Abstract—
Evaluation of the frequency of chromosome translocations in peripheral blood T-lymphocytes is a generally accepted method of retrospective biodosimetry. Accidental contamination of the Techa River (Chelyabinsk Oblast) in 1950s with bone-seeking long-lived strontium-90 gave an opportunity to evaluate the effect of local red bone marrow (RBM) exposure on translocation formation in the peripheral T-lymphocytes of local inhabitants. The studies of the inhabitants using fluorescent in situ hybridization (FISH) showed that RBM doses calculated based on FISH results were lower than those estimated based on 90Sr body burden measurements. The current study presents analytical review of the published data dealing with the most important processes of the T-lymphocyte development and formation of chromosome aberrations: characteristics of the main compartments where the exposure of T-cell occurs; assessment of the time spent by T-lymphocytes and their progenitors in these compartments; analysis of the dynamics of T-cell populations (proliferation and death); age-related aspects. The paper presents a concept of T-cell Genus (TG) united all the progeny of T progenitor with inheritable specific aberrations that could have developed in bone marrow.

Similar content being viewed by others
Notes
Whole chromosome probes for the coloration of three chromosome pairs (that is, approximately 23% of the genome) were used.
CD molecules can act in different ways often acting as receptors or ligands (molecules that activate the receptor) important for the cell. They can initiate the signaling cascade changing the cell behavior. Some CD proteins play no role in cell signals, but have other functions, such as cell adhesion. There are about 250 different CD proteins.
The main RTE markers are the following: (1) T cell excision circle (TREC), extrachromosomal rings, the product of episomal DNA, which are obtained when rearranging the ТКР genes and which is not replicative, that is, is not transmitted to descendant cells during maternal RTE cell division [22]; (2) the CD31 marker identifies the subgroup of naive cells, in which there is a high level of TREC; (3) protein tyrosine kinase 7 (PTK7) is expressed by a subpopulation of naive CD31+CD4+ cells with a high content of TREC; (4) Ki67 is not an RTE marker, but is a cell cycle marker, which is expressed only by proliferative cells at the stage G1. This allows us to determine what part of the cell population is currently dividing.
REFERENCES
IAEA. Cytogenetic Dosimetry: Applications in Preparedness for and Response to Radiation Emergences, International Atomic Energy Agency, 2011.
Nugis, V.Yu., Sevan’kaev, A.V., Khvostunov, I.K., et al., The results of 25 year-cytogenetic investigation of survivors exposed to different doses of irradiation in the Chernobyl accident, Radiats. Biol. Radioecol., 2011, vol. 51, no. 1, pp. 81–90.
Khvostunov, I.K., Snigiryova, G.P., Moiseenko, V.V., and Lloyd, D.C., A follow-up cytogenetic study of workers highly exposed inside the Chernobyl sarcophagus, Radiat. Prot. Dosim., 2015, vol. 167, no. 4, pp. 405–418. http://www.memoid.ru/node/Perspektivy_atomnoj_ ehnergetiki_sovremennoj_Rossii-cite_ref-.D0.B0.D1. 82.D0.BE.D0.BC_12-7.https://doi.org/10.1093/rpd/ncu351
Biologicheskaya indikatsiya radiatsionnogo vozdeistviya na organizm cheloveka s ispol’zovaniem tsitogeneticheskikh metodov: med. tekhnologiya № FS-2007/015-U (Biological Indication of Radiation Effects on the Human Body Using Cytogenetic Methods: Medical Technology no. FS-2007/015-U), Moscow: Ross. Nauchn. Tsentr Rentgenoradiol., Inst. Obshch. Genet. im. N.I. Vavilova, 2007.
Nowell, P.C., Phytohemagglutinin—an initiator of mitosis in cultures of normal human leukocytes, Cancer Res., 1960, vol. 20, no. 4, pp. 462–466.
Sotnik, N.V., Osovets, S.V., Scherthan, H., and Azizova, T.V., mFISH analysis of chromosome aberrations in workers occupationally exposed to mixed radiation, Radiat. Environ. Biophys., 2014, vol. 53, no. 2, pp. 347–354. https://doi.org/10.1007/s00411-014-0536-7
Tawn, E.J., Whitehouse, C.A., Holdsworth, D., et al., mBAND analysis of chromosome aberrations in lymphocytes exposed in vitro to α-particles and γ-rays, Int. J. Radiat. Biol., 2008, vol. 84, no. 1, pp. 1–7. https://doi.org/10.1080/09553000802078412
Tawn, E.J., Curwen, G.B., Jonas, P., et al., Chromosome aberrations determined by FISH in radiation workers from the Sellafield Nuclear Facility, Radiat. Res., 2015, vol. 184, no. 3, pp. 296–303. https://doi.org/10.1667/RR14125.1
Pilinskaia, M.A., Dybskii, S.S., Skaletskii, Yu.N., et al., The experience of fish technique application for reconstruction of individual radiation doses in Chernobyl liquidators in the framework of Ukrainian-American project “Leukemia,” Tsitol. Genet., 2006, vol. 40, no. 3, pp. 34–39.
Hande, M.P., Azizova, T.V., Burak, L.E., et al., Complex chromosome aberrations persist in individuals many years after occupational exposure to densely ionizing radiation: an mFISH study, Genes Chromosomes Cancer, 2005, vol. 44, no. 1, pp. 1–9. https://doi.org/10.1002/gcc.20217
Curwen, G.B., Sotnik, N.V., Cadwell, K.K., et al., Chromosome aberrations in workers with exposure to α-particle radiation from internal deposits of plutonium: expectations from in vitro studies and comparisons with workers with predominantly external γ-radiation exposure, 2015, vol. 54, no. 2, pp. 195–206. https://doi.org/10.1007/s00411-015-0585-6
Sotnik, N.V. and Azizova, T.V., Using mFISH and mBAND for bioindication of internal α-radiation, Radiats. Biol. Radioecol., 2016, vol. 56, no. 2, pp. 156–162.
Degteva, M.O., Shagina, N.B., Vorobiova, M.I., et al., Contemporary understanding of radioactive contamination of the Techa River in 1949–1956, Radiats. Biol. Radioecol., 2016, vol. 56, no. 5, pp. 523–534. https://doi.org/10.7868/S0869803116050039
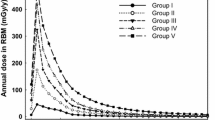
Degteva, M.O., Napier, B.A., Tolstykh, E.I., et al., Enhancements in the Techa River dosimetry system: TRDS-2016D code for reconstruction of deterministic estimates of dose from environmental exposures, Health Phys., 2019, vol. 117, no. 4, pp. 378–387. https://doi.org/10.1097/HP.0000000000001067
Davis, F.G., Krestinina, L.Yu., Preston, D., et al., Solid cancer incidence in the techa river incidence cohort: 1956–2007, Radiat. Res., 2015, vol. 184, pp. 56–65. https://doi.org/10.1667/RR14023.1
Krestinina, L.Yu., Davis, F.G., Schonfeld, S., et al., Leukaemia incidence in the Techa River Cohort: 1953–2007, Br. J. Cancer, 2013, vol. 109, pp. 2886–2893. https://doi.org/10.1038/bjc.2013.614
Schonfeld, S.J., Krestinina, L.Yu., Epifanova, S.B., et al., Solid cancer mortality in the Techa River Cohort (1950–2007), Radiat. Res., 2013, vol. 179, no. 2, pp. 183–189. https://doi.org/10.1667/RR2932.1
Napier, B.A., Degteva, M.O., Shagina, N.B., and Anspaugh, L.R., Uncertainty analysis for the techa river dosimetry system, Med. Radiol. Radiat. Saf., 2013, vol. 58, no. 1, pp. 5–28.
Napier, B.A., Eslinger, P.W., Tolstykh, E.I., et al., Calculations of individual doses for techa river cohort members exposed to atmospheric radioiodine from Mayak releases, J. Environ. Radioact., 2017, vols. 178–179, pp. 156–167. https://doi.org/10.1016/j.jenvrad.2017.08.013
Degteva, M.O., Tolstykh, E.I., Suslova, K.G., et al., Analysis of the results of long-lived radionuclide body burden monitoring in residents of the Urals region, Radiat. Hygiene, 2018, vol. 11, no. 3, pp. 30–39. https://doi.org/10.21514/1998-426X-2018-11-3-30-39
Shagina, N.B., Tolstykh, E.I., Degteva, M.O., et al., Age and gender specific biokinetic model for strontium in humans, J. Radiol. Prot., 2015, vol. 35, no. 1, pp. 87–127. https://doi.org/10.1088/0952-4746/35/1/87
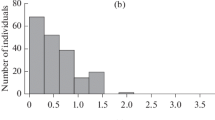
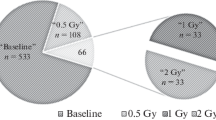
Vozilova, A.V., Shagina, N.B., Degteva, M.O., et al., Preliminary FISH-based assessment of external dose for residents exposed on the Techa River, Radiat. Res., 2012, vol. 177, no. 1, pp. 84–91.
Vozilova, A.V., Shagina, N.B., Degteva, M.O., et al., FISH analysis of translocations induced by chronic exposure to Sr radioisotopes: second set of analysis of the Techa River Cohort, Radiat. Prot. Dosim., 2014, vol. 159, nos. 1–4, pp. 34–37. https://doi.org/10.1093/rpd/ncu131
Degteva, M.O., Shishkina, E.A., Tolstykh, E.I., et al., Application of EPR and FISH methods to dose reconstruction for people exposed in the Techa River area, Radiats. Biol. Radioecol., 2017, vol. 57, no. 1, pp. 30–41. https://doi.org/10.7868/S0869803117010052
Bains, I., Thiébaut, R., Yates, A.J., and Callard, R., Quantifying thymic export: combining models of naive T cell proliferation and TCR excision circle dynamics gives an explicit measure of thymic output, J. Immunol., 2009, vol. 183, no. 7, pp. 4329–4336. https://doi.org/10.4049/jimmunol.0900743
Steinmann, G.G., Klaus, B., and Muller-Hermelink, H.K., The involution of the ageing human thymic epithelium is independent of puberty. A morphometric study, Scand. J. Immunol., 1985, vol. 22, pp. 563–575. https://doi.org/10.1111/j.1365-3083.1985.tb01916.x
Braber, I., Mugwagwa, T., Vrisekoop, N., et al., Maintenance of peripheral naive T cells is sustained by thymus output in mice but not humans, Immunity, 2012, vol. 36, no. 2, pp. 288–297. https://doi.org/10.1016/j.immuni.2012.02.006
Britanova, O.V., Shugay, M., Merzlyak, E.M., et al., Dynamics of individual T cell repertoires: from cord blood to centenarians, J. Immunol., 2016, vol. 196, no. 12, pp. 5005–5013. https://doi.org/10.4049/jimmunol.1600005
Naumova, E.N., Gorski, J., and Naumov, Y.N., Two compensatory pathways maintain long-term stability and diversity in CD8 T cell memory repertoires, J. Immunol., 2009, vol. 183, no. 4, pp. 2851–2858. https://doi.org/10.4049/jimmunol.0900162
Yoshida, K., Cologne, J.B., Cordova, K., et al., Aging-related changes in human T-cell repertoire over 20 years delineated by deep sequencing of peripheral T-cell receptors, Exp. Gerontol., 2017, vol. 1, no. 96, pp. 29–37. https://doi.org/10.1016/j.exger.2017.05.015
Linton, P.J. and Dorshkind, K., Age-related changes in lymphocyte development and function, Nat. Immunol., 2004, vol. 5, no. 2, pp. 133–139. https://doi.org/10.1038/ni1033
Sambandam, A., Bell, J.J., Schwarz, B.A., et al., Progenitor migration to the thymus and T cell lineage commitment, Immunol. Res., 2008, vol. 42, nos. 1–3, pp. 65–74. https://doi.org/10.1007/s12026-008-8035-z
Müller, L. and Pawelec, G., Introduction to ageing of the adaptive immune system, in Immunosenescence: Psychological and Behavioural Determinants, Bosch, J.A., Phillips, A.C., and Lord, J.M., Eds., New York: Springer, 2013, pp. 17–33.
Krueger, A., Zietara, N., and Lyszkiewicz, M., T-cell development by the numbers, Trends Immunol., 2017, vol. 38, no. 2, pp. 128–139. https://doi.org/10.1016/j.it.2016.10.007
Zlotoff, D.A. and Bhandoola, A., Hematopoietic progenitor migration to the adult thymus, Ann. N.Y. Acad. Sci., 2011, vol. 1217, pp. 122–138. https://doi.org/10.1111/j.1749-6632.2010.05881.x
Wagner, U., Schatz, A., Baerwald, C., and Rossol., M., Brief report: deficient thymic output in rheumatoid arthritis despite abundance of prethymic progenitors, Arthritis Rheum., 2013, vol. 65, no. 10, pp. 2567–2572. https://doi.org/10.1002/art.38058
Kyoizumi, S., Kubo, Y., Kajimura, J., et al., Age-associated changes in the differentiation potentials of human circulating hematopoietic progenitors to T- or NK-lineage cells, J. Immunol., 2013, vol. 190, no. 12, pp. 6164–6172. https://doi.org/10.4049/jimmunol.1203189
Bains, I., Mathematical modelling of T cell homeostasis, Ph.D. Thesis, London: University College, 2010. http://discovery.ucl.ac.uk/20159/1/20159.pdf. Accessed August 29, 2019.
Stewart, F.A., Akleyev, A.V., Hauer-Jensen, M., et al., Early and Late Effects of Radiation in Normal Tissues and Organs—Threshold Doses for Tissue Reactions in a Radiation Protection Context, Annals of the ICRP, Elsevier, 2012.
Yassai, M.B., Naumov, Y.N., Naumova, E.N., and Gorski, J., A clonotype nomenclature for T cell receptors, Immunogenetics, 2009, vol. 61, no. 7, pp. 493–502. https://doi.org/10.1007/s00251-009-0383-x
Broere, F., Apasov, S.G., Sitkovsky, M.V., and van Eden, W., T cell subsets and T cell-mediated immunity, in Principles of Immunopharmacology, Nijkamp, F.P. and Parnham, M., Eds., Birkhauser, Basel: Springer, 2011, pp. 15–27.
De Boer, R.J. and Perelson, A.S., Quantification T lymphocyte turnover, J. Theor. Biol., 2013, vol. 327, pp. 45–87. https://doi.org/10.1016/j.jtbi.2012.12.025
Douek, D.C., Betts, M.R., and Hill, B.J., Evidence for increased T cell turnover and decreased thymic output in HIV infection, J. Immunol., 2001, vol. 167, no. 11, pp. 6663–6668. https://doi.org/10.4049/jimmunol.167.11.6663
Bloemers, B.L., Bont, L., de Weger, R.A., et al., Decreased thymic output accounts for decreased naive T cell numbers in children with down syndrome, J. Immunol., 2011, vol. 186, no. 7, pp. 4500–4507. https://doi.org/10.4049/jimmunol.1001700
Flores, K., Li, J., Sempowski, G.D., et al., Analysis of the human thymic perivascular space during aging, J. Clinic. Investigate, 1999, vol. 104, no. 8, pp. 1031–1039. https://doi.org/10.1172/jci7558
Ye, P. and Kirschner, D.E., Measuring emigration of human thymocytes by T-cell receptor excision circles, Crit. Rev. Immunol., 2002, vol. 22, nos. 5–6, pp. 483–497.
Ye, P. and Kirschner, D.E., Reevaluation of T cell receptor excision circles as a measure of human recent thymic emigrants, J. Immunol., 2002, vol. 168, no. 10, pp. 4968–4979. https://doi.org/10.4049/jimmunol.168.10.4968
Haines, C.J., Giffon, T.D., Lu, L.S., et al., Human CD4+ T cell recent thymic emigrants are identified by protein tyrosine kinase 7 and have reduced immune function, J. Exp. Med., 2009, vol. 206, no. 2, pp. 275–285. https://doi.org/10.1084/jem.20080996
Aguilera-Sandoval, C.R., Yang, O.O., Jojic, N., et al., Supranormal thymic output up to 2 decades after HIV-1 infection, AIDS, 2016, vol. 30, no. 5, pp. 701–711. https://doi.org/10.1097/QAD.0000000000001010.
Fink, P.J., The biology of recent thymic emigrants, Annu Rev. Immunol., 2013, vol. 31, pp. 31–50. https://doi.org/10.1146/annurev-immunol-032712-100010
Vrisekoop, N., den Braber, I., de Boer, A.B., et al., Sparse production but preferential incorporation of recently produced naive T cells in the human peripheral pool., Proc. Natl. Acad. Sci. U. S. A., 2008, vol. 105, no. 16, pp. 6115–6120. https://doi.org/10.1073/pnas.0709713105
Naylor, K., Li, G., Vallejo, A.N., et al., The influence of age on T cell generation and TCR diversity, J. Immunol., 2005, vol. 174, no. 11, pp. 7446–7452. https://doi.org/10.4049/jimmunol.174.11.7446
Abdulahad, W.H., van der Geld, Y.M., Stegeman, C.A., et al., Persistent expansion of CD4+ effector memory T cells in Wegener’s granulomatosis, Kidney Int., 2006, vol. 70, no. 5, pp. 938–947. https://doi.org/10.1038/sj.ki.5001670
Huenecke, S., Behl, M., Fadler, C., et al., Age-matched lymphocyte subpopulation reference values in childhood and adolescence: application of exponential regression analysis, Eur. J. Haematol., 2008, vol. 80, no. 6, pp. 532–539. https://doi.org/10.1111/j.1600-0609.2008.01052.x
Yan, J., Greer, J.M., Hull, R., et al., The effect of ageing on human lymphocyte subsets: comparison of males and females, Immun. Ageing, 2010, vol. 7, p. 4. https://doi.org/10.1186/1742-4933-7-4
Pido-Lopez, J., Imami, N., and Aspinall, R., Both age and gender affect thymic output: more recent thymic migrants in females than males as they age, Clin. Exp. Immunol., 2001, vol. 125, no. 3, pp. 409–413. https://doi.org/10.1046/j.1365-2249.2001.01640.x
Ahmed, R., Bevan, M.J., Reiner, S.L., and Fearon, D.T., The precursors of memory: models and controversies, Nat. Rev. Immunol., 2009, vol. 9, pp. 662–668. https://doi.org/10.1038/nri2619
Lugli, E., Dominguez, M.H., Gattinoni, L., et al., Superior T memory stem cell persistence supports long-lived T cell memory, J. Clin. Invest., 2013, vol. 123, no. 2, pp. 594–599. https://doi.org/10.1172/JCI66327
Costa, Del Amo, P., Lahoz-Beneytez, J., Boelen, L., et al., Human TSCM cell dynamics in vivo are compatible with long-lived immunological memory and stemness, PLoS Biol., 2018, vol. 16, no. 6. e2005523. https://doi.org/10.1371/journal.pbio.2005523
Robins, H.S., Campregher, P.V., Srivastava, S.K., et al., Comprehensive assessment of T-cell receptor beta-chain diversity in alphabeta T cells, Blood, 2009, vol. 114, no. 19, pp. 4099–4107. https://doi.org/10.1182/blood-2009-04-217604
Fisher, R.A., Corbet, A.S., and Williams, C.B., The relation between the number of species and the number of individuals in a random sample of an animal population, J. Anim. Ecol., 1943, vol. 12, pp. 42–58. https://doi.org/10.2307/1411
Naumov, Y.N., Naumova, E.N., Clute, S.C., et al., Complex T cell memory repertoires participate in recall responses at extremes of antigenic load, Immunology, 2006, vol. 177, no. 3, pp. 2006–2014. https://doi.org/10.4049/jimmunol.177.3.2006
Naumov, Y.N., Naumova, E.N., Yassai, M.B., and Gorski, J., Selective T cell expansion during aging of CD8 memory repertoires to influenza revealed by modeling, J. Immunol., 2011, vol. 186, no. 11, pp. 6617–6624. https://doi.org/10.4049/jimmunol.1100091
Johnson, P.L., Yates, A.J., Goronzy, J.J., and Antia, R., Peripheral selection rather than thymic involution explains sudden contraction in naive CD4 T-cell diversity with age, Proc. Natl. Acad. Sci. U. S. A., 2012, vol. 109, no. 52, pp. 21432–21437. https://doi.org/10.1073/pnas.1209283110
Venturi, V., Quigley, M.F., Greenaway, H.Y., et al., A mechanism for TCR sharing between T cell subsets and individuals revealed by pyrosequencing, J. Immunol., 2011, vol. 186, no. 7, pp. 4285–4294. https://doi.org/10.4049/jimmunol.1003898
Naumov, Y.N., Naumova, E.N., Hogan, K.T., et al., A fractal clonotype distribution in the CD8+ memory T cell repertoire could optimize potential for immune responses, J. Immunol., 2003, vol. 170, no. 8, pp. 3994–4001. https://doi.org/10.4049/jimmunol.170.8.3994
Meier, J., Roberts, C., Avent, K., et al., Fractal organization of the human T cell repertoire in health and after stem cell transplantation, Biol. Blood. Marrow Transplant., 2013, vol. 19, no. 3, pp. 366–377. https://doi.org/10.1016/j.bbmt.2012.12.004
Bolkhovskaya, O.V., Zorin, D.Yu., and Ivanchenko, M.V., Assessing T cell clonal size distribution: a non-parametric approach, arXiv:1404.6790 [q-bio.QM], August 21, 2014. https://arxiv.org/pdf/1404.6790.pdf. Accessed August 29, 2019.
Robins, H.S., Srivastava, S.K., Campregher, P.V., et al., Overlap and effective size of the human CD8+ T cell receptor repertoire, Sci. Transl. Med., 2010, vol. 2, no. 47, pp. 47–64. https://doi.org/10.1126/scitranslmed.3001442
Trepel, F., Number and distribution of lymphocytes in man. A critical analysis, Klin Wochenschr., vol. 52, pp. 511–515 (quoted by [38]).
Di Rosa, F. and Gebhardt, T., Bone marrow T cells and the integrated functions of recirculating and tissue-resident memory T cells, Front. Immunol., 2016, vol. 7, no. 51. https://doi.org/10.3389/fimmu.2016.00051
Attaf, M., Huseby, E., and Sewell, A.K., αβ T cell receptors as predictors of health and disease, Cell Mol. Immunol., 2015, vol. 12, no. 4, pp. 391–399. https://doi.org/10.1038/cmi.2014.134
Schick, P.F., Trepel, F., Lehmann-Brockhaus, E., et al., Autotransfusion of 3H-cytidine-labelled blood lymphocytes in patient with Hodgkin’s and non-Hodgkin patient. I. Limitation of the method, Acta Haematol., 1975, vol. 53, no. 4, pp. 193–205. https://doi.org/10.1159/000208184
Pabst, R., The spleen in lymphocyte migration, Immunol. Today, 1988, vol. 9, no. 2, pp. 43–45. https://doi.org/10.1016/0167-5699(88)91258-3
Zhao, E., Xu, H., Wang, L., et al., Bone marrow and the control of immunity, Cell Mol. Immunol., 2012, vol. 9, no. 1, pp. 11–19. https://doi.org/10.1038/cmi.2011.47
Parretta, E., Cassese, G., Santoni, A., et al., Kinetics of in vivo proliferation and death of memory and naive CD8 T cells: parameter estimation based on 5-bromo-2'-deoxyuridine incorporation in spleen, lymph nodes, and bone marrow, J. Immunol., 2008, vol. 180, no. 11, pp. 7230–7239. https://www.ncbi.nlm.nih.gov/pubmed/18490722.https://doi.org/10.1038/icb.2016.47
Di Rosa, F., T-lymphocyte interaction with stromal, bone and hematopoietic cells in the bone marrow, Immunol. Cell Biol., 2009, vol. 87, no. 1, pp. 20–29. https://doi.org/10.1038/icb.2008.84
Di Rosa, F. and Pabst, R., The bone marrow: a nest for migratory memory T cells, Trends Immunol., 2005, vol. 26, no. 7, pp. 360–366. https://doi.org/10.1016/j.it.2005.04.011
Britanova, O.V., Putintseva, E.V., Shugay, M., et al., Age-related decrease in TCR repertoire diversity measured with deep and normalized sequence profiling, J. Immunol., 2014, vol. 192, no. 6, pp. 2689–2698. https://doi.org/10.4049/jimmunol.1302064
Tolstykh, E.I., Degteva, M.O., Vozilova, A.V., and Akleyev, A.V., Interpretation of FISH results in the case of nonuniform internal radiation exposure of human body with the use of model approach, Hum. Genet., 2019, vol. 55, no. 10, pp. 1227–1233. https://doi.org/10.1134/S1022795419100132
ICRP-67. Age-dependent dose to members of the public from intake of radionuclides. Part 2: Ingestion dose coefficients, ICRP Publication 67, Ann. ICRP, 1993, vol. 23, nos. 3/4, pp. 1–167.
Suslova, K.G., Khokhryakov, V.F., Sokolova, A.B., and Miller, S.C., 238Pu: a review of the biokinetics, dosimetry, and implications for human exposures, Health Phys., 2012, vol. 102, no. 3, pp. 251–262. https://doi.org/10.1097/hp.0b013e318234899a
Suslova, K.G., Sokolova, A.B., Krahenbuhl, M.P., and Miller, S.C., The effects of smoking and lung health on the organ retention of different plutonium compounds in the Mayak PA workers, Radiat. Res., 2009, vol. 171, no. 3, pp. 302–309. https://doi.org/10.1667/0033-7587-171.3.302
Racanelli, V. and Rehermann, B., The liver as an immunological organ, Hepatology, 2006, vol. 43, pp. 54–62. https://doi.org/10.1002/hep.21060
Lalor, P.F., Shields, P., Grant, A.J., and Adams, D.H., Recruitment of lymphocytes to the human liver, Immunol. Cell Biol., 2002, vol. 80, pp. 52–64. http://www. nature.com/icb/journal/v80/n1/full/icb20027a.html-aff1.https://doi.org/10.1046/j.1440-1711.2002.01062.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Statement of Compliance with Standards of Research Involving Humans as Subjects
This article does not contain any studies involving human participants performed by any of the authors.
Additional information
Translated by A. Barkhash
Rights and permissions
About this article
Cite this article
Tolstykh, E.I., Vozilova, A.V., Degteva, M.O. et al. Concept of T-Cell Genus as a Basis for Analysis of the Results of Cytogenetic Studies after Local Bone Marrow Exposure. Biol Bull Russ Acad Sci 47, 1495–1506 (2020). https://doi.org/10.1134/S1062359020110151
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1062359020110151