Abstract
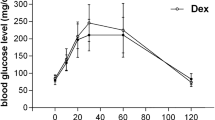
The present study aims to confirm if the moderate-intensity swimming has successful glycemic control and non-toxic oxidative stress levels and to verify the influence on pancreatic adaptations, embryo implantation, and placental efficiency. Female Wistar rats were randomly distributed to obtain mildly diabetic by streptozotocin induction at birth and the non-diabetic females given vehicle. At adulthood, pregnant rats were put at random into sedentary non-diabetic rats (ND); exercise non-diabetic rats (NDEx); sedentary diabetic rats (D); and exercise diabetic rats (DEx). The rats of the groups submitted to moderate intensity carried loads equivalent to 4% of body weight. On day 17 of gestational day, all rats were submitted to oral glucose tolerance test (OGTT). Next day (GD18), the rats were anesthetized and killed to count implantation sites and to collect placentas, blood, and muscle samples for biochemical biomarkers and pancreas for immunohistochemical analysis. The moderate exercise used was not sufficient to stimulate the aerobic pathway but presented positive results on glucose metabolism, lower embryo postimplantation loss, and pancreatic morphology compared with the sedentary diabetic group. However, the DEx group showed muscular damage, decreased antioxidant defense, and lipid peroxidation. Thus, the moderate-intensity exercise reduces glycemic levels during OGTT and causes no damage to non-diabetic rats related to other analyzed parameters in this study. The exercised diabetic rats present better glycemic metabolism in OGTT, islet pancreatic morphology, and embryofetal development. However, it is necessary an adjustment in this exercise intensity to improve the effectiveness of aerobic training for reduction of maternal muscular and lipid membrane damages.






Similar content being viewed by others
Data Availability
Data supporting findings are presented within the manuscript.
Change history
19 February 2021
A Correction to this paper has been published: https://doi.org/10.1007/s43032-021-00490-w
References
World Health Organization (WHO). Diabetes. 2018. https://www.who.int/news-room/fact-sheets/detail/diabetes.
International Diabetes Federation (IDF). IDF Diabetes Atlas Ninth edition 2019. 2019. https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html.
Bequer L, Gómez T, Molina JL, Álvarez A, Chaviano C, Clapés S. Experimental diabetes impairs maternal reproductive performance in pregnant Wistar rats and their offspring. Syst Biol Reprod Med. 2018;64(1):60–70. https://doi.org/10.1080/19396368.2017.1395928.
Iessi I, Sinzato Y, Gallego F, Nielsen J, Damasceno D. Effect of diabetes on circulating pancreatic hormones in pregnant rats and their offspring. Horm Metab Res. 2016;48(10):682–6. https://doi.org/10.1055/s-0042-114039.
Gallego FQ, Sinzato YK, Miranda CA, Iessi IL, Dallaqua B, Volpato GT, et al. Pancreatic islet response to diabetes during pregnancy in rats. Life Sci. 2018;214:1–10. https://doi.org/10.1016/j.lfs.2018.10.046.
Gallego FQ, Miranda CA, Sinzato YK, Iessi IL, Dallaqua B, Pando RH, et al. Temporal analysis of distribution pattern of islet cells and antioxidant enzymes for diabetes onset in postnatal critical development window in rats. Life Sci. 2019;226:57–67. https://doi.org/10.1016/j.lfs.2019.03.061.
Hauschildt AT, Corá LA, Volpato GT, Sinzato YK, Damasceno DC, Américo MF. Mild diabetes: long-term effects on gastric motility evaluated in rats. Int J Exp Pathol. 2018;99(1):29–37. https://doi.org/10.1111/iep.12262.
Eriksson UJ. Congenital anomalies in diabetic pregnancy. Seminars in Fetal & Neonatal Medicine. 2008:1–9.
Holemans K, Aerts L, Van Assche FA. Lifetime consequences of abnormal fetal pancreatic development. J Physiol. 2003;547:11–20. https://doi.org/10.1113/jphysiol.2002.036582.
Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065–79. https://doi.org/10.2337/dc16-1728.
Hopkins SA, Artal R. The role of exercise in reducing the risks of gestational diabetes mellitus women’s health 2013; 9(6):569–581. https://doi.org/10.2217/whe.13.52.
Vigelsø A, Andersen NB, Dela F. The relationship between skeletal muscle mitochondrial citrate synthase activity and whole body oxygen uptake adaptations in response to exercise training. Int J Physiol Pathophysiol Pharmacol. 2014;6:84–101.
Larsen S, Nielsen J, Hansen CN, Nielsen LB, Wibrand F, Stride N, et al. Biomarkers of mitochondrial content in skeletal muscle of healthy young human subjects. J Physiol. 2012;590:3349–60. https://doi.org/10.1113/jphysiol.2012.230185.
Blomstrand E, Radegran G, Saltin B. Maximum rate of oxygen uptake by human skeletal mus- cle in relation to maximal activities of enzymes in the Krebs cycle. J Physiol. 1997;501:455–60. https://doi.org/10.1111/j.1469-7793.1997.455bn.x.
Byllund AC, Bjuro T, Cederblad G, Holm J, Lundholm K, Sjostroom M, et al. Physical training in man. Skeletal muscle metabolism in relation to muscle morphology and running ability. Eur J Appl Physiol Occup Physiol. 1977;36:151–69. https://doi.org/10.1007/BF00421747.
Halliwell B, Gutteridge JMC. Oxidative stress: adaptation, damage, repair and death. Oxford: Oxford University Press; 1998.
Baird MF, Graham SM, Baker JS, Bickerstaff GF. Creatine-kinase- and exercise-related muscle damage implications for muscle performance and recovery. J Nutr Metab. 2012;2012:960363. https://doi.org/10.1155/2012/96036310.1155/2012/960363.
Close GL, Kayani A, Vasilaki A, McArdle A. Skeletal muscle damage with exercise and aging. Sports Med. 2005;35(5):413–27. https://doi.org/10.2165/00007256-200535050-00004.
Lopez-Soldado I, Herrera E. Different diabetogenic response to moderate doses of streptozotocin in pregnant rats, and its long-term consequences in the offspring. Exp Diabesity Res. 2003;4:107–18. https://doi.org/10.1155/EDR.2003.107.
Leandro CG, Fidalgo M, Bento-Santos A, Falcão-Tebas F, Vasconcelos D, Castro RM, et al. Maternal moderate physical training during pregnancy attenuates the effects of a low-protein diet on the impaired secretion of insulin in rats: potential role for compensation of insulin resistance and preventing gestational diabetes mellitus. J Biomed Biotechnol. 2012;2012:1–7. https://doi.org/10.1155/2012/805418.
Lazo-Osório RA, Pereira R, Christofani JS, Russo AK, Machado M, Ribeiro W, et al. Effect of physical training on metabolic responses of pregnant rats submitted to swimming under termal stress. J Res Med Sci. 2009;14(4):223–30.
Volpato GT, Damasceno DC, Campos KE, Rocha R, Rudge MVC, Calderon IMP. Avaliação do efeito do exercício físico no metabolismo de ratas diabéticas prenhes. Rev Bras Med Esporte. 2006;12(5):229–33. https://doi.org/10.1590/S1517-86922006000500001.
Volpato GT, Damasceno DC, Kempinas WG, Rudge MV, Calderon IM. Effect of exercise on the reproductive outcome and fetal development of diabetic rats. Reprod BioMed Online. 2009;19(6):852–8. https://doi.org/10.1016/j.rbmo.2009.09.027.
Damasceno DC, Silva HP, Vaz GF, Vasques-Silva FA, Calderon IMP, Rudge MVC, et al. Diabetic rats exercise prior to and during pregnancy: maternal reproductive outcome, biochemical profile, and frequency of fetal anomalies. Reprod Sci. 2013;20(7):730–8. https://doi.org/10.1177/1933719112461186.
Volpato GT, Damasceno DC, Sinzato YK, Ribeiro VM, Rudge MVC, Calderon IMP. Oxidative stress status and placental implications in diabetic rats undergoing swimming exercise after embryonic implantation. Reprod Sci. 2015;22(5):602–8. https://doi.org/10.1177/1933719114556485.
Netto AO, Gelaleti RB, Corvino SB, Serrano RG, Hernándezb SC, Volpato GT, et al. Small-for-pregnancy-age rats submitted to exercise: DNA damage in mothers and newborns, measured by the comet assay. Mutat Res Gen Tox En. 2018;835:11–5. https://doi.org/10.1016/j.mrgentox.2018.08.006.
Corvino SB, Damasceno DC, Sinzato YK, Netto AO, Macedo NCD, Zambrano E, et al. Comparative analysis of two different models of swimming applied to pregnant rats born small for pregnant age. An Acad Bras Cienc. 2017;89(1):223–30. https://doi.org/10.1590/0001-3765201720160285.
Netto AO, Macedo NCD, Gallego FQ, Sinzato YK, Volpato GT, Damasceno DC. Evaluation of anaerobic threshold in non-pregnant and pregnant rats. An Acad Bras Cienc. 2017;89(4):2749–56. https://doi.org/10.1590/0001-3765201720170199.
Netto AO, Macedo NCD, Gallego FQ, Sinzato YK, Volpato GT, Zambrano E, et al. Impact of different exercise intensities on pregnant rats and on their offspring. An Acad Bras Cienc. 2020;92(4) (in press).
Sinzato YK, Damasceno DC, Laufer-Amorim R, Rodrigues MM, Oshiiwa M, Taylor KN, et al. Plasma concentrations and placental immunostaining of interleukin-10 and tumor necrosis factor-α as predictors of alterations in the embryo-fetal organism and the placental development of diabetic rats. Braz J Med Biol Res. 2011;44:206–11. https://doi.org/10.1590/s0100-879x2011007500015.
Sinzato YK, Volpato GT, Iessi IL, Bueno A, Calderon IMP, Rudge MV, et al. Neonatally induced mild diabetes in rats and its effect on maternal, placental, and fetal parameters. Exp Diabetes Res. 2012;2012:1–7. https://doi.org/10.1155/2012/108163.
Tai MM. A mathematical model for the determination of total area under glucose tolerance and other metabolic curves. Diabetes Care. 1994;17:152–4. https://doi.org/10.2337/diacare.17.2.152.
Soares TS, Andreolla AP, Miranda CA, Klöppel E, Rodrigues LS, Moraes- Souza RQ, et al. Effect of the induction of transgenerational obesity on maternal-fetal parameters. Syst Biol Reprod Med 2018; 64:51–59. https://doi.org/10.1080/19396368.2017.1410866.
de Souza MSS, Sinzato YK, Lima PHO, Calderon IMP, Damasceno DC. Oxidative stress status and lipid profiles of diabetic pregnant rats exposed to cigarette smoke. Reprod BioMed Online. 2010;20(4):547–52. https://doi.org/10.1016/j.rbmo.2010.01.002.
Alp PR, Newsholme EA, Zammit VA. Activities of citrate synthase and NAD+ linked and NADP+ linked isocitrate dehydrogenase in muscle from vertebrates and invertebrates. Biochem J. 1976;154:689–700. https://doi.org/10.1042/bj1540689.
Hayward CE, Lean S, Sibley CP, Jones RL, Wareing M, Greenwood SL, et al. Placental adaptation: what can we learn from birth weight: placental weight ratio? Front Physiol. 2016;7:28. https://doi.org/10.3389/fphys.2016.00028.
Damasceno DC, Kempinas WDG, Volpato GT, Consonni M, Rudge MVC, Paumgartten FJR. Anomalias congênitas - estudos experimetais. Editora Médica: Botucatu; 2008.
Nascimento SL, Surita FG, Cecatti JG. Physical exercise during pregnancy: a systematic review. Curr Opin Obstet Gynecol. 2012;24(6):387–94. https://doi.org/10.1097/GCO.0b013e328359f131.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50. https://doi.org/10.1056/NEJM200105033441801.
Kim HJ, Park JY, Oh SL, Kim YA, So B, Seong JK, et al. Effect of treadmill exercise on interleukin-15 expression and glucose tolerance in zucker diabetic fatty rats. Diabetes Metab J. 2013;37:358–64. https://doi.org/10.4093/dmj.2013.37.5.358.
Mota CSA, Ribeiro C, Araújo GG, de Araújo MB, Manchado-Gobatto FB, Voltarelli FA, et al. Exercise training in the aerobic/anaerobic metabolic transition prevents glucose intolerance in alloxan- treated rats. BMC Endocr Disord. 2008;8:11. https://doi.org/10.1186/1472-6823-8-11.
Butler AE, Cao-Minh L, Galasso R, Rizza RA, Corradin A, Cobelli C, et al. Adaptive changes in pancreatic beta cell fractional area and beta cell turnover in human pregnancy. Diabetology. 2010;53:2167–76. https://doi.org/10.1007/s00125-010-1809-6.
Rawal S, Huang HH, Novikova L, Hamedi T, Smirnova IV, Stehno-Bittel L. Effect of exercise on pancreatic islets in Zucker diabetic fatty rats. J Diabetes Metab. 2013;10:1–7. https://doi.org/10.4172/2155-6156.
Park S, Hong SM, Sung SR. Exendin-4 and exercise promotes β-cell function and mass through IRS2 induction in islets of diabetic rats. Life Sci. 2008;82:503–11. https://doi.org/10.1016/j.lfs.2007.
Burgos-Morón E, Abad-Jiménez Z, Marañón AM, Iannantuoni F, Escribano-López I, López-Domènech S, et al. Relationship between oxidative stress, ER stress, and inflammation in type 2 diabetes: the battle continues. J Clin Med. 2019;8(9):1385. https://doi.org/10.3390/jcm8091385.
Wang J, Wang H. Oxidative stress in pancreatic beta cell regeneration. Oxidative Med Cell Longev. 2017;2017:1–9. https://doi.org/10.1155/2017/1930261.
Pingitore A, Lima GP, Mastorci F, Quinones A, Iervasi G, Vassalle C. Exercise and oxidative stress: potential effects of antioxidant dietary strategies in sports. Nutrition. 2015;31(7–8):916–22. https://doi.org/10.1016/j.nut.2015.02.005.
Powers SK, Jackson MJ. Exercise-induced oxidative stress: cellular mechanisms and impact on muscle force production. Physiol Rev. 2008;88:1243–76. https://doi.org/10.1152/physrev.00031.2007.
Dillard CJ, Litov RE, Savin WM, Dumelin EE, Tappel AL. Effects of exercise, vitamin E, ozone on pulmonary function and lipid peroxidation. J Appl Physiol. 1978;45:927–32. https://doi.org/10.1152/jappl.1978.45.6.927.
Davies KJ, Quintanilha AT, Brooks GA, Packer L. Free radicals and tissue damage produced by exercise. Biochem Biophys Res Commun. 1982;107:1198–205. https://doi.org/10.1016/s0006-291x(82)80124-1.
Duthie GG, Robertson JD, Maughan RJ, Morrice PC. Blood antioxidant status and erythrocyte lipid peroxidation following distance running. Arch Biochem Biophys. 1990;282:78–83. https://doi.org/10.1016/0003-9861(90)90089-h.
de Oliveira DM, Dourado GKZS, Cesar TB. Hesperidin associated with continuous and interval swimming improved biochemical and oxidative biomarkers in rats. J Int Soc Sports Nutr. 2013;10(27):1–7. https://doi.org/10.1186/1550-2783-10-27.
Levay EA, Govic A, Hazi A, Flannery G, Christianson J, Drugan RC, et al. Endocrine and immunological correlates of behaviorally identified swim stress resilient and vulnerable rats. Brain Behav Immun. 2006;20(5):488–97. https://doi.org/10.1016/j.bbi.2005.10.004.
Ferry A, Picard F, Duvallet A, Weill B, Rieu M. Changes in blood leukocyte populations induced by acute maximal and chronic submaximal exercise. Eur J Appl Physiol. 1990;59(6):435–42. https://doi.org/10.1007/BF02388625.
Walsh NP, Gleeson M, Shephard RJ, et al. Position statement. Part one: Immune function and exercise. Exer Immunol Rev. 2011;17:6–63.
Sachdev S, Davies KJ. Production, detection, and adaptive responses to free radicals in exercise. Free Radic Biol Med. 2008;44(2):215–23. https://doi.org/10.1016/j.freeradbiomed.2007.07.019.
Perales M, Valenzuela PL, Barakat R, Cordero Y, Peláez M, López C, et al. Gestational exercise and maternal and child health: effects until delivery and at post-natal follow-up. J Clin Med. 2020;9(2):E379. https://doi.org/10.3390/jcm9020379.
Adesegun D, Cai C, Sivak A, Chari R, Davenport MH. Prenatal exercise and pre-gestational diseases: a systematic review and meta-analysis. J Obst Gynaecol Can. 2019;41(8):1134–43. https://doi.org/10.1016/j.jogc.2018.10.007.
Acknowledgments
The authors are thankful to the staff of the Laboratory for Experimental Research in Gynecology and Obstetrics, especially to Talisia Moreto, Carlos Roberto Lima, Vitor Souza, and Danilo Chaguri for the excellent technical assistance. They are also grateful to Dr. Carlos Eduardo Meirelles for providing us the structure of the swimming tanks and for making of the anesthesia machine, and to the Dr. José Eduardo Corrente for assistance with statistical analysis.
Funding
This study was supported by grants from FAPESP/Brazil in most of the study at Nathália C. D. Macedo, as part of her thesis (Fellowship-Process Number 2013/23478-3).
Author information
Authors and Affiliations
Contributions
NCDM, GTV, and DCD conceived and designed the experiments. NCDM, FQG, and AON collected the experimental data. NCDM, ILI, FQG, and DCD analyzed and interpreted data. ILI, FQG, YKS, GTV, EZ, and DCD drafted the article and revised it critically for important intellectual content. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of Interests
The authors confirm that they have no conflict of interest.
Code Availability (Software Application or Custom Code)
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article was updated to correct the affiliation numbers in the author display.
Rights and permissions
About this article
Cite this article
Macedo, N.C.D., Iessi, I.L., Gallego, F.Q. et al. Swimming Program on Mildly Diabetic Rats in Pregnancy. Reprod. Sci. 28, 2223–2235 (2021). https://doi.org/10.1007/s43032-021-00462-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00462-0