, the reduced function of CYP2D6 was not associated with an increased risk of liver dysfunction in the gefitinib cohort. Further analysis of the different metabolic profiles of CYP enzymes should be performed to clarify the metabolisms of gefitinib. The DLST of gefitinib may be considered of value in some patients with gefitinib-induced liver dysfunction.
The in vitro metabolism of gefitinib was investigated using human liver microsomes, and gefitinib metabolized mainly by expressed CYP3A4 produced a similar range of metabolites as liver microsomes [15]. When CYP3A4 function was low or inhibited by other drugs that inhibit CYP3A4, gefitinib metabolism that involves the formation of O-desmethyl-gefitinib and is determined by the CYP2D6 enzyme expressed in the liver was increased marginally [15]. Therefore, the CYP2D6 enzyme is important for the metabolism of gefitinib not only in patients with reduced CYP2D6 function, but also in patients with normal CYP2D6 function who take other drugs related to CYP3A4 inhibition. These patients treated with gefitinib may have severe skin rash due to decreased metabolism of gefitinib.
We evaluated 5 mutated alleles, CYP2D6*1, CYP2D6*2, CYP2D6*10, CYP2D6*14A and CYP2D6*14B, in 289 patients. The frequency of each allele was similar to those reported in previous Japanese studies. Two reports showed that the frequencies of the CYP2D6*1, CYP2D6*2, CYP2D6*5, CYP2D6*10, and CYP2D6*14 alleles were 40.1%, 12.9%, 6.2%, 38.6%, and 2.2%, respectively, in 162 Japanese [21], and 43%, 12.3%, 4.5%, 38.1%, and 0.7%, respectively, in 412 Japanese [22]. A further report showed that the frequencies of the CYP2D6*1, CYP2D6*2, CYP2D6*5, and CYP2D6*10 alleles were 42.3%, 9.2%, 6.1%, and 40.8%, respectively, in 98 healthy Japanese [23]. Taken together, the average frequencies of the functional and reduced function alleles in these studies were 54.2%, and 44.7%, respectively. Asians have a high frequency of the reduced function alleles that ranges from 43% to 47% [21–23, 28]. However, in Caucasians, the functional and reduced function alleles represented a median frequency of 71% and 26%, respectively, in all cohort studies [16] and 68.8% and 25.36%, respectively, in German subjects [29]. Thus, Asians have a higher frequency of reduced function alleles than do Caucasians. In addition, population-related pharmacogenomics revealed a significant difference between Japanese and US patients in genomic distribution and genotype-related associations with patient outcomes for CYP3A4*1B and ERCC2[30]. These facts may explain the frequency differences of adverse events, particularly rash, that are based on race.
CYP2D6 metabolizes many clinically important drugs, including antidepressants, neuroleptics, beta-blockers, anti-arrhythmics, and anti-cancer agents. In breast cancer patients who were treated with tamoxifen, the CYP2D6 phenotype was associated with survival [31] and the concentration of the active tamoxifen metabolite, endoxifen [32]. Recently, in 2 single-agent studies with gefitinib in bronchioloalveolar and head and neck carcinomas, an association between the occurrence of skin toxicity and survival was found [33, 34]. In our study, the subjects with reduced CYP2D6 function were associated with an increased risk of rash in the gefitinib cohort. Reduced CYP2D6 function may relate to longer overall survival as well as poor metabolism of gefitinib. A prospective large clinical trial is warranted to clarify these relationships.
Our findings had some limitations. The number of patients was too small to have sufficient power to detect significant differences in other adverse events between CYP2D6 phenotypes. This study was a retrospective analysis. The identification of adverse effects was prompted by monthly visits with hematological tests or a medical interview for onset of symptoms, although the hematological toxicities were in some cases diminished at the time of next visit because of self-judgment for discontinuation. The adverse events were generally controlled, except for interstitial lung disease. The relation between CYP2D6 and carcinogenic risk was not evaluated. The blood concentrations of gefitinib and erlotinib and the metabolites of gefitinib and erlotinib, were not measured. However, in clinical settings, it may be difficult to perform blood sampling at sufficient frequency to calculate area under the curve (AUC). We could not separate the UM cohort from the EM cohort. UM consists of CYP2D6*1 or CYP2D6*2, and this group was included with EM in this study. Other cytochrome P450 enzymes were not measured. The relationship between these concentrations and these enzyme phenotypes remain to be elucidated. Our study may provide useful information regarding drug selection for EGFR-TKIs. When gefitinib is administered in combination with drugs which inhibit CYP2D6 function, the frequency of severe rash by gefitinib may be increased. When the patients with unknown CYP2D6 phenotype, have a severe rash by gefitinib, the change of gefitinib to erlotinib may be sometimes useful, because the patient may have reduced CYP2D6 function and CYP2D6 is not affected the erlotinib metabolism. CYP2D6 genotyping and an understanding of CYP2D6 function may be helpful in predicting rash during gefitinib therapy.
Conclusions
We conclude that patients with reduced CYP2D6 activity treated with gefitinib had a significantly higher frequency of rash than did patients with functional CYP2D6. CYP2D6 phenotypes are a risk factor for the development of rash in gefitinib therapy. In contrast, no associations were found between the toxicity of liver dysfunction and CYP2D6 activity in patients treated with gefitinib. In our knowledge, our study is the first report that CYP2D6 phenotypes are related to severity of rash by gefitinib. Further clinical studies that include prospective investigations in a large patient population with pharmacokinetics/pharmacodynamics analyses, and that include detailed information regarding CYP2D6 genotype, phenotype and activity, should be conducted.
References
Kim E, Hirsh V, Mok T, Socinski M, Gervais R, Wu Y, Li L, Watkins C, Sellers M, Lowe E, et al: Gefitinib versus docetaxel in previously treated non-small-cell lung cancer (INTEREST): a randomised phase III trial. Lancet. 2008, 372 (9652): 1809-1818. 10.1016/S0140-6736(08)61758-4.
Maemondo M, Inoue A, Kobayashi K, Sugawara S, Oizumi S, Isobe H, Gemma A, Harada M, Yoshizawa H, Kinoshita I, et al: Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010, 362 (25): 2380-2388. 10.1056/NEJMoa0909530.
Maruyama R, Nishiwaki Y, Tamura T, Yamamoto N, Tsuboi M, Nakagawa K, Shinkai T, Negoro S, Imamura F, Eguchi K, et al: Phase III study, V-15-32, of gefitinib versus docetaxel in previously treated Japanese patients with non-small-cell lung cancer. J Clin Oncol. 2008, 26 (26): 4244-4252. 10.1200/JCO.2007.15.0185.
Mok T, Wu Y, Thongprasert S, Yang C, Chu D, Saijo N, Sunpaweravong P, Han B, Margono B, Ichinose Y, et al: Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009, 361 (10): 947-957. 10.1056/NEJMoa0810699.
Thatcher N, Chang A, Parikh P, Rodrigues Pereira J, Ciuleanu T, von Pawel J, Thongprasert S, Tan E, Pemberton K, Archer V, et al: Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet. 2005, 366 (9496): 1527-1537. 10.1016/S0140-6736(05)67625-8.
Shepherd F, Rodrigues Pereira J, Ciuleanu T, Tan E, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S, Smylie M, Martins R, et al: Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005, 353 (2): 123-132. 10.1056/NEJMoa050753.
Hotta K, Kiura K, Takigawa N, Yoshioka H, Harita S, Kuyama S, Yonei T, Fujiwara K, Maeda T, Aoe K, et al: Comparison of the incidence and pattern of interstitial lung disease during erlotinib and gefitinib treatment in Japanese Patients with non-small cell lung cancer: the Okayama Lung Cancer Study Group experience. J Thorac Oncol. 2010, 5 (2): 179-184. 10.1097/JTO.0b013e3181ca12e0.
Lee JH, Jo YR, Park HS, Ryu YJ, Chun EM, Chang JH: Comparison of gefitinib and erlotinib for Korean patients with advanced non-small cell lung cancer. J Thorac Oncol. 2009, 4 (9): S692-
Togashi Y, Masago K, Fujita S, Hatachi Y, Fukuhara A, Nagai H, Sakamori Y, Kim YH, Mio T, Mishima M: Differences in adverse events between 250 mg daily gefitinib and 150 mg daily erlotinib in Japanese patients with non-small cell lung cancer. Lung Cancer. 2011, 74 (1): 98-102. 10.1016/j.lungcan.2011.01.022.
Uhm JE, Sun JM, Lee SH, Kong JH, Yun JA, Lee SM, Lee J, Park YH, Ahn JS, Park K, et al: Comparison of erlotinib (Tarceva (TM)) versus gefitinib (Iressa (R)) as the second line therapy for the treatment of advanced non-small cell lung cancer patients: a randomized phase II trial. J Thorac Oncol. 2009, 4 (9): S292-
Hidalgo M, Siu LL, Nemunaitis J, Rizzo J, Hammond LA, Takimoto C, Eckhardt SG, Tolcher A, Britten CD, Denis L, et al: Phase I and pharmacologic study of OSI-774, an epidermal growth factor receptor tyrosine kinase inhibitor, in patients with advanced solid malignancies. J Clin Oncol. 2001, 19 (13): 3267-3279.
Baselga J, Rischin D, Ranson M, Calvert H, Raymond E, Kieback DG, Kaye SB, Gianni L, Harris A, Bjork T, et al: Phase I safety, pharmacokinetic, and pharmacodynamic trial of ZD1839, a selective oral epidermal growth factor receptor tyrosine kinase inhibitor, in patients with five selected solid tumor types. J Clin Oncol. 2002, 20 (21): 4292-4302. 10.1200/JCO.2002.03.100.
Kijima T, Shimizu T, Nonen S, Furukawa M, Otani Y, Minami T, Takahashi R, Hirata H, Nagatomo I, Takeda Y, et al: Safe and successful treatment with erlotinib after gefitinib-induced hepatotoxicity: difference in metabolism as a possible mechanism. J Clin Oncol. 2011, 29 (19): E588-E590. 10.1200/JCO.2010.34.3368.
Li J, Zhao M, He P, Hidalgo M, Baker SD: Differential metabolism of gefitinib and erlotinib by human cytochrome P450 enzymes. Clin Cancer Res. 2007, 13 (12): 3731-3737. 10.1158/1078-0432.CCR-07-0088.
McKillop D, McCormick A, Millar A, Miles G, Phillips P, Hutchison M: Cytochrome P450-dependent metabolism of gefitinib. Xenobiotica. 2005, 35 (1): 39-50. 10.1080/00498250400026464.
Bradford LD: CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics. 2002, 3 (2): 229-243. 10.1517/14622416.3.2.229.
Gaedigk A, Blum M, Gaedigk R, Eichelbaum M, Meyer UA: Deletion of the entire cytochrome P450 CYP2D6 gene as a cause of impaired drug metabolism in poor metabolizers of the debrisoquine/sparteine polymorphism. Am J Hum Genet. 1991, 48 (5): 943-950.
Johansson I, Lundqvist E, Bertilsson L, Dahl ML, Sjöqvist F, Ingelman-Sundberg M: Inherited amplification of an active gene in the cytochrome P450 CYP2D locus as a cause of ultrarapid metabolism of debrisoquine. Proc Natl Acad Sci U S A. 1993, 90 (24): 11825-11829. 10.1073/pnas.90.24.11825.
Kimura S, Umeno M, Skoda RC, Meyer UA, Gonzalez FJ: The human debrisoquine 4-hydroxylase (CYP2D) locus: sequence and identification of the polymorphic CYP2D6 gene, a related gene, and a pseudogene. Am J Hum Genet. 1989, 45 (6): 889-904.
Sakuyama K, Sasaki T, Ujiie S, Obata K, Mizugaki M, Ishikawa M, Hiratsuka M: Functional characterization of 17 CYP2D6 allelic variants (CYP2D6.2, 10, 14A-B, 18, 27, 36, 39, 47–51, 53–55, and 57). Drug Metab Dispos. 2008, 36 (12): 2460-2467. 10.1124/dmd.108.023242.
Kubota T, Yamaura Y, Ohkawa N, Hara H, Chiba K: Frequencies of CYP2D6 mutant alleles in a normal Japanese population and metabolic activity of dextromethorphan O-demethylation in different CYP2D6 genotypes. Br J Clin Pharmacol. 2000, 50 (1): 31-34.
Nishida Y, Fukuda T, Yamamoto I, Azuma J: CYP2D6 genotypes in a Japanese population: low frequencies of CYP2D6 gene duplication but high frequency of CYP2D6*10. Pharmacogenetics. 2000, 10 (6): 567-570. 10.1097/00008571-200008000-00010.
Tateishi T, Chida M, Ariyoshi N, Mizorogi Y, Kamataki T, Kobayashi S: Analysis of the CYP2D6 gene in relation to dextromethorphan O-demethylation capacity in a Japanese population. Clin Pharmacol Ther. 1999, 65 (5): 570-575. 10.1016/S0009-9236(99)70077-9.
Zhu CQ, da Cunha Santos G, Ding K, Sakurada A, Cutz JC, Liu N, Zhang T, Marrano P, Whitehead M, Squire JA, et al: Role of KRAS and EGFR as biomarkers of response to erlotinib in National Cancer Institute of Canada Clinical Trials Group Study BR.21. J Clin Oncol. 2008, 26 (26): 4268-4275. 10.1200/JCO.2007.14.8924.
Mitsudomi T, Morita S, Yatabe Y, Negoro S, Okamoto I, Tsurutani J, Seto T, Satouchi M, Tada H, Hirashima T, et al: Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010, 11 (2): 121-128. 10.1016/S1470-2045(09)70364-X.
Zhou C, Wu YL, Chen G, Feng J, Liu XQ, Wang C, Zhang S, Wang J, Zhou S, Ren S, et al: Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011, 12 (8): 735-742. 10.1016/S1470-2045(11)70184-X.
Takeda M, Okamoto I, Fukuoka M, Nakagawa K: Successful Treatment With Erlotinib After Gefitinib-Related Severe Hepatotoxicity. J Clin Oncol. 2010, 28 (17): E273-E274. 10.1200/JCO.2009.26.5496.
Johansson I, Oscarson M, Yue QY, Bertilsson L, Sjöqvist F, Ingelman-Sundberg M: Genetic analysis of the Chinese cytochrome P4502D locus: characterization of variant CYP2D6 genes present in subjects with diminished capacity for debrisoquine hydroxylation. Mol Pharmacol. 1994, 46 (3): 452-459.
Sachse C, Brockmoller J, Bauer S, Roots I: Cytochrome P450 2D6 variants in a Caucasian population: allele frequencies and phenotypic consequences. Am J Hum Genet. 1997, 60 (2): 284-295.
Gandara DR, Kawaguchi T, Crowley J, Moon J, Furuse K, Kawahara M, Teramukai S, Ohe Y, Kubota K, Williamson SK, et al: Japanese-US common-arm analysis of paclitaxel plus carboplatin in advanced non-small-cell lung cancer: a model for assessing population-related pharmacogenomics. J Clin Oncol. 2009, 27 (21): 3540-3546. 10.1200/JCO.2008.20.8793.
Abraham JE, Maranian MJ, Driver KE, Platte R, Kalmyrzaev B, Baynes C, Luccarini C, Shah M, Ingle S, Greenberg D, et al: CYP2D6 gene variants: association with breast cancer specific survival in a cohort of breast cancer patients from the United Kingdom treated with adjuvant tamoxifen. Breast Cancer Res. 2010, 12 (4): R64-10.1186/bcr2629.
Irvin WJ, Walko CM, Weck KE, Ibrahim JG, Chiu WK, Dees EC, Moore SG, Olajide OA, Graham ML, Canale ST, et al: Genotype-guided tamoxifen dosing increases active metabolite exposure in women with reduced CYP2D6 metabolism: a multicenter study. J Clin Oncol. 2011, 29 (24): 3232-3239. 10.1200/JCO.2010.31.4427.
Cohen EE, Kane MA, List MA, Brockstein BE, Mehrotra B, Huo D, Mauer AM, Pierce C, Dekker A, Vokes EE: Phase II trial of gefitinib 250 mg daily in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck. Clin Cancer Res. 2005, 11 (23): 8418-8424. 10.1158/1078-0432.CCR-05-1247.
West HL, Franklin WA, McCoy J, Gumerlock PH, Vance R, Lau DH, Chansky K, Crowley JJ, Gandara DR: Gefitinib therapy in advanced bronchioloalveolar carcinoma: Southwest Oncology Group Study S0126. J Clin Oncol. 2006, 24 (12): 1807-1813. 10.1200/JCO.2005.04.9890.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/12/568/prepub
Acknowledgements
This research was partially supported by a Grant-in-Aid for Young Scientists (B), the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors have made no disclosures.
Authors’ contributions
TS and TK conceived of the study, participated in the design of the study, acquisition of data, performed the statistical analysis, drafted and revising the manuscript. SK conceived of the study, participated in the design of the study, acquisition of data and revising the manuscript. KU, MN, MK, HT, SM, NY, NT were involved in acquisition of data. YK carried out real-time PCR methods. KH participated in the design of the study, acquisition of data and revising the manuscript. All authors have read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Suzumura, T., Kimura, T., Kudoh, S. et al. Reduced CYP2D6 function is associated with gefitinib-induced rash in patients with non-small cell lung cancer. BMC Cancer 12, 568 (2012). https://doi.org/10.1186/1471-2407-12-568
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-12-568