Abstract
Background
Daptomycin is a cyclic lipopeptide with potent activity and broad spectrum against Gram-positive bacteria currently used for the treatment of complicated skin and skin structure infections and bacteremia, including right sided endocarditis. We evaluated the in vitro activity of this compound and selected comparator agents tested against clinical strains of staphylococci and enterococci collected in European medical centers in 2005.
Methods
A total of 4,640 strains from 23 medical centers located in 10 European countries, Turkey and Israel (SENTRY Program platform) were tested for susceptibility by reference broth microdilution methods according to Clinical and Laboratory Standards Institute guidelines and interpretative criteria. Mueller-Hinton broth was supplemented to 50 mg/L Ca++ for testing daptomycin. Results for oxacillin (methicillin)-resistant staphylococci and vancomycin-resistant enterococci were analyzed separately.
Results
Oxacillin resistance rates among Staphylococcus aureus varied from 2.1% in Sweden to 42.5% in the United Kingdom (UK) and 54.7% in Ireland (29.1% overall), while vancomycin resistance rates varied from 0.0% in France, Sweden and Switzerland to 66.7% in the UK and 71.4% in Ireland among Enterococcus faecium (17.9% overall). All S. aureus strains were inhibited at daptomycin MIC of 1 mg/L (MIC50/90, 0.25/0.5 mg/L; 100.0% susceptible) and only one coagulase-negative staphylococci strain (0.1%) showed an elevated (>1 mg/L) daptomycin MIC value (4 mg/L). Among E. faecalis (MIC50/90, 0.5/1 mg/L; 100% susceptible) the highest daptomycin MIC value was 2 mg/L; while among E. faecium (MIC50/90, 2/4 mg/L; 100% susceptible) the highest MIC result was 4 mg/L.
Conclusion
Daptomycin showed excellent in vitro activity against staphylococci and enterococci collected in European medical centers in 2005 and resistance to oxacillin, vancomycin or quinupristin/dalfopristin did not compromise its activity overall against these pathogens. Based on these results and those of previous publications, daptomycin appears to be an excellent therapeutic option for serious infections caused by oxacillin-resistant staphylococci and vancomycin-resistant enterococci in Europe.
Similar content being viewed by others
Background
Gram-positive bacteria, especially staphylococci and enterococci, are extremely important pathogens causing infections in the hospital environment. Staphylococcus aureus, coagulase-negative staphylococci (CoNS) and enterococci are among the five most frequently isolated organisms from nosocomial bloodstream infections (BSI) [1, 2]. These three pathogens are responsible for approximately one-half of the cases of BSI in North American medical centers evaluated by the SENTRY Antimicrobial Surveillance Program [1].
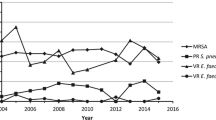
Oxacillin (methicillin)-resistant S. aureus (MRSA) is currently recognized as a major problem in hospitals worldwide [3]. The 2004 National Nosocomial Infections Surveillance (NNIS) system report identified methicillin resistance in 59.5% of S. aureus infections in intensive care unit (ICU) patients [4]. This represented an 11% increase in resistance compared with rates for the period 1998 to 2002. The SCOPE project report showed a significant increase in the proportion of S. aureus isolates resistant to methicillin among patients in ICUs from 1995 to 2001 (22% vs. 57%; P < 0.001) [5]. In hospitalized pediatric patients with staphylococcal BSI, the proportion expressing methicillin resistance increased from 10% in 1995 to 29% in 2001 [6]. Furthermore, MRSA has recently emerged as an important cause of community-acquired infection in many parts of the United States (USA) [7].
A dramatic rise in frequency of enterococcal infections and the prevalence of vancomycin-resistant enterococci (VRE) occurred during the 1990s in the USA, first in ICUs, then essentially throughout hospitals [8–10]. The 2004 NNIS report indicated that nearly 30% of all enterococci isolated from patients infected in ICUs were resistant to vancomycin [4]. Although most European countries were able to control the hospital dissemination of VRE in the 1990s, the prevalence of this pathogen has recently increased dramatically in many European countries [8, 11].
Daptomycin is a cyclic lipopeptide derived from Streptomyces roseosporus [12–14]. The mode of action is unique in that it binds to bacterial membranes, in the presence of physiological levels of calcium ions [15, 16]. Daptomycin is primarily effective against Gram-positive bacteria, due to its inability to penetrate the outer membrane of Gram-negative organisms [17]. It is available as an intravenous drug and exhibits linear kinetics and is rapidly bactericidal [12, 16–18]. Daptomycin is active against a wide range of multidrug-resistant (MDR) organisms for which there are very few therapeutic alternatives, such as MRSA and VRE. Due to daptomycin's requirement of calcium to be present for effective binding to the bacterial membrane, susceptibility testing requires appropriate supplementation of calcium to simulate levels found in human serum (45–55 mg/L) [14–16].
Daptomycin was approved by the USA Food and Drug Administration (FDA) in September 2003 for the treatment of complicated skin and skin structure infections (cSSTI) at a dosage of 4 mg/kg every 24 hours; and more recently for the treatment of S. aureus bacteremia with or without right sided infectious endocarditis at a dosage of 6 mg/kg every 24 hours [12, 17, 19]. Daptomycin has also been recently approved by the European Medicines Agency (EMEA) for the treatment of cSSTI [20]. In addition, the European Committee for Antimicrobial Susceptibility Testing (EUCAST) has assigned daptomycin breakpoints for staphylococci and streptococci [21], which are ≤ 1 mg/L for susceptible (similar to Clinical and Laboratory Standards Institute [CLSI] and US-FDA breakpoints) and ≥2 mg/L for resistance [22].
We have recently published a comprehensive analysis of the antimicrobial susceptibility of Gram-positive bacteria collected in European medical centers in previous years (2002–2004) [11]. In the present study, we summarize the antimicrobial activity results of daptomycin and several comparator agents tested against 4,640 clinical staphylococcal and enterococcal isolates collected in 2005.
Methods
Bacterial strains
A total of 4,640 contemporary clinical isolates, including 2,887 staphylococci (1,946 S. aureus and 941 CoNS) and 953 enterococci (646 Enterococcus faecalis and 307 E. faecium), were evaluated in the present study. All isolates were non-duplicate, consecutive, clinical strains collected from patients hospitalized in 23 medical centers located in 10 European countries, Turkey and Israel in 2005 (SENTRY Program platform) following common protocols. The isolates were collected according to site of infection. Identifications were performed by the submitting laboratories and confirmed in the monitoring laboratory (JMI Laboratories, North Liberty, Iowa, USA) using standard biochemical algorithms and/or the Vitek System (bioMerieux, Hazelwood, Missouri, USA).
Antimicrobial agents and susceptibility testing
Daptomycin and selected comparator agents were tested by CLSI (formerly the NCCLS) criteria [22]. All strains were tested for antimicrobial susceptibility by the broth microdilution method. Dry-form, validated microdilution panels and broth reagents were manufactured by TREK Diagnostics (Cleveland, OH, USA). Mueller-Hinton Broth (MHB) adjusted to contain physiological levels of calcium (50 mg/L) was used when testing daptomycin [15]. Comparator agents included those representing the most common classes and examples of drugs used for the empiric or directed treatment of the indicated pathogen.
The isolates were categorized as susceptible and resistant according to CLSI guidelines [22]. A daptomycin susceptible breakpoint of ≤ 1 mg/L was used for staphylococci, while ≤ 4 mg/L was used for enterococci, as approved by the USA-FDA, CLSI and EUCAST [12, 20–22]. The following quality control organisms were concurrently tested: E. faecalis ATCC 29212, and S. aureus ATCC 29213.
Results
The isolates were collected mainly from bloodstream infection (55.1%), skin and skin structure infections (22.3%) and pneumonia (8.1%). France (940 strains; 20.3% of all isolates), Germany (848 strains; 18.3%) and Italy (519 strains; 11.2%) contributed with the highest number of strains; while Greece (78 strains; 1.7%), Israel (187 strains; 4.0%) and Switzerland (217 strains; 4.7%) supplied the lowest number of samples (Table 1). The frequencies of oxacillin resistance among staphylococci and vancomycin resistance among enterococci by country are listed in Table 2, and showed that oxacillin resistance rates varied from 2.1% in Sweden (187 strains) to 42.5% in the United Kingdom (UK; 153 strains) and 54.7% in Ireland (203 strains) among S. aureus (29.1% overall). Oxacillin resistance rates were most elevated among CoNS strains, varying from 53.3% in the UK (30 strains) to 83.3% in Greece (24 strains). Vancomycin-resistant E. faecalis strains were detected only in Italy (one strain; 1.6%) and UK (five strains; 17.9%), while among E. faecium, the vancomycin resistance rates varied from 0.0% in France, Sweden and Switzerland to 66.7% in the UK (18 strains) and 71.4% in Ireland (14 strains), with an all Europe rate of 17.9% (Table 2).
Daptomycin was generally very potent against the Gram-positive organisms collected in European medical centers in 2005 (Table 3). All S. aureus strains were inhibited at a daptomycin MIC of ≤1 mg/L (100.0% susceptible) with a MIC50 of 0.25 mg/L and a MIC90 of only 0.5 mg/L. A slight trend toward higher daptomycin MIC values was observed for MRSA (52.8% at 0.25 mg/L and 43.8% at 0.5 mg/L) compared to oxacillin (methicillin)-susceptible S. aureus (MSSA; 70.7% at 0.25 mg/L and 24.9% at 0.5 mg/L). This very modest skewing was less apparent for CoNS where the frequency of strains inhibited at 0.25 mg/L were 48.1 and 47.3%, and at 0.5 mg/L were 33.6 and 43.2% for oxacillin (methicillin)-susceptible (MS-CoNS) and oxacillin (methicillin)-resistant (MR-CoNS) strains, respectively. Only one CoNS strain (0.1%) exhibited an elevated daptomycin MIC value for an oxacillin-susceptible strain isolated from a medical center located in Rome, Italy (reproducible MIC value of 4 mg/L). All other CoNS strains were inhibited at daptomycin MIC ≤1 mg/L (Table 3).
Daptomycin was also highly active against enterococci (Table 3). Among 646 tested E. faecalis (MIC50, 0.5 mg/L; MIC90, 1 mg/L; 100% susceptible) the highest daptomycin MIC value was only 2 mg/L (2.2% of strains tested); while among E. faecium (MIC50, 2 mg/L; MIC90, 4 mg/L; 100% susceptible) the highest MIC value was 4 mg/L.
MSSA strains showed high rates of susceptibility (>95%) to most comparison antimicrobial agents tested except erythromycin (85.9% susceptibility), ciprofloxacin (93.0%) and levofloxacin (93.9%). In contrast, resistance rates to many agents were high among MRSA strains (Table 4). The most active compounds tested against this pathogen (100.0% susceptible) were daptomycin (MIC90, 0.5 mg/L), linezolid (MIC90, 2 mg/L), teicoplanin (MIC90, ≤2 mg/L) and vancomycin (MIC90, 1 mg/L; Table 4). CoNS showed higher rates of resistance compared to S. aureus. The fluoroquinolones, ciprofloxacin and levofloxacin, were active against only 86.9 and 87.3% of MS-CoNS, respectively. In contrast, daptomycin, linezolid and vancomycin were the only compounds active against 100.0% of MR-CoNS at the susceptible breakpoint (Table 4). It is important to note the emergence of quinupristin/dalfopristin resistance among both MRSA (98.6% susceptible) and MR-CoNS (99.3% susceptible).
Daptomycin (MIC90, 0.5 mg/L; 100.0% susceptible), ampicillin (MIC90, 2 mg/L; 99.4% susceptible) and linezolid (MIC90, 2 mg/L; 100.0% susceptible) were very active against E. faecalis, and only six vancomycin-resistant E. faecalis strains (0.9%) were detected in Europe in 2005 (Table 4). These strains were from Italy (one strains) and the UK (five strains), and all six strains showed low daptomycin MIC values (0.25 – 1 mg/L). On the other hand, E. faecium exhibited high rates of resistance to most antimicrobials tested. Resistance to vancomycin was observed in 17.9% of E. faecium strains (Table 2) and only daptomycin (MIC50, 2 mg/L and MIC90, 4 mg/L) and linezolid (MIC50, 1 mg/L and MIC90, 2 mg/L) were active against all vancomycin-resistant E. faecium strains tested. Furthermore, only 72.7% of vancomycin-resistant and 70.2% of vancomycin-susceptible E. faecium strains were susceptible to quinupristin/dalfopristin (Table 4).
Discussion
The treatment of serious MRSA infections presents a great challenge to clinicians, particularly bacteremias and infective endocarditis, for which bactericidal therapy is essential to maximize successful clinical outcomes [23, 24]. Vancomycin has been the preferred antimicrobial agent to treat such MRSA infections; however, the clinical efficacy of this glycopeptide has become more limited [24–27]. In addition to the increasing reports of isolates with reduced susceptibility (vancomycin-intermediate S. aureus [VISA]) or high-level vancomycin resistance (vancomycin-resistant S. aureus [VRSA]), other reports have shown limited bactericidal activity against a large proportion of strains with vancomycin MIC values within the CLSI susceptible range [22, 27–30]. Linezolid and quinupristin-dalfopristin represent alternative treatment options for serious MRSA infections; however, these compounds also possess important limitations. Quinupristin-dalfopristin, a streptogramin combination, requires a central venous access to be administrated and has been linked to some adverse events such as arthralgia and myalgia [31, 32]. Concerns with linezolid, an oxazolidinone, include possible hematologic toxicity of long-term treatment and the fact that it is a bacteriostatic agent against staphylococci and enterococci and is not indicated for the treatment endocarditis and serious infections in immuno-suppressed patients [31, 33].
Although they are relatively nonvirulent organisms, the enterococci have become increasingly common nosocomial pathogens because they are resistant to many antimicrobials and can survive in the environment for prolonged periods of time. Enterococci are intrinsically resistant to multiple antimicrobial agents. Furthermore, other agents that are active in vitro, such as vancomycin, are not bactericidal at clinically achievable concentrations. As shown in the present study, E. faecium is usually resistant to ampicillin, and this type of resistance has been reported as a significant predictor of treatment failure [9, 34]. Combination therapy of a cell-wall active agent plus an aminoglycoside has become the "standard of care" for patients with serious enterococcal infections, such as endocarditis or BSI, but the prevalence of high-level resistance to aminoglycosides and to ampicillin are increasing, leaving glycopeptides as the remaining class of active antimicrobials. Clearly, the emergence of VRE has further complicated therapeutic options [35].
Two antimicrobial agents have been approved specifically for the treatment of VRE infections: quinupristin/dalfopristin and linezolid [31, 36]. However, quinupristin/dalfopristin MIC90 results (16 mg/L) for E. faecalis systemic infections exceeds the maximum achievable serum concentrations, making this compound inactive for E. faecalis [9, 32], and resistance among E. faecium has been recently increasing, especially in Europe among vancomycin-resistant strains [11, 35, 37]. In this presented study, only 70% of E. faecium were susceptible to quinupristin/dalfopristin. On the other hand, linezolid has potent in vitro activity against both vancomycin-resistant E. faecalis and E. faecium, as well as good therapeutic efficacy for VRE bacteremia in mice [31, 33, 34]. However, as mentioned previously, linezolid has not been recommended for the treatment of endocarditis or serious infections in immuno-suppressed patients due to its predominantly bacteriostatic activity. In addition, the emergence of oxazolidinone resistance has been reported, especially in patients who receive prolonged courses of therapy [33, 38].
Conclusion
Daptomycin is the first member of a novel class of antimicrobial agents, the cyclic lipopeptides [13, 14]. It has broad-spectrum and potent bactericidal activity against Gram-positive pathogens, including MRSA and VRE [39–42]. This compound has demonstrated activity against both growing and stationary-phase bacteria [12–14], [16–18]. Here daptomycin was recognized as highly active against S. aureus and CoNS, including oxacillin-resistant strains. Only one strain showed a daptomycin MIC value >1 mg/L (a CoNS strain with MIC value of 4 mg/L). Vancomycin (MIC50, 1 mg/L) and linezolid (MIC50, 1 – 2 mg/L) were active against all staphylococcal strains tested. However, daptomycin (MIC50, 0.25 – 0.5 mg/L) was four-fold more potent than these key comparison bacteriostatic antimicrobials. Furthermore, all enterococci, including vancomycin-resistant strains were susceptible to daptomycin and resistance rates were relatively high to all other compounds tested, except linezolid (see Table 4).
In summary, daptomycin showed excellent in vitro activity in a surveillance study against staphylococci and enterococci collected in European medical centers in 2005. Resistance to oxacillin, vancomycin, quinupristin/dalfopristin did not compromise daptomycin potency against these pathogens. Based on these results and those of previous publications [11, 43, 44], daptomycin appears to be an excellent therapeutic option for serious infections caused by MRSA, MR-CoNS and VRE (especially E. faecium) in Europe.
Abbreviations
- BSI:
-
bloodstream infection
- CLSI:
-
Clinical and Laboratory Standards Institute
- CoNS:
-
coagulase-negative staphylococci
- cSSTI:
-
complicated skin and soft tissue infection
- EMEA:
-
European Medicines Agency
- EUCAST:
-
European Committee for Antimicrobial Susceptibility Testing
- FDA:
-
Federal Drug Administration
- ICU:
-
intensive care unit
- MDR:
-
multidrug-resistant
- MHB:
-
Mueller-Hinton broth
- MIC:
-
minimum inhibitory concentration
- MR-CoNS:
-
methicillin-resistant coagulase-negative staphylococci
- MRSA:
-
methicillin-resistant Staphylococcus aureus
- MS-CoNS:
-
methicillin-resistant coagulase-negative staphylococci
- MSSA:
-
methicillin-susceptible Staphylococcus aureus
- NCCLS:
-
National Committee for Clinical Laboratory Standards
- NNIS:
-
National Nosocomial Infections Surveillance
- UK:
-
United Kingdom
- USA:
-
United States of America
- VISA:
-
vancomycin-intermediate Staphylococcus aureus
- VRSA:
-
vancomycin-resistant Staphylococcus aureus
- VRE:
-
vancomycin-resistant enterococci
References
Biedenbach DJ, Moet GJ, Jones RN: Occurrence and antimicrobial resistance pattern comparisons among bloodstream infection isolates from the SENTRY Antimicrobial Surveillance Program (1997-2002). Diagn Microbiol Infect Dis. 2004, 50 (1): 59-69. 10.1016/j.diagmicrobio.2004.05.003.
Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP: Nosocomial bloodstream infections in United States hospitals: A three-year analysis. Clin Infect Dis. 1999, 29 (2): 239-244.
Rice LB: Antimicrobial resistance in Gram-positive bacteria. American Journal of Infection Control. 2006, 34 (5, Supplement 1): S11-S19. 10.1016/j.ajic.2006.05.220.
NNIS: National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004, 32 (8): 470-485. 10.1016/j.ajic.2004.10.001.
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB: Nosocomial bloodstream infections in US hospitals: Analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004, 39 (3): 309-317. 10.1086/421946.
Wisplinghoff H, Seifert H, Tallent SM, Bischoff T, Wenzel RP, Edmond MB: Nosocomial bloodstream infections in pediatric patients in United States hospitals: Epidemiology, clinical features and susceptibilities. Pediatr Infect Dis J. 2003, 22 (8): 686-691.
Tenover FC, McDougal LK, Goering RV, Killgore G, Projan SJ, Patel JB, Dunman PM: Characterization of a strain of community-associated methicillin-resistant Staphylococcus aureus widely disseminated in the United States. J Clin Microbiol. 2006, 44 (1): 108-118. 10.1128/JCM.44.1.108-118.2006.
Willems RJ, Top J, van Santen M, Robinson DA, Coque TM, Baquero F, Grundmann H, Bonten MJ: Global spread of vancomycin-resistant Enterococcus faecium from distinct nosocomial genetic complex. Emerg Infect Dis. 2005, 11 (6): 821-828.
Mascini EM, Bonten MJ: Vancomycin-resistant enterococci: Consequences for therapy and infection control. Clin Microbiol Infect. 2005, 11 Suppl 4: 43-56. 10.1111/j.1469-0691.2005.01164.x.
Stevens MP, Edmond MB: Endocarditis due to vancomycin-resistant enterococci: Case report and review of the literature. Clin Infect Dis. 2005, 41 (8): 1134-1142. 10.1086/444459.
Sader HS, Streit JM, Fritsche TR, Jones RN: Antimicrobial susceptibility of Gram-positive bacteria isolated from European medical centres: Results of the Daptomycin Surveillance Programme (2002-2004). Clin Microbiol Infect. 2006, 12 (9): 844-852. 10.1111/j.1469-0691.2006.01550.x.
Package Insert: Cubicin (daptomycin for injection). Lexington MA. (Cubist Pharmaceuticals, Inc). Available at http://www.cubicin.com/2006_full_pi.pdf. Accessed on June 28, 2006. 2006, [http://www.cubicin.com/2006_full_pi.pdf]
Fenton C, Keating GM, Curran MP: Daptomycin. Drugs. 2004, 64 (4): 445-55; discussion 457-8. 10.2165/00003495-200464040-00009.
Steenbergen JN, Alder J, Thorne GM, Tally FP: Daptomycin: A lipopeptide antibiotic for the treatment of serious Gram-positive infections. J Antimicrob Chemother. 2005, 55 (3): 283-288. 10.1093/jac/dkh546.
Fuchs PC, Barry AL, Brown SD: Daptomycin susceptibility tests: Interpretive criteria, quality control, and effect of calcium on in vitro tests. Diagn Microbiol Infect Dis. 2000, 38 (1): 51-58. 10.1016/S0732-8893(00)00164-4.
Silverman JA, Perlmutter NG, Shapiro HM: Correlation of daptomycin bactericidal activity and membrane depolarization in Staphylococcus aureus. Antimicrob Agents Chemother. 2003, 47 (8): 2538-2544. 10.1128/AAC.47.8.2538-2544.2003.
Carpenter CF, Chambers HF: Daptomycin: Another novel agent for treating infections due to drug-resistant Gram-positive pathogens. Clin Infect Dis. 2004, 38 (7): 994-1000. 10.1086/383472.
Laganas V, Alder J, Silverman JA: In vitro bactericidal activities of daptomycin against Staphylococcus aureus and Enterococcus faecalis are not mediated by inhibition of lipoteichoic acid biosynthesis. Antimicrob Agents Chemother. 2003, 47 (8): 2682-2684. 10.1128/AAC.47.8.2682-2684.2003.
Segreti JA, Crank CW, Finney MS: Daptomycin for the treatment of Gram-positive bacteremia and infective endocarditis: A retrospective case series of 31 patients. Pharmacotherapy. 2006, 26 (3): 347-352. 10.1592/phco.26.3.347.
Cubicin Product Information: European Medicines Agency. http://www.emea.eu.int/humandocs/Humans/EPAR/cubicin/cubicin.htm. Accessed May 11, 2006. 2006, [http://www.emea.eu.int/humandocs/Humans/EPAR/cubicin/cubicin.htm]
EUCAST: The European Committee on Antimicrobial Susceptibility Testing (EUCAST) Steering Committee. EUCAST Technical Note on daptomycin. Clin Microbiol Infect. 2006, 12 (6): 599-601. 10.1111/j.1469-0691.2006.01455.x.
Clinical and Laboratory Standards Institute: M100-S16, Performance standards for antimicrobial susceptibility testing; sixteenth informational supplement. 2006, Wayne, PA: CLSI
Pankey GA, Sabath LD: Clinical relevance of bacteriostatic versus bactericidal mechanisms of action in the treatment of Gram-positive bacterial infections. Clin Infect Dis. 2004, 38 (6): 864-870. 10.1086/381972.
Sakoulas G, Moise-Broder PA, Schentag J, Forrest A, Moellering RC, Eliopoulos GM: Relationship of MIC and bactericidal activity to efficacy of vancomycin for treatment of methicillin-resistant Staphylococcus aureus bacteremia. J Clin Microbiol. 2004, 42 (6): 2398-2402. 10.1128/JCM.42.6.2398-2402.2004.
Asseray N, Jacqueline C, Le Mabecque V, Batard E, Bugnon D, Potel G, Caillon J: Activity of glycopeptides against Staphylococcus aureus infection in a rabbit endocarditis model: MICs do not predict in vivo efficacy. Antimicrob Agents Chemother. 2005, 49 (2): 857-859. 10.1128/AAC.49.2.857-859.2005.
Sakoulas G, Gold HS, Cohen RA, Venkataraman L, Moellering RC, Eliopoulos GM: Effects of prolonged vancomycin administration on methicillin-resistant Staphylococcus aureus (MRSA) in a patient with recurrent bacteraemia. J Antimicrob Chemother. 2006, 57 (4): 699-704. 10.1093/jac/dkl030.
Jones RN: Microbiological features of vancomycin in the 21st century: Minimum inhibitory concentration creep, bactericidal/static activity, and applied breakpoints to predict clinical outcomes or detect resistant strains. Clin Infect Dis. 2006, 42 Suppl 1: S13-24. 10.1086/491710.
Cosgrove SE, Carroll KC, Perl TM: Staphylococcus aureus with reduced susceptibility to vancomycin. Clin Infect Dis. 2004, 39 (4): 539-545. 10.1086/422458.
May J, Shannon K, King A, French G: Glycopeptide tolerance in Staphylococcus aureus. J Antimicrob Chemother. 1998, 42 (2): 189-197. 10.1093/jac/42.2.189.
Sader HS, Fritsche TR, Jones RN: Daptomycin bactericidal activity and correlation between disk and broth microdilution method results in testing of Staphylococcus aureus strains with decreased susceptibility to vancomycin. Antimicrob Agents Chemother. 2006, 50 (7): 2330-2336. 10.1128/AAC.01491-05.
Lundstrom TS, Sobel JD: Antibiotics for Gram-positive bacterial infections: Vancomycin, quinupristin-dalfopristin, linezolid, and daptomycin. Infect Dis Clin North Am. 2004, 18 (3): 651-68, x. 10.1016/j.idc.2004.04.014.
Linden PK, Moellering RC, Wood CA, Rehm SJ, Flaherty J, Bompart F, Talbot GH: Treatment of vancomycin-resistant Enterococcus faecium infections with quinupristin/dalfopristin. Clin Infect Dis. 2001, 33 (11): 1816-1823. 10.1086/323899.
Moellering RC: Linezolid: The first oxazolidinone antimicrobial. Ann Intern Med. 2003, 138 (2): 135-142.
Landman D, Quale JM: Management of infections due to resistant enterococci: A review of therapeutic options. J Antimicrob Chemother. 1997, 40 (2): 161-170. 10.1093/jac/40.2.161.
Schouten MA, Voss A, Hoogkamp-Korstanje JA: Antimicrobial susceptibility patterns of enterococci causing infections in Europe. The European VRE Study Group. Antimicrob Agents Chemother. 1999, 43 (10): 2542-2546.
Livermore DM: Quinupristin/dalfopristin and linezolid: Where, when, which and whether to use?. J Antimicrob Chemother. 2000, 46 (3): 347-350. 10.1093/jac/46.3.347.
Vergis EN, Hayden MK, Chow JW, Snydman DR, Zervos MJ, Linden PK, Wagener MM, Schmitt B, Muder RR: Determinants of vancomycin resistance and mortality rates in enterococcal bacteremia. A prospective multicenter study. Ann Intern Med. 2001, 135 (7): 484-492.
Gonzales RD, Schreckenberger PC, Graham MB, Kelkar S, DenBesten K, Quinn JP: Infections due to vancomycin-resistant Enterococcus faecium resistant to linezolid. Lancet. 2001, 357 (9263): 1179-10.1016/S0140-6736(00)04376-2.
Jevitt LA, Smith AJ, Williams PP, Raney PM, McGowan JE, Tenover FC: In vitro activities of daptomycin, linezolid, and quinupristin-dalfopristin against a challenge panel of staphylococci and enterococci, including vancomycin-intermediate Staphylococcus aureus and vancomycin-resistant Enterococcus faecium. Microb Drug Resist. 2003, 9 (4): 389-393. 10.1089/107662903322762833.
Johnson AP, Mushtaq S, Warner M, Livermore DM: Activity of daptomycin against multi-resistant Gram-positive bacteria including enterococci and Staphylococcus aureus resistant to linezolid. Int J Antimicrob Agents. 2004, 24 (4): 315-319. 10.1016/j.ijantimicag.2004.04.006.
Sader HS, Streit JM, Fritsche TR, Jones RN: Antimicrobial activity of daptomycin against multidrug-resistant Gram-positive strains collected worldwide. Diagn Microbiol Infect Dis. 2004, 50 (3): 201-204. 10.1016/j.diagmicrobio.2004.07.002.
Sader HS, Fritsche TR, Jones RN: Antimicrobial activity of daptomycin tested against clinical strains of indicated species isolated in North American medical centers (2003). Diagn Microbiol Infect Dis. 2005, 53 (4): 329-332. 10.1016/j.diagmicrobio.2005.07.001.
Fluit AC, Schmitz FJ, Verhoef J, Milatovic D: Daptomycin in vitro susceptibility in European Gram-positive clinical isolates. Int J Antimicrob Agents. 2004, 24 (1): 59-66. 10.1016/j.ijantimicag.2003.12.014.
Fluit AC, Schmitz FJ, Verhoef J, Milatovic D: In vitro activity of daptomycin against Gram-positive European clinical isolates with defined resistance determinants. Antimicrob Agents Chemother. 2004, 48 (3): 1007-1011. 10.1128/AAC.48.3.1007-1011.2004.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/7/29/prepub
Acknowledgements
We would like to thank the sites participating in this surveillance study: Prof. Jacques Bille (University Hospital, Lausanne, Switzerland); Dr. Karen E. Bowker (Southmead Hospital, Bristol, UK); Dr. Rafael Canton (Hospital Ramon y Cajal, Madrid, Spain); Prof. Eugenio Debbia (San Martino-Instituto Di Microbiolgia, Genova, Italy); Prof. Jerome Etienne (Hospital Edouard Herriot, Lyon, France); Dr. Wolfgang Falk (Labor Dres Ballies, Kiel, Germany); Prof. Giovanni Fadda (Policlinico Agostino Gemelli, Roma, Italy); Prof. Deniz Gur (Hacettepe University, Anakara, Turkey); Prof. Waleria Hryniewicz (National Institute of Public Health, Warsaw, Poland); Dr. Gudrun Just-Nuebling (University of Frankfurt, Frankfurt, Germany); Dr. Gunnar Kahlmeter (Central Hospital, Vaxjo, Sweden); Dr. Nathan Keller (Chaim Sheba Medical Center, Tel-Hashomer, Israel); Dr. Volkan Korten (Marmara University Hospital, Istanbul, Turkey); Dr. Roland Leclercq (Hospital Cote de Nacre, Cedex, France); Prof. Nicholas Legakis (National University of Athens Medical School, Athens, Greece); Prof. Giuseppe Nicolletti (Azienda Policlinico Universita de Catania, Catania, Italy); Dr. Lennart Nilsson (University Hospital Linkoping, Linkoping, Sweden); Dr. A. Oltmann (University of Leipzig School of Medicine, Liepzig, Germany); Dr. Alvaro Pascual (Univesity Hospital V. de Marcarena, Sevilla, Spain); Dr. Yves Rio (Centre Hospitalier Regional de Metz, Metz, France); Dr. Micheline Roussel-Delvallez (A. Calmette Hospital, Lille Cedex, France); Prof. Franz-Joseph Schmitz (Klinikum Minden, Minden, Germany); Dr. Edward Smyth (Beaumont Hospital, Dublin, Ireland); and Prof. Claude James Soussey (Hospital Henri Mondor, Creteil Cedex, France). We also express our appreciation to the following individuals for assistance with technical support, manuscript preparation, and editorial processing: N. O'Mara-Morrissey, P. Rhomberg and P. Strabala. This study was funded by a research grant from Chiron Corporation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
H. S. Sader, T.R. Fritsche and R. N. Jones have received research/education grants in the last three years from: AB BIODISK, Abbott, AlamX, Arpida, AstraZeneca, Avexa, Basilea, Bayer, Becton Dickinson, bioMerieux, Bristol-Myers Squibb, Cadence, Cerexa, Chiron, Cubist, Daiichi, Elan, Elanco, Enanta, GlaxoSmithKline, Intrabiotics, Johnson & Johnson, LG Chemicals, Merck, Micrologix, Novartis, Optimer, Ordway, Osmotics, Peninsula, Pfizer, Replidyne, Schering-Plough, Sequoia, Serenex, Shionogi, Theravance, TREK Diagnostics, and Wyeth.
Authors' contributions
HSS: Data analysis and manuscript writing.
AAW: Technical support and manuscript writing.
TRF: Data analysis and manuscript revision.
RNJ: Study design, data analysis and manuscript revision.
The content has been read and approved by all co-authors.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Sader, H.S., Watters, A.A., Fritsche, T.R. et al. Daptomycin antimicrobial activity tested against methicillin-resistant staphylococci and vancomycin-resistant enterococci isolated in European medical centers (2005). BMC Infect Dis 7, 29 (2007). https://doi.org/10.1186/1471-2334-7-29
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-7-29