Abstract
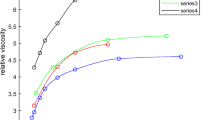
A mathematical model of aggregation and destruction of erythrocyte clots in the shear flow is constructed. Calculations show the influence of shear stresses in a blood flow on the mean dimension of clots. It is also shown that the sinuses of aneurysms create conditions for formation of large agglomerates, which can result in thrombosis of a blood vessel under consideration.
Similar content being viewed by others
References
Z. Lou and W. J. Yang, “A Computer Simulation of the Blood Flow in the Aortic Bifurcation with Flexible Walls,” in Proceedings of the ASCE Engineering Mechanics Speciality Conference “Mechanics Computing in 1990’s and Beyond”, Ohio, 1991, Ed. by H. Adeli and R. Sierakowski (ASCE, New York, 1991), vol. 1, pp. 544–548.
G. G. Ferguson, “Physical Factors in the Initiation, Growth and Rupture of Human Intracranial Saccular Aneurysms,” J. Neurosurg. 37, 666–676 (1972).
W. E. Stehbens, “Flow Disturbances in Glass Models of Aneurysms at Low Reynolds Numbers,” Q. J. Exp. Physiol. 59, 167–174 (1974).
H. J. Steiger, “Pathophysiology of Development and Rupture of Cerebral Aneurysms,” Acta Neurochir. 48, 11–23 (1990).
K. N. T. Kayembe, M. Sasahara, and F. Nazama, “Cerebral Aneurysms and Variations of the Circle of Willis,” Stroke 15, 846–850 (1984).
W. E. Stenbens, “Etiology of Intracranial Berry Aneurysm,” J. Neurosurg. 70, 823–831.
S. Ahmed and D. P. Giddens, “Pulsatile Poststenotic Flow Studies with Laser Doppler Anemometry,” J. Biomech. 17, 695 (1984).
M. Ojha, R. S. Cobbold, K. W. Johnston, and R. L. Hummel, “Pulsatile Flow Through Constricted Tubes: An Experimental Investigation Using Photochromic Tracer Methods,” J. Fluid Mech. 203, 173 (1989).
M. Ojha, R. S. Cobbold, K. W. Johnston, and R. L. Hummel, “Detailed Visualization of Pulsatile Flow Fields Produced by Modelled Arterial Stenoses,” J. Biomed. Eng. 12, 463–469 (1990).
S. Chien, “Physiological and Pathological Significance of Hemorheology,” in Clinical Hemorheology, Ed. by S. Chien (Martinus Nijhoff, Dordrecht, 1987), pp. 125–164.
S. Chien, S. A. Luse, K. M. Jan, et al., “Effects of Macromolecules on the Rheology and Ultrastructure of Red Cells Suspensions,” in Proceedings of the 6th European Conference on Microcirculation, Aalborg, 1970, Ed. by J. Ditzel and D. H. Lewis (S. Karger, Basel), pp. 29–34.
S. Chien, “Clumping (Reversible Aggregation and Irreversible Agglutination) of Blood Cellular Elements,” Thromb. Res. 8(Suppl. II), 189–202 (1976).
S. Chien, “Electrochemical Interaction and Energy Balance in Red Blood Cell Aggregation,” in Topics in Bioelectricity and Bioenergetics, Ed. By G. Milazzo (Wiley, New York, 1981), vol. 4, pp. 73–112.
A. P. Gast and L. Leibler, “Interaction of Sterically Stabilized Particles Suspended in a Polymer Solution,” J. Macromol. 19, 686–691 (1986).
J. F. Joanny, L. Leibler, and P. G. De Gennes, “Effects of Polymer Solutions on Colloid Stability,” J. Polym. Sci. 17, 1030–1084 (1979).
S. Chien, “Biophysical Behavior of Red Cells in Suspensions,” in The Red Blood Cell, Ed. by D. M. Surgenor (Academic Press, New York, 1975), pp. 1031–1133.
M. Elimelech, J. Gregory, X. Jia, and R.A. Williams, Particle Deposition and Aggregation: Measurement, Modeling and Simulation (Butterworth-Heinemann, Oxford, 1995), chap. 6, pp. 157–202.
P. A. Shamlou and N. Titchener-Hooker, “Turbulent Aggregation and Breakup of Particles in Liquids in Stirred Vessels,” in Processing of Solid-Liquid Suspensions, Ed. by P. A. Shamlou (Butterworth-Heinemann, Oxford, 1993), pp. 1–25.
K. Muhle, “Floc Stability in Laminar and Turbulent Flow,” in Coagulation and Flocculation, Theory and Applications, Ed. by B. Dobias (M. Dekker, New York, 1993), pp. 355–390.
A. P. Shortland, R. A. Black, J. C. Jarvis, et al., “Formation and Travel of Vortices in Model Ventricles: Application to the Design of Skeletal Muscle Ventricles,” J. Biorheol. 29(4), 501–511 (1996).
M. Hasegawa, “Rheological Properties and Wall Structures of Large Veins,” J. Biorheol. 20(5), 531–545 (1983).
B. Lim, P. J. Bascom, and R. S. C. Cobbold, “Simulation of Red Cell Aggregation in Shear Flow,” J. Biorheol. 34(6), 425–441 (1997).
Y. W. Yuan and K. K. Shung, “Echoicity of Whole Blood,” J. Ultrasound Med. 8, 425–434 (1989).
L. Y. L. Mo, R. S. C. Cobbold, C. Gutt, et al., “Non-Newtonian Behavior of Whole Blood in a Large Diameter Tube,” J. Biorheol. 28(5), 421–427 (1991).
R. E. N. Shehada, R. S. C. Cobbold, and L. Y. L. Mo, “Aggregation Effects in Whole Blood: Influence of Time and Shear Rate Measurement Using Ultrasound,” J. Biorheol. 31(1) 115–135 (1994).
T. Murata and T. W. Secomb, “Effects of Shear Rate on Rouleau Formation in Simple Shear Flow,” J. Biorheol. 25(1–2), 113–122 (1988).
A. A. Samarskii, An Introduction to the Theory of Difference Schemes (Nauka, Moscow, 1971) [in Russian].
M. Kolb and R. Jullien, “Chemically Limited Versus Diffusion Limited Aggregation,” J. Phys. Lett. 45, 977–981 (1984).
P. Mills, “Non-Newtonian Behavior of Flucculated Suspensions,” J. Phys. Lett. 46, 301–309 (1985).
P. Snabre, M. Bitbol, and P. Mills, “Cell Disaggregation Behavior in Shear Flow,” J. Biophys. 51, 795–807 (1987).
P. Meakin, “Fractal Aggregates and Their Fractal Measures,” in Phase Transitions and Critical Phenomena, Ed. by -. Domb and J. L. Lebowitz (Academic Press, London, 1988), vol. 12.
T. Fabry, “Mechanism of Erythrocyte Aggregation and Sedimentation,” J. Blood 70, 1572–1576 (1987).
G. Cloutier, Z. Qin, L. G. Durand, and B. G. Teh, “Power Doppler Ultrasound Evaluation of the Shear Rate and Shear Stress Dependencies of Red Blood Cell Aggregation,” IEEE Trans. Biomed. Eng. 43, 441–450 (1996).
A. L. Copley, R. G. King, and C. R. Huang, “Erythrocyte Sedimentation of Human Blood at Varying Shear Rates,” J. Microcirculation, Ed. By J. Grayson and W. Zingg (Plenum Press, New York), 133–134 (1976).
H. Schmid-Schonberg, P. Gaehtgens, and H. Hirsch, “On the Shear Rate Dependence of Red Cell Aggregation in Vitro,” J. Clin. Invest. 47, 1447–1454 (1968).
Y. I. Cho and K.R. Kensey, “Effects of the Non-Newtonian Viscosity of the Blood on Flows in a Diseased Arterial Vessel. Part 1: Steady Flows,” J. Biorheol. 28(3–4), 241–262 (1991).
Author information
Authors and Affiliations
Corresponding author
Additional information
Original Russian Text © S.E. Kornelik, E.K. Borzenko, A.N. Grishin, M.A. Bubenchikov, V.I. Stolyarov, 2008, published in Matematicheskoe Modelirovanie, 2008, Vol. 20, No. 1, pp. 3–5.
Rights and permissions
About this article
Cite this article
Kornelik, S.E., Borzenko, E.K., Grishin, A.N. et al. Formation and destruction of erythrocyte rouleau in a vessel with local bulge. Math Models Comput Simul 1, 1–10 (2009). https://doi.org/10.1134/S2070048209010013
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S2070048209010013