Abstract
Background
Different MRI parameters have been studied for evaluating thyroid nodules. Diffusion-weighted imaging (DWI) and T2 imaging sequences with considerable efficacy in evaluating soft tissue tumors merit further assessment for thyroid nodule investigation.
Method
We evaluated incidental thyroid nodules (ITNs) reported on head and neck MRI studies. The T2 signal intensity (SI), T2 signal intensity ratio (SIR), Z value, and apparent diffusion coefficient (ADC) values of the thyroid nodule were obtained for every patient. The patients were referred to the radiology department for the thyroid nodule ultrasound study. Finally, 33 participants (37 thyroid nodules) who were scheduled for fine needle aspiration and cytology (FNAC) were enrolled. Regarding the FNAC results, the nodules were divided into malignant and benign groups. The two groups’ MRI parameters were compared using a two samples independent t test, and the cutoff values were estimated by analyzing the receiver operating characteristics plot.
Results
The T2 signal intensities, SIR, Z values, and ADC values were significantly higher in the benign group than malignant. The cutoff points of 230 (AUC = 0.759), 3.38 (AUC = 0.754), 37 (AUC = 0.759), and 1.73 (AUC = .690) were obtained for T2 values, SIR, Z values, and ADC values, respectively.
Conclusion
T2, SIR, Z, and ADC values are reliable for discriminating benign from malignant ITNs. However, further studies with a larger sample size are needed to provide more accurate mean values, identify outliers, and reduce confounding factors and bias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although thyroid nodules are amongst the most common medical issues worldwide, differentiating benign nodules from malignant ones is not desirable. Ultrasound is the most commonly used imaging approach to thyroid nodules, and fine needle aspiration and cytology (FNAC) of the nodule is the gold standard in determining these nodules’ underlying pathology. However, FNAC is sometimes inconclusive in results, and surgical excisional biopsy and lobar or total thyroidectomy would be the final choice that may be a great burden of physical and psychological stress for the patient and a wastage in medical expenses [1]. The situation becomes more complicated in incidental thyroid nodules (ITNs) found in head and neck and upper mediastinum imaging studies [2]. Regarding the fact that ITNs may present either a benign or malignant behavior, reporting these nodules on magnetic resonance imaging (MRI) or computed tomography (CT) studies without any particular suggestion or diagnosis may lead to over-diagnosis or under-diagnosis of the malignancies [3,4,5].
Therefore, the better the radiologist could distinguish the pattern and nature of ITNs, the more effective medical investigations could be applied to identify the underlying pathology, and the less the patients encounter anxiety and uncertainty [4]. Although the guidelines for the management of ITNs on MRI recommend some properties to determine whether the nodules need more investigations or not, still no definite approach to discriminate malignancy from benignity on MRI of thyroid nodules is recommended [6]. Moreover, research indicates that these guidelines may not be reliable as some thyroid malignancies incidentally found in MRI may be missed [3]. On the other hand, many benign ITNs that need no further evaluation due to these guidelines have to undergo more evaluation by ultrasound study and FNAC [4]. These facts highlight the need for more studies on the properties of ITNs on MRI to attain proper criteria for differentiating malignant from benign ones.
Recent studies in MRI of thyroid nodules have candidate T2 protocols and diffusion-weighted imaging (DWI) for differentiating benign from malignant lesions [7,8,9,10]. T2-weighted MRI has been used to assess various soft tissue pathologies, especially for estimating the probability of malignancy in lymph nodes and prostate [11]. It is also suggested as a potential modality to assess thyroid nodules [8]. DWI, which is reported quantitatively by apparent diffusion coefficient value (ADCV), is a functional MRI based on the Brownian movement of water molecules through the tissue. DWI can provide crucial information from the molecular profile and microarchitecture of the studied organ or pathologic tissue. Consequently, DWI is a useful tool in evaluating head and neck tumors, salivary gland tumors, and cervical lymphadenopathy [12] and is also suggested for assessing thyroid nodules [13].
In this study, we sought to define a scale for reporting thyroid nodules in MRIs and determine whether the T2 and ADC values could predict the nature of thyroid nodules. We also hypothesized that a small proportion of thyroid nodules undergo the subsequent evaluation and that certain factors related to the MRI characteristics of the nodule influence workup.
Thus, we performed an MRI in T2 and DWI sequences for patients with thyroid nodules suspicious of malignancy diagnosed by ultrasound and then compared the MRI values with the FNAC report.
Patients and Methods
Patient Selection
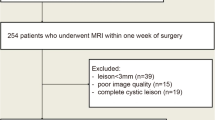
This prospective study was conducted in Al-Zahra Hospital, Isfahan city, Iran, from 20 October 2018 to 15 December 2020. This study was approved by the committee of biomedical research ethics of our department.
Before including patients in the study, informed consent was obtained. The study aims, procedures, and risks were completely defined for the patients. It is essential to mention that this study had no interference with standard care for patients diagnosed with thyroid nodules.
In this study, subjects were patients who underwent head and neck MRI for any reason. To obtain a study limited to patients with ITNs, a patient was excluded if the imaging study was performed to evaluate symptoms or signs related to the thyroid gland or if the patient had a history of thyroid nodules or had undergone a prior evaluation of the thyroid gland, such as a previous thyroid ultrasound study or thyroid biopsy. The patients were referred to the radiology department for the thyroid nodule ultrasound study. According to the American College of Radiology (ACR) Thyroid Imaging Reporting and Data System (TI-RADS), based on the size and structure of the nodules in ultrasound study, the TI-RADS score is indicative of either fallow-up or FNAC of the nodule. In this study, we needed to determine the nature of the nodules through FNAC and pathologic studies. Therefore, we only included patients with TI-RADS scores indicative of FNA, which is shown in (Table 1, Fig. 1).
Ultrasonography Protocol
The ultrasound study was performed by an expert radiologist with 10 years of experience in thyroid US using the same ultrasound scanner (siemens-healthineers, ACUSON NX) for all patients with a 15MHZ linear transducer. The examination was performed in transverse and longitudinal views to investigate for any thyroid nodule, abnormal lymph node, tumor infiltration, metastasis, and other soft tissue pathologies differentially diagnosed of the thyroid nodule. The ultrasound study was reported according to the American College of radiologists’ TIRAD system. The radiologist was blinded to the patient’s MRI results.
MRI Protocol
MRI was performed by a 1.5 T scanner (Philips medical system, Ingenia ambition 1.5TX, the Netherlands) using a neck coil. All patients were studied by the same mentioned machine and coil.
The MRI protocol included axial T2-weighted (T2WI) (repetition time/echo time (TR/TE): 2904 ms/80 ms, slice thickness: 3 mm; gap 0.5 mm; (number of excitation) NEX: 4; field of view (FOV): 16 cm; matrix: 320 × 224) and DWI on axial plane on diffusion gradient b factor = 800 (TR/TE: 5000 ms/minimum; FOV: 16 cm; NEX: 4; matrix: 128 × 128; slice thickness: 4 mm; and gap = 0.5 mm.
Quantitative Image Analysis
Two radiologists with 10 and 8 years of experience in head and neck imaging who were blinded to the patient’s ultrasound reports measured signal intensities of thyroid nodules and paraspinal muscles on T2-weighted imaging by placing a circular ROI cursor. In thyroid nodules, circular ROI covered the entire nodule at the largest cross-section area without including artifacts or cystic portions of the nodule. Signal intensity ratio (SIR) on T2-weighted was measured as a ratio of signal intensity of the thyroid nodule on T2-weighted to that of paraspinal muscle.
Also, signal intensities of background noise on T2-weighted were measured.
The Z value is calculated as following:
The DWI sequence was performed to obtain the ADC values of each patient’s thyroid nodule by analyzing the ADC map for every individual (Figs. 2 and 3).
A 57-year-old man with papillary thyroid nodule and nodal metastasis: a axial T2-weighted image shows small hyperintense thyroid nodule in the right lobe with central calcification (arrow), with TIRADS4 in sonography (not shown here). b Axial T2-weighted image of same patient with lymphadenopathy (arrow) in the right side of the neck. c, d Axial DWI and ADC images of lymph adenopathy show restriction on DWI (c) and ADC value 1.14 × 10–3 mm.2/s (d) (arrows)
Ultrasound-Guided FNAC Study
Under sterile conditions after ultrasound-guided localization of the nodule and local anesthesia, a 21-gauge or 22-gauge was used to perform aspiration biopsy. The specimen was fixed and stained for histopathology study. An expert interventional radiologist performed the FNAC of the thyroid nodule for each patient in the intervention section of the AL-Zahra hospital’s radiology department, Isfahan, Iran, and the samples were transported to the pathology department. All samples were initially classified according to the recommended six diagnostic categories (DCs) of the Bethesda system for reporting thyroid cytopathology (TBSRTC), including nondiagnostic or unsatisfactory (ND/UNS; I), benign (B; II), atypia of undetermined significance or follicular lesion of undetermined significance (AUS/FLUS; III), suspicious for follicular neoplasm or follicular neoplasm (SFN/FN; IV), suspicious for malignancy (SM; V), and malignant (M; VI). The cytological study was performed independently by a pathologist, an expert in thyroid cytology. The pathologist was blinded to the patient’s MRI and ultrasound results.
Statistical Analysis
Quantitative variables were reported as mean, median, standard deviation, and interquartile ranges. Qualitative variables were reported as numbers and percentages. The quantitative data were assessed for being normal by the Kolmogorov–Smirnov test and Q-Q plot. The comparison of quantitative variables between the malignant and benign groups was made by 2 samples independent t test. The diagnostic values of thyroid nodule signal intensity on T2-weighted, T2 SIR, Z value, ADC value of thyroid nodule, and the cutoff points of each parameter in the malignant and benign group were determined by analyzing the receiver operating characteristics (ROC). Sensitivity, specificity, positive likelihood ratio (LR +), and accuracy of the cutoff points were also determined. The area under the curve was reported with a 95% confidence interval.
Results
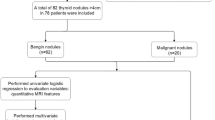
A total of 37 solid thyroid nodules were identified in 33 patients. Twenty-two nodules were benign, and 15 nodules were malignant. Mean, median, standard deviation, and interquartile ranges of patients’ age, thyroid nodule signal intensity on T2-weighted, T2 SIR, Z value, and ADC value of thyroid nodule in benign and malignant nodules were summarized in Table 2.
The mean age was 50.05 years, and in the malignant and benign groups was 50.18 and 49.87 years, respectively, without any significant differences between the groups (p = 0.943). The sex distribution was not significantly different between the groups as well.
The T2-weighted signal intensity of thyroid nodule, T2 SIR, ADC value of thyroid nodule, and Z value were compared between the malignant and benign groups. The mean T2-weighted signal intensity of thyroid nodule, SIR, and Z value were 314 ± 127, 4.21 ± 1.3, and 51 ± 21.2, which were significantly higher in the benign group. P values were 0.001, 0.002, and 0.001, respectively. The ADC value in the benign group was 1.63 ± 0.7 and in the malignant group was 1.26 ± 0.4, which was marginally higher in the benign group (P value 0.08).
On the basis of ROC analysis, the optimal threshold of T2-weighted signal intensity of thyroid nodule for differentiating benign and malignant groups was 230, which was the most accurate (68%), cutoff point with a sensitivity of 68.18%, specificity of 67%, and positive likelihood ratio (LR +) of 2. The area under the curve for this cutoff point was 0.759 (p < 0.01) (Fig. 4a).
Also, the diagnostic value of T2 SIR and Z value were evaluated by ROC, and the results indicated that 3.38 with AUC = 0.754 (p = 0.01) (Fig. 4b) and cutoff point of 37 with AUC = 0.759 (p = 0.01) (Fig. 4c) were the most accurate, specific, and sensitive cutoff point with the highest positive likelihood ratio.
The evaluation of ADC values by ROC indicated that the 1.73 with AUC = 0.690 (p < 0.05) has the greatest accuracy, specificity, and sensitivity, with the highest positive likelihood ratio (LR +) discriminating benign from malignant nodules (Fig. 4d).
Cutoff points of the T2 values, SIR, Z value, and ADC values with specificity, sensitivity, and positive likelihood ratio are summarized in Table 3.
Discussion
Studies evaluating MRI parameters in reporting benign and malignant thyroid lesions have been controversial. T2-weighted MRI always has been a subject of interest for distinguishing malignant from benign lesions, especially in soft tissue tumors [7, 14]. To our best knowledge, there is no study particularly reporting T2 imaging protocol as a reliable method to evaluate thyroid nodules. However, in a study of 181 patients with thyroid nodules, Wang et al. [10] reported that among T1, T2, and ADC protocols, only ADC values of thyroid nodules have diagnostic values. On the other hand, Shi et al. [7] indicated that T2* values of thyroid nodules could be diagnostic and reported a cutoff point of 25.00 ms. Herein, we assessed the diagnostic value of the T2 imaging protocol in thyroid nodules of 37 patients (15 malignant and 22 benign nodules). The results indicated a reliable diagnostic value of the T2 protocol in ITNs with a cutoff point of 230 (AUC of 0.759, sensitivity of 68.18, specificity of 66.67, and LR + of 2.0455).
Moreover, to better assess the competency of T2-weighted MRI in discriminating thyroid nodules, the signal intensity ratio (SIR) was calculated for every nodule, and the cutoff point of 3.38 (AUC of 0.754, sensitivity of 77.27, specificity of 66.67, and LR + of 2.1382) was obtained. This method with higher sensitivity may guarantee the reliability of the T2 imaging protocol in the discrimination of thyroid nodules. In addition to a SIR of the nodules to diminish the background noise effect on interpreting T2 values, we corrected the T2 values of every nodule with noise in the background by calculating the Z values. The results were conclusive for T2 values of thyroid nodules with the cutoff point of 37 (with AUC of 0.759, sensitivity of 68.18, specificity of 66.67, and LR + of 2.0455). These results indicated that the background noise does not significantly affect the estimated cutoff point for T2 values.
DWI protocol is better studied in the field of thyroid malignancies. Although the number of studies purposing DWI as a diagnostic method is far more than the T2 protocol, heterogeneous results and cutoff points increase the need for more investigations to establish these methods [13]. A systematic review and meta-analysis by Chen et al. [13] evaluated studies assessing thyroid nodules by DWI. They concluded that although this imaging method is an accurate way to distinguish malignant and benign nodules, still more investigations are needed to determine a reliable cutoff point and b value for this method. They also explained that the heterogeneous cutoff points reported in different studies are due to different b values utilized in the imaging process. A brief review of studies determining cutoff points for ADC values is listed in Table 4.
As demonstrated, the different b values ranging from 100 to 2000 are co-existent with heterogeneous cutoff points ranging from 0/36 to 2/17. Moreover, the literature’s current state suggests that the highest possible b values in DW imaging would better discriminate between malignant and benign thyroid nodules [13]. Thus, in the present study, the relatively high b value of 800 was applied, and the cutoff point for ADC values was 1.73 (AUC of 0.690, sensitivity of 66.67, specificity of 92.86, and LR + of 9.33). Compared to other studies, ADC values of 1.73 with an AUC of 0.69 indicated a lower accuracy than some of the studies. However, compared to Wu et al. [16], with a b value of 800 and a cutoff point of 1.65 (AUC of 0.63, sensitivity of 53%, and specificity of 71%), our study indicated better accuracy for the cutoff point of 1.73. Linh et al. [17] also reported the AUC of 0.94 with a cutoff point of 1.53, sensitivity of 84%, and specificity of 92%, which shows a considerably higher accuracy that could be explained by a bigger study population than us.
Study Strengths and Limitations
This study used two new equations to better identify thyroid tumors’ malignancy or benignity. These equations (Z and T2 values) could better help radiologists interpret thyroid nodules, especially in doubtful results by single T2 or ADC values. Regarding the COVID-19 pandemic and limitations in resources, we decided to cut the number of participants in half to be able to prepare the best protective equipment and avoid any dangerous contacts for both patients and the research team; thus, due to the limited number of studied patients the risk for accidentally meaningful results is considerable, and we suggest further studies with greater study populations. Further studies with a larger sample size provide more accurate mean values, identify outliers that could skew the data in smaller samples, and provide a smaller margin of error. Furthermore, adjusting potential confounding variables and a larger sample size ensures good generalizability of results.
Conclusion
Our results showed that T2 and ADC values are appropriate for differentiating malignant from benign thyroid nodules. Therefore, we suggest that thyroid nodules’ T2 and ADC values could be appropriate and safe methods for investigating thyroid nodules on MRI. However, further studies with a larger sample size are needed to confirm these findings.
Data Availability
All data will be made available based on reasonable request.
Code Availability
Not applicable.
References
Grani G, Sponziello M, Pecce V, Ramundo V, Durante C. Contemporary thyroid nodule evaluation and management. J Clin Endocrinol Metab. 2020;105(9):2869–83.
Özdemir M, Kavak RP. Incidentally discovered thyroid nodules by routine magnetic resonance imaging of the cervical spine: incidence and clinical significance. Curr Med Imaging. 2020;16(6):677–81.
Bahl M, Sosa JA, Eastwood JD, Hobbs HA, Nelson RC, Hoang JK. Using the 3-tiered system for categorizing workup of incidental thyroid nodules detected on CT, MRI, or PET/CT: how many cancers would be missed? Thyroid. 2014;24(12):1772–8.
Tanpitukpongse TP, Grady AT, Sosa JA, Eastwood JD, Choudhury KR, Hoang JK. Incidental thyroid nodules on CT or MRI: discordance between what we report and what receives workup. Am J Roentgenol. 2015;205(6):1281–7.
Hoang JK, Riofrio A, Bashir MR, Kranz PG, Eastwood JD. High variability in radiologists’ reporting practices for incidental thyroid nodules detected on CT and MRI. AJNR Am J Neuroradiol. 2014;35(6):1190–4.
Hoang JK, Langer JE, Middleton WD, Wu CC, Hammers LW, Cronan JJ, et al. Managing incidental thyroid nodules detected on imaging: white paper of the ACR Incidental Thyroid Findings Committee. J Am Coll Radiol. 2015;12(2):143–50.
Shi R, Yao Q, Wu L, Zhou Q, Lu Q, Gao R, et al. T2* mapping at 3.0T MRI for differentiation of papillary thyroid carcinoma from benign thyroid nodules. J Magn Reson Imaging. 2016;43(4):956–61.
Noda Y, Kanematsu M, Goshima S, Kondo H, Watanabe H, Kawada H, et al. MRI of the thyroid for differential diagnosis of benign thyroid nodules and papillary carcinomas. AJR Am J Roentgenol. 2015;204(3):W332-335.
Aghaghazvini L, Sharifian H, Yazdani N, Hosseiny M, Kooraki S, Pirouzi P, et al. Differentiation between benign and malignant thyroid nodules using diffusion-weighted imaging, a 3-T MRI study. Indian J Radiol Imaging. 2018;28(4):460–4.
Wang H, Wei R, Liu W, Chen Y, Song B. Diagnostic efficacy of multiple MRI parameters in differentiating benign vs. malignant thyroid nodules. BMC Med Imaging. 2018;18:1–9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6278127/. Accessed 2 Jan 2021.
Chavhan GB, Babyn PS, Thomas B, Shroff MM, Haacke EM. Principles, techniques, and applications of T2*-based MR imaging and its special applications. Radiographics. 2009;29(5):1433–49.
Baliyan V, Das CJ, Sharma R, Gupta AK. Diffusion weighted imaging: technique and applications. World J Radiol. 2016;8(9):785–98.
Chen L, Xu J, Bao J, Huang X, Hu X, Xia Y, et al. Diffusion-weighted MRI in differentiating malignant from benign thyroid nodules: a meta-analysis. BMJ Open. 2016;6(1):e008413.
Wu L-M, Chen X-X, Xuan H-Q, Liu Q, Suo S-T, Hu J, et al. Feasibility and preliminary experience of quantitative T2* mapping at 3.0 T for detection and assessment of aggressiveness of prostate cancer. Acad Radiol. 2014;21(8):1020–6.
Bozgeyik Z, Coskun S, Dagli AF, Ozkan Y, Sahpaz F, Ogur E. Diffusion-weighted MR imaging of thyroid nodules. Neuroradiology. 2009;51(3):193.
Wu Y, Yue X, Shen W, Du Y, Yuan Y, Tao X, et al. Diagnostic value of diffusion-weighted MR imaging in thyroid disease: application in differentiating benign from malignant disease. BMC Med Imaging. 2013;13(1):23.
Linh LT, Cuong NN, Hung TV, Hieu NV, Lenh BV, Hue ND, et al. Value of Diffusion weighted MRI with quantitative ADC map in diagnosis of malignant thyroid disease. Diagnostics. 2019;9(4):129.
Shi HF, Feng Q, Qiang JW, Li RK, Wang L, Yu JP. Utility of diffusion-weighted imaging in differentiating malignant from benign thyroid nodules with magnetic resonance imaging and pathologic correlation. J Comput Assist Tomogr. 2013;37(4):505–10.
Ilica AT, Artaş H, Ayan A, Günal A, Emer O, Kilbas Z, et al. Initial experience of 3 tesla apparent diffusion coefficient values in differentiating benign and malignant thyroid nodules. J Magn Reson Imaging. 2013;37(5):1077–82.
Nakahira M, Saito N, Murata S, Sugasawa M, Shimamura Y, Morita K, et al. Quantitative diffusion-weighted magnetic resonance imaging as a powerful adjunct to fine needle aspiration cytology for assessment of thyroid nodules. Am J Otolaryngol. 2012;33(4):408–16.
Mutlu H, Sivrioglu AK, Sonmez G, Velioglu M, Sildiroglu HO, Basekim CC, et al. Role of apparent diffusion coefficient values and diffusion-weighted magnetic resonance imaging in differentiation between benign and malignant thyroid nodules. Clin Imaging. 2012;36(1):1–7.
El-Hariri MA, Gouhar GK, Said NS, Riad MM. Role of diffusion-weighted imaging with ADC mapping and in vivo 1H-MR spectroscopy in thyroid nodules. Egypt J Radiol Nucl Med. 2012;43(2):183–92.
Razek AAKA, Sadek AG, Kombar OR, Elmahdy TE, Nada N. Role of apparent diffusion coefficient values in differentiation between malignant and benign solitary thyroid nodules. Am J Neuroradiol. 2008;29(3):563–8.
Wang Q, Guo Y, Zhang J, Ning H, Zhang X, Lu Y, et al. Diagnostic value of high b-value (2000 s/mm2) DWI for thyroid micronodules. Medicine. 2019;98(10). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6417555/. Accessed 3 Mar 2021.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and data analysis were performed by A. Shayganfar, S. Hajiahmadi, N. Azin, A.M. Ghanei, and P. Hashemi. The first draft of the manuscript was written by S. Hajiahmadi and supervised by A. Shayganfar. All authors commented on previous versions of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
IR.MUI.MED.REC.1398.325.
Consent to Participate
A waiver of informed consent was granted for this prospective study.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shayganfar, A., Azin, N., Hashemi, P. et al. Diagnostic Accuracy of Multiple MRI Parameters in Dealing with Incidental Thyroid Nodules. SN Compr. Clin. Med. 4, 228 (2022). https://doi.org/10.1007/s42399-022-01307-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01307-w