Abstract
Introduction: The length of stay (LOS) in patients admitted to intensive care units (ICUs) is influenced by the clinical history of the patient, so the main factors affecting clinical outcome are logicalcandidates to be predictors of LOS. Since there is still limited information about which factors can influence LOS in these patients, we undertook this observational study in Italian hospitals.
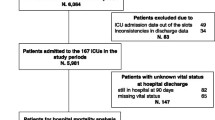
Materials and methods: From 1 August to 31 October 2001 we enrolled a maximum of 10 consecutive patients admitted to ICUs in 16 Italian hospitals. The following information was recorded from each patient: date of admission; APACHE II score on admission; active sepsis and/or septic shock on admission; sepsis and/or septic shock developed during the stay in ICU; Glasgow coma scale on the third day; date and clinical outcome upon discharge from the hospital (alive or dead).
Results: In the study 131 patients were enrolled; 31 (23.7%) had active sepsis upon admission to ICU and 10 (7.6%) had septic shock; 12 (9.2%) developed sepsis during hospitalization and 12 (9.2%) developed septic shock. At the end of the study, 101 patients were alive and 30 had died. The overall mean LOS was 12 days. The mean LOS was 18.3 days for the subgroup with sepsis and 8.3 days in the subgroup without sepsis. Sepsis was the only factor that significantly influenced the LOS (P = 0.016).
Conclusions: Our study was aimed to analyse the factors that influence the LOS in ICU patients and found that among the variables that affected LOS, sepsis had the greatest impact. Other studies had evaluated the impact of some variables on LOS and identified sepsis and infection as a determinant prolonging LOS.
Similar content being viewed by others
References
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985; 13: 818–29.
Digiovine B, Chenoweth C, Watts C, Higgins M. The attributable mortality and costs of primary nosocomial bloodstream infec-tions in the intensive care unit. Am J Respir Crit Care Med 1999; 160: 976–81
Girou E, Stephan F, Novara A, Safar M, Fagon JY. Risk factors and outcome of nosocomial infections: results of a matched case-control study of ICU patients. Am J Respir Crit Care Med 1998; 157(Pt 1): 1151–8.
Pittet D, Tarara D, Wenzel RP. Nosocomial bloodstream infection in critically ill patients. Excess length of stay, extra costs, and at-tributable mortality. JAMA 1994; 271: 1598–601
Eisele B, Lamy M, Thijs LG, Keinecke HO, Schuster HP, Matthias FR et al. Antithrombin III in patients with severe sepsis. A rand-omized, placebo-controlled, double-blind multicenter trial plus a meta-analysis on all randomized, placebo-controlled, double-blind trials with antithrombin III in severe sepsis. Intens Care Med 1998; 24: 663–72.
Pitimana-aree S, Forrest D, Brown G, Anis A, Wang XH, Dodek P. Implementation of a clinical practice guideline for stress ulcer prophylaxis increases appropriateness and decreases cost of care. Intens Care Med 1998; 24: 217–23.
Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann Intern Med 1993; 118: 201–10.
Messori A, Trippoli S, Vaiani M, Gorini M, Corrado A. Bleeding and pneumonia in intensive care patients given ranitidine and sucralfate for prevention of stress ulcer: meta-analysis of ran-domised controlled trials. BMJ 2000; 321: 1103–6.
Abraham E, Matthay MA, Dinarello CA, Vincent JT, Cohen J, Opal SM et al. Consensus conference definitions for sepsis, sep-tic shock, acute lung injury, and acute respiratory distress syn-drome: time for a reevaluation. Crit Care Med 2000; 28: 232–5.
Fagon JY, Chastre J, Vuagnat A, Gibert G. Nosocomial pneumo-nia and mortality among patients in intensive care units. JAMA 1996; 275: 866–9.
Cook DJ, Reeve BK, Guyatt GH, Heyland DK, Griffith LE, Buck-ingham L et al. Stress c in critically ill patients. Resolving discord-ant meta-analyses. JAMA 1996; 275: 308–14.
Author information
Authors and Affiliations
Additional information
c/o Azienda Ospedaliera Careggi
c/o Azienda Ospedaliera Careggi
c/o Azienda Ospedaliera Careggi
c/o Azienda Ospedaliera Careggi
c/o Azienda Ospedaliera Careggi
c/o Azienda Ospedaliera Careggi
c/o Azienda Ospedaliera Careggi
Rights and permissions
About this article
Cite this article
Vacca, F., Vaiani, M., Messori, A. et al. Factors influencing the length of hospitalisation in intensive care units: a prospective observational study. Pharm World Sci 26, 263–267 (2004). https://doi.org/10.1023/B:PHAR.0000042880.12835.4e
Issue Date:
DOI: https://doi.org/10.1023/B:PHAR.0000042880.12835.4e