Abstract
Background
Caudal regression is a rare syndrome which has a spectrum of congenital malformations ranging from simple anal atresia to absence of sacral, lumbar and possibly lower thoracic vertebrae, to the most severe form which is known as sirenomelia. Maternal diabetes, genetic predisposition and vascular hypoperfusion have been suggested as possible causative factors.
Case presentation
We report a case of caudal regression syndrome diagnosed in utero at 22 weeks' of gestation. Prenatal ultrasound examination revealed a sudden interruption of the spine and "frog-like" position of lower limbs. Termination of pregnancy and autopsy findings confirmed the diagnosis.
Conclusion
Prenatal ultrasonographic diagnosis of caudal regression syndrome is possible at 22 weeks' of gestation by ultrasound examination.
Similar content being viewed by others
Background
Caudal regression syndrome represents a spectrum congenital malformations ranging from agenesis of the lumbosacral spine to the most severe cases of sirenomelia with lower extremity fusion and major vessel anomalies. The etiology of this syndrome is not well-known. Maternal diabetes, genetic predisposition and vascular hypoperfusion have been suggested as possible causative factors [1].
Case presentation
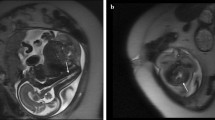
A 16-year-old primigravid woman, was first seen at 22 weeks' of gestation at the perinatology clinic of SSK Bakirkoy Maternity and Children Hospital. Her medical history was unremarkable. She has a positive 100 gr oral glucose tolerance test and her glycosylated hemoglobin (HbA1C) was 5.71 per cent on presentation. Ultrasonographic examination showed a singleton fetus with normal amniotic fluid volume. Fetal biometry was consistent with dates. A detailed examination of fetal anatomy revealed a sudden termination of spine at lumbal level and fixed lower extremities with club feet (Figure 1,2).
These findings were strongly suggestive of the caudal regression syndrome. The patient was counseled accordingly and she elected for termination of pregnancy. She delivered a 700 gr male infant without any complication. Autopsy examination confirmed the prenatal diagnosis of lumbosacral agenesis, flexion contractures of the lower extremities with extensive popliteal webbing in "frog-like" position and club feet. Heart examination showed a ventricular septal defect. Postpartum radiologic examination showed missing ribs, absent lumbosacral vertebrae and a hypoplastic pelvis (Figure 3).
Caudal regression syndrome is an uncommon malformation in the general population, but occurs in about one in 350 infants of diabetic mothers, representing an increase of about 200-fold over the rate seen in the general population [2]. Whereas sacral agenesis is estimated to occur in 0.3 to 1 percent of infants born to pregestational and gestational diabetic mothers, only 8 to 16 percent of infants with the syndrome were delivered to these patients [3].
The embryologic insult occurs at the midposterior axis mesoderm and the lesion originates before the fourth weeks of gestation but the etiology of caudal regression syndrome remains unclear [4]. Recent advances in the understanding of axial mesoderm patterning during early embryonic development suggest that sirenomelia represents the most severe end of the caudal regression spectrum [5].
Detailed evaluation of the fetal spine and lower extremities is an important aspect of every prenatal ultrasound examination. Sacral agenesis is a less severe variant of caudal regression syndrome and in the presence of normal amniotic fluid, the diagnosis can be made by demonstrating the termination of lumbar spine and small and abnormal lower extremities [6]. Both findings were present in this case. In sirenomelia third-trimester ultrasonographic diagnosis is usually impaired by severe oligohydramnios related to bilateral renal agenesis, whereas during the early second trimester the amount of amniotic fluid may be sufficient to allow diagnosis. Early antenatal sonographic diagnosis is important in view of the dismal prognosis, and allows for earlier, less traumatic termination of pregnancy [5].
Sacral and/or lumbosacral agenesis has been well described. However, especially as far as MRI studies are concerned, thoraco-lumbosacral agenesis has rarely been reported [7].
Amnioinfusion and magnetic resonance imaging may be helpful in evaluation of the fetal anatomy in cases with oligohydramnios [8].
The diagnosis is often made late in pregnancy. In this case detection of the abnormality at 22 weeks' of pregnancy allowed termination of pregnancy. Early detection of caudal regression syndrome at 11 weeek's of gestational age by transvaginal ultrasound scanning was reported. In the first trimester crown-rump length was found to be smaller than expected in caudal regression using abdominal ultrasound [9]. In differential diagnosis body-wall complex with caudal defects and segmental spinal dysgenesis should be evaluated. Bladder exstrophy, omphalocele and sacral myelomeningocele can be demonstrated in body-wall complex.
Segmental spinal dysgenesis (SSD) is a rare congenital abnormality in which a segment of the spine and spinal cord fails to develop properly. SSD and caudal regression syndrome probably represent two faces of a single spectrum of segmental malformations of the spine and spinal cord. The neuroradiologic picture depends on the severity of the malformation and on its segmental level along the longitudinal embryonic axis. The severity of the morphologic derangement correlates with residual spinal cord function and with severity of the clinical deficit [10].
Orthopedic, gastrointestinal, genitourinary and cardiac anomalies are associated with caudal regression syndrome [11]. In our case club feet, flexion contractures of hips and knees, kyphoscoliosis and absence of ribs are the orthopedic deformities. A ventricular septal defect was the associated cardiac malformation [12].
The prognosis for children with caudal regression syndrome depends on the severity of the lesion and the presence of associated anomalies. Surviving infants have usually a normal mental function and they require extensive urologic and orthopedic assistence [13].
Conclusion
Prenatal ultrasonographic diagnosis of caudal regression syndrome is possible at 22 weeks' of gestation. Visualization of the anomalies such as amputation of the spine and the deformities of extremities which were described in this report should not be difficult, particularly with normal amniotic fluid.
References
Reece EA, Hobbins JC: Diabetic embryopathy: Pathogenesis, prenatal diagnosis and prevention. Obstet Gynecol Surv. 1986, 41: 325-335.
Mills JL: Malformations in infants of diabetic mothers. Teratology. 1984, 25: 385-394.
Passarge E, Lenz W: Syndrome of caudal regression in infants of diabetic mothers. Pediatrics. 1966, 37: 672-
Gabbe SG, Cohen AW: Diabetes mellitus in pregnancy. In: Perinatal medicine: Management of the high risk fetus and neonate. (Edited by Bolognese RJ, Schwarz RH, Schneider J). Baltimore, Williams and Wilkins. 1982, 336-347.
Valenzano M, Paoletti R, Rossi A, et al: Sirenomelia. Pathologic features, antenatal ultrasonographic clues, and a review of current embryogenic theories. Hum Reprod. 1999, 5: 82-86.
Sonek JD, Gabbe SG, Landon MB, et al: Antenatal diagnosis of sacral agenesis syndrome in a pregnancy complicated by diabetes mellitus. Am J Obstet Gynecol. 1990, 162: 806-
Mihmanli I, Kuruoglu S, Kantarci F, Kanberoglu K: Dorsolumbosacral agenesis. Pediatr Radiol. 2001, 31: 286-288. 10.1007/s002470000411.
Quetel TA, Mejides AA, Salman FA, et al: Amnioinfusion: An aid in the ultrasonographic evaluation of severe oligohydramnios in pregnancy. Am J Obstet Gynecol. 1992, 167: 333-
Fitzmorris-Glass R, Mattrey RF, Cantrell CJ: Magnetic resonance imaging as an adjunction to ultrasound in oligohydramnios. Detection of syrenomelia. J Ultrasound Med. 1989, 8: 159-
Tortori-Donati P, Fondelli MP, Rossi A, et al: Segmental spinal dysgenesis: neuroradiologic findings with clinical and embryologic correlation. Am J Neuroradiol. 1999, 20: 445-456.
Baxi L, Warren W, Collins MH, Timor-Tritsch IE: Early detection of caudal regression syndrome with transvaginal scanning. Obstet Gynecol. 1990, 75: 486-489.
Mariani AJ, Stern J, Khan AU, et al: Sacral agenesis: An analysis of 11 cases and review of the literature. J Urol. 1979, 122: 684-
Adra A, Cordero D, Mejides A, et al: Caudal regression syndrome: Etiopathogenesis, prenatal diagnosis, and perinatal management. Obstet Gynecol Sur. 1994, 49: 508-516.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2393/1/8/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Aslan, H., Yanik, H., Celikaslan, N. et al. Prenatal diagnosis of Caudal Regression Syndrome : a case report. BMC Pregnancy Childbirth 1, 8 (2001). https://doi.org/10.1186/1471-2393-1-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2393-1-8