Abstract
Method: Structured telephone interviews and pre- and post-intervention prescription data.
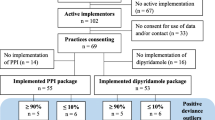
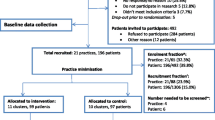
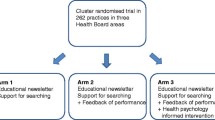
Setting: Additional study in an RCT to rationalize prescribing in primary care, addressing groups of pharmacists and doctors. Representatives of 61 primary care practice groups in the Netherlands.
Main outcome measures: Identification and evaluation of primary care practice group characteristics related to changes in prescribing. These characteristics were evaluated by estimation of incidence rate ratios (Poisson regression).
Results: Of practice groups 40 representatives (66%) participated in our study. Three characteristics were found to be most relevant for stratification: the purpose of the practice groups (whether they participated in information exchange (n=14) or binding consensus on pharmacotherapy (n=26)), the use of a formulary (22 practice groups did and 18 groups did not) and the use of feedback data (22 groups did and 18 groups did not). These characteristics strongly modified the effect of the program on prescribing behaviour. While the overall effect of the program was to significantly reduce the prescribing of the targeted drugs, this change was not consistent in all strata.
Conclusion: Assessment of the characteristics of practice groups made it possible to define factors to be used for a stratified randomization of practice groups which in retrospect indeed modified the effect of an educational intervention directed to change prescribing. Such pre-randomization assessments can be a useful tool in interventions designed to improve practice patterns in groups of physicians.
Similar content being viewed by others
References
Kernan WN, Viscoli CM, Makuch RW et al. Stratified randomization for clinical trials. J Clin Epidemiol 1999; 52: 19–26.
Diwan VK, Eriksson B, Sterky G, Tomson G. Randomization by group in studying the effect of drug information in primary care. Int J Epidemiol 1992; 21: 124–30.
Donner A. An empirical study of cluster randomization. Int J Epidemiol 1982; 11: 283–6.
Donner A, Donald A. Analysis of data arising from a stratified design with the cluster as unit of randomization. Stat Med 1987; 6: 43–52.
Donner A. Sample size requirements for stratified cluster randomization designs [published erratum appears in Stat Med 1997; 16: 2927-8]. Stat Med 1992; 11: 743–50.
Shipley MJ, Smith PG, Dramaix M. Calculation of power for matched pair studies when randomization is by group. Int J Epidemiol 1989; 18: 457–61.
van Eijk MEC, Avorn J, Porsius AJ, de Boer A. Reducing prescribing of highly anticholinergic antidepressants for elderly people: randomised trial of group versus individual academic detailing.Br Med J 2001; 322: 654.
Szecsenyi J, Andres E, Bahrs O et al. Evaluation of a training program for moderators of panel doctor quality circles: a progress assessment. Z Arztl Fortbild (Jena) 1995; 89: 419–23.
Guptill PB, Graham FE. Continuing education activities of physicians in solo and group practice: report on a pilot study. Med Care 1976; 14: 173–80.
Paes AHP. Pharmacists and general practitioners in consultations? Contacts in primary health care. Utrecht, The Netherlands: University of Utrecht 1989.
Mulder J, Kroon Ad, Duijn J. Farmacotherapie-overleg in Nederland 1: hoe staat het ervoor en hoe kan het beter? [Peer review groups in the Netherlands, state of the art and how can it be improved?] Pharm Weekbl 1993; 128: 1236–1241.
Mulder J, Kroon Ad, Duijn J. Farmacotherapie-overleg in Nederland 2: hoe staat het ervoor en hoe kan het beter? [Peer review groups in the Netherlands, state of the art and how can it be improved?] Pharm Weekbl 1993; 128: 1312–16.
Grol R. Quality improvement by peer review in primary care: a practical guide. Qual Health Care 1994; 3: 147–52.
de Vries CS. Collaboration in healthcare, the tango to drug safety [PhD]. Groningen, The Netherlands: University of Groningen 1998.
Deen JBH. Verslag van farmacotherapie-gesprekken in Culemborg [Report of primary care practice meetings.] Pharm Weekbl 1974; 109: 585–9.
Rogers EM. Diffusion of innovations. Third edition. New York: Free Press 1995.
NHS Centre for reviews and dissemination. Getting evidence into practice. York: University of York, February 1999. Volume 5 number 1.
Grant J, Stanton F. The effectiveness of continuing professional development. Milton Keynes: Joint Centre for Education in Medicine, The Open University, March 1998.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Eijk, M.E., Paes, A.H., Porsius, A. et al. Pre-randomization decisions and group stratification in a randomized controlled trial to improve prescribing. Pharm World Sci 26, 227–231 (2004). https://doi.org/10.1023/B:PHAR.0000035888.60709.43
Issue Date:
DOI: https://doi.org/10.1023/B:PHAR.0000035888.60709.43