Abstract
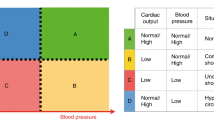
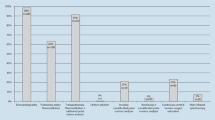
This paper aims to identify hemodynamic and echocardiographic standards in pediatric patients in the Emergency Department. The study design is epidemiological, observational, and cross-sectional. The study was carried out in the Emergency Department of the Baca Ortiz Pediatric Hospital, Quito, Ecuador. Inclusion criteria included pediatric patients from 1 month of age up to 15 years old, both sexes, any ethnic group, critical patients with shock, trauma, or respiratory insufficiency, without previous cardiopulmonary comorbidities. We performed echocardiography, assessing volume, fluid responsiveness, left ventricular systolic function, left ventricle diastolic function, right ventricle systolic function, and pericardium. When it was necessary, doctors administered inotropic or vasoactive drugs to stabilize the patient. The volume responder profile was male sex in 61% of the cases, from zero to 5 years in 93.4% of the cases; the mean heart rate was 126, the MAP of 65, and the CVP of 5.5. The ejection fraction and shortening did show significant variability between the two cohorts, trauma and shock. There was not a correlation between peak aortic flow and mean arterial pressure. For the selected model, sensitivity reached 85.7%, specificity of 91.4%, positive predictive value (VPP) of 66.7%, negative predictive value (VPN) of 96.97%, and 90.5%. In the ejection fraction (EF), those who presented systolic dysfunction had significantly lower values than the patients with diastolic dysfunction and the normal ones; the difference between the patients with systolic dysfunction compared with those without dysfunction was − 24.6%, and between the systolic dysfunction and diastolic was − 27.8%. This is the first report on standard hemodynamic values in echocardiography for critically ill pediatric patients. It needs more research to understand these parameters better, focusing on other etiologies, ethnic groups, and more complex variables. This paper’s general message is to show how non-invasive measures can be used sooner in ED rather than just in critical care. The quality of non-invasive monitoring improves care and patient outcomes, length of stay, and mortality, among other essential factors.
Similar content being viewed by others
Data Availability
Upon request
References
McGovern M. Miletin J. A review of superior vena cava flow measurement in the neonate by functional echocardiography. Acta Paediatr. 2017;106(1):22–9. https://doi.org/10.1111/apa.13584.
Vieillard-Baron A, Millington SJ, Sanfilippo F, et al. A decade of progress in critical care echocardiography: a narrative review [published correction appears in Intensive Care Med. 2019 Apr 15]. Intensive Care Med. 2019;45(6):770–88. https://doi.org/10.1007/s00134-019-05604-2.
Mannarino S, Bulzomì P, Codazzi AC, et al. Inferior vena cava, abdominal aorta, and IVC-to-aorta ratio in healthy Caucasian children: ultrasound Z-scores according to BSA and age. J Cardiol. 2019;74(4):388–93. https://doi.org/10.1016/j.jjcc.2019.02.021.
Musolino AM, Buonsenso D, Massolo AC, Gallo M, Supino MC, Boccuzzi E. Point of care ultrasound in the paediatric acute care setting: getting to the ‘heart’ of respiratory distress [published online ahead of print, 2020 Dec 9]. J Paediatr Child Health. 2020. https://doi.org/10.1111/jpc.15308.
Park DB, Presley BC, Cook T, Hayden GE. Point-of-care ultrasound for pediatric shock. Pediatr Emerg Care. 2015;31(8):591–601. https://doi.org/10.1097/PEC.0000000000000519.
Maw AM, Huebschmann AG, Mould-Millman NK, Dempsey AF, Soni NJ. Point-of-care ultrasound and modernization of the bedside assessment. J Grad Med Educ. 2020;12(6):661–5. https://doi.org/10.4300/JGME-D-20-00216.1.
O’Brien AJ, Brady RM. Point-of-care ultrasound in pediatric emergency medicine. J Paediatr Child Health. 2016;52(2):174–80. https://doi.org/10.1111/jpc.13098.
Potter SK, Griksaitis MJ. The role of point-of-care ultrasound in pediatric acute respiratory distress syndrome: emerging evidence for its use. Ann Transl Med. 2019;7(19):507. https://doi.org/10.21037/atm.2019.07.76.
Miller AF, Arichai P, Gravel CA. et al., Use of cardiac point-of-care ultrasound in the Pediatric Emergency Department [published online ahead of print, 2020 Oct 27]. Pediatr Emerg Care. 2020. https://doi.org/10.1097/PEC.0000000000002271.
Abdalaziz FA, Algebaly HAF, Ismail RI, El-Sherbini SA, Behairy A. The use of bedside echocardiography for measuring cardiac index and systemic vascular resistance in pediatric patients with septic shock. Uso de ecocardiografia junto ao leito para medir índices cardíaco e de resistência vascular sistêmica em pacientes pediátricos com choque séptico. Rev Bras Ter Intens. 2018;30(4):460–70. https://doi.org/10.5935/0103-507X.20180067.
Hardwick JA, Griksaitis MJ. Fifteen-minute consultation: point of care ultrasound in the management of paediatric shock. Arch Dis Childhood - Educ Pract Publ Online First. 2020. https://doi.org/10.1136/archdischild-2019-317972.
Conlon TW, Nishisaki A, Singh Y, et al. Moving beyond the stethoscope: diagnostic point-of-care ultrasound in pediatric practice. Pediatrics. 2019;144(4):e20191402. https://doi.org/10.1542/peds.2019-1402.
Dominguez A, Gaspar HA, Preto M, Ejzenberg FE. Point-of-care lung ultrasound in pediatric critical and emergency care. J Paediatr Child Health. 2018;54(9):945–52. https://doi.org/10.1111/jpc.14067.
Bortcosh W, Shaahinfar A, Sojar S, Klig JE. New directions in point-of-care ultrasound at the crossroads of pediatric emergency and critical care. Curr Opin Pediatr. 2018;30(3):350–8. https://doi.org/10.1097/MOP.0000000000000621.
Yıldızdaş D, Aslan N. A new stethoscope for pediatric intensivists: point-of-care ultrasound. Turk Pediatr Ars. 2020;55(4):345–53. Published 2020 Dec 16. https://doi.org/10.14744/TurkPediatriArs.2020.12499.
Yildizdas D, Aslan N. Ultrasonographic inferior vena cava collapsibility and distensibility indices for detecting the volume status of critically ill pediatric patients. J Ultrason. 2020;20(82):e205–9. https://doi.org/10.15557/JoU.2020.0034.
Pourmand A, Pyle M, Yamane D, Sumon K, Frasure SE. The utility of point-of-care ultrasound in the assessment of volume status in acute and critically ill patients. World J Emerg Med. 2019;10(4):232–8. https://doi.org/10.5847/wjem.j.1920-8642.2019.04.007.
Basu S, Sharron M, Herrera N, Mize M, Cohen J. Point-of-care ultrasound assessment of the inferior vena cava in mechanically ventilated critically ill children. J Ultrasound Med. 2020;39(8):1573–9. https://doi.org/10.1002/jum.15247.
Aslan N, Yildizdas D, Horoz OO, Coban Y, Arslan D, Sertdemir Y. Central venous pressure, global end-diastolic index, and the inferior vena cava collapsibility/distensibility indices to estimate intravascular volume status in critically ill children: A pilot study. Aust Crit Care. 2020;S1036-7314(20):30297–6. https://doi.org/10.1016/j.aucc.2020.08.005.
Mercolini F, Di Leo V, Bordin G, et al. Central venous pressure estimation by ultrasound measurement of inferior vena cava and aorta diameters in pediatric critical patients: an observational study. Pediatr Crit Care Med. 2021;22(1):e1–9. https://doi.org/10.1097/PCC.0000000000002526.
NICE. 2020 Surveillance of intravenous fluid therapy in children and young people in hospital (NICE guideline NG29). London: National Institute for Health and Care Excellence (UK); 2020. Available at https://www.nice.org.uk/guidance/ng29
Acknowledgements
The authors thank Catalina Vásquez Hahn, Santiago Pinto Zaldumbide, Carlos Valencia Calderón, authorities of the Baca Ortiz Pediatric Hospital, Rosa Quiguantar Reascos, and Israel Castro González.
Author information
Authors and Affiliations
Contributions
The contributions are equal for all authors. All authors carried out the protocol design, data collection, statistical analysis, assessment, interpretation of the data, critical analysis, discussion, writing, and final manuscript approval. The corresponding author represents a group of authors.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Subcommittee on Ethics and Research in Human Beings (SEISH) of the Central University of Ecuador approved this research. The legal custodian or the children’s parents gave Informed Consent. Additionally, all parents sign a consent to the admission to the Emergency Department.
Consent for Publication
Parents give their consent for publication, also Hospital Baca Ortiz.
Conflict of Interest
The authors declare no competing interests.
Code Availability
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Fuenmayor-Oramas, F., González-Andrade, F. & la Cueva, X.PD. Moving Toward Non-invasive Hemodynamic and Echocardiographic Monitoring in Critical Pediatric Patients in the Emergency Department: Setting Standards. SN Compr. Clin. Med. 3, 818–825 (2021). https://doi.org/10.1007/s42399-021-00804-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00804-8