Abstract
Aims
The aim of this study was to compare the results of laparoscopic splenectomy (LS) with open splenectomy (OS) in children at a tertiary care referral institute in North India.
Methods
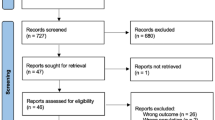
The electronic medical records of all children who had undergone non-emergent splenectomies between July 2014 and December 2019 at our centre were reviewed retrospectively. Patients undergoing splenectomies for trauma or portal hypertension were excluded. During the period from July 2014 to June 2016, splenectomy was performed by an open technique. From July 2016 onwards, all splenectomy procedures were performed laparoscopically. Demographic features, indications for splenectomy, operative time, estimated blood loss, spleen weight, need for conversion, length of stay, time to oral feeds and requirement for analgesia were recorded. Data for children undergoing LS were compared with those undergoing OS.
Results
Between July 2014 and June 2016, 20 children underwent OS. Between July 2016 and November 2019, 16 children underwent LS. The groups were similar in age and sex; hereditary spherocytosis was the commonest indication in both the groups. Operating time was longer in the LS group (186 ± 20.4 min vs 136 ± 12.2 min; P < 0.05), but blood loss and complication rates were similar. Two (12.5%) conversions were necessary, primarily due to spleen size. Children undergoing LS had a shorter length of stay (3.4 ± 0.6 vs 6.8 ± 1.2 days; P < 0.05), shorter time to oral feeds (0.5 vs 2.5 days; P < 0.05), and lesser requirement for analgesia.
Conclusions
LS is feasible and safe in children. It is superior to OS with regard to cosmesis, duration of postoperative analgesia, duration of hospital stay, and recovery of bowel function. However, operating time for LS is longer than OS at our centre currently.



Similar content being viewed by others
References
Thibault C, Mamazza J, Letourneau R et al (1992) Laparoscopic splenectomy: operative technique and preliminary report. Surg Laparosc Endosc 2:248–255
Tulman S, Holcomb GW, Karamanoukian HL et al (1993) Laparoscopic splenectomy. J Pediatr Surg 28:689–692
Feng S, Qiu Y, Li X, Yang H, Wang C, Yang J et al (2016) Laparoscopic versus open splenectomy in children: a systematic review and meta-analysis. Pediatr Surg Int 32:253–259
Farah RA, Rogers ZR, Thompson WR et al (1997) Comparison of laparoscopic and open splenectomy in children with hematologic disorders. J Pediatr 131:41–46
Rescorla FJ, Breitfeld PP, West KW et al (1998) A case-controlled comparison of open and laparoscopic splenectomy in children. Surgery 124:670–675
Qureshi FG, Ergun O, Sandulache VC et al (2005) Laparoscopic splenectomy in children. JSLS 9:389–392
Kühne T, Blanchette V, Buchanan GR et al (2007) Splenectomy in children with idiopathic thrombocytopenic purpura: a prospective study of 134 children from the Intercontinental Childhood ITP Study Group. Pediatr Blood Cancer 49(6):829–834
Goers T, Panepinto J, DeBaun M et al (2008) Laparoscopic versus open abdominal surgery in children with sickle cell disease is associated with a shorter hospital stay. Pediatr Blood Cancer 50:603–606
Alwabari A, Parida L, Al-Salem AH (2009) Laparoscopic splenectomy and/or cholecystectomy for children with sickle cell disease. Pediatr Surg Int 25:417–421
Lesher AP, Kalpatthi R, Glenn JB et al (2009) Outcome of splenectomy in children younger than 4 years with sickle cell disease. J Pediatr Surg 44(6):1134–1138
Zhu J, Ye H, Wang Y et al (2011) Laparoscopic versus open pediatric splenectomy for massive splenomegaly. Surg Innov 18(4):349–353
Wood JH, Partrick DA, Hays T et al (2011) Contemporary pediatric splenectomy: continuing controversies. Pediatr Surg Int 27(11):1165–1171
Hassan ME, Al AK (2014) Massive splenomegaly in children: laparoscopic versus open splenectomy. JSLS 18(3):1–5
Fachin CG, Amado F, Romaniello G et al (2019) Open versus laparoscopic splenectomies in children: a comparative study performed at a public hospital in Brazil. J Laparoendosc Adv Surg Tech A 29(10):1357–1361
Fitzgerald PG, Langer JC, Cameron BH et al (1996) Pediatric laparoscopic splenectomy using the lateral approach. Surg Endosc 10:859–861
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Delaitre B (1995) Laparoscopic splenectomy: the “hanged spleen” technique. Surg Endosc 9:528–529
Trias M, Targarona EM, Balagué C (1996) Laparoscopic splenectomy: an evolving technique. A comparison between anterior and lateral approaches. Surg Endosc 10:387–388
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AM, AG and RH. The first draft of the manuscript was written by AM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was waived by the ethics committee of the institute in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Rights and permissions
About this article
Cite this article
Mandelia, A., Gupta, A., Haldar, R. et al. Laparoscopic splenectomy in children: experience from a tertiary care referral institute in North India. J Ped Endosc Surg 2, 139–144 (2020). https://doi.org/10.1007/s42804-020-00066-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42804-020-00066-6