Abstract
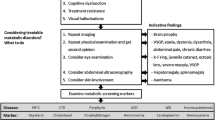
Inborn errors of metabolism (IEM) are individually rare but collectively common disorders, occurring in 1:800 to 1:1000 births. There are more than 1000 known inherited disorders characterized by disruption of metabolic pathways which may present with diverse symptoms affecting any organ at any age, including with psychiatric symptoms mimicking primary psychiatric disorders. This review is intended to help psychiatrists and other physicians suspect an inborn error of metabolism in a patient presenting with psychiatric symptoms. A comprehensive literature review was undertaken, using Index Medicus and resources at the University of Southern California Norris Medical Library to identify specific information for each individual disorder described. Those inborn errors of metabolism most likely to present with psychiatric symptoms primarily impact the brain, acting either directly on biochemical pathways in the central nervous system or indirectly reflecting dysfunction in other organs. Symptoms may occur episodically under stress when metabolic demands are highest or progressively evolve over time reflecting gradual neuropsychiatric deterioration. Cognitive impairment and psychosis appear to be the most frequently reported psychiatric problems. Noting age of onset, patterns of psychiatric presentation, and associated symptoms in other organ systems can increase suspicion and facilitate diagnosis of psychiatric symptoms due to an inborn error of metabolism. Psychiatric problems can be seen with multiple inborn errors of metabolism with associated systemic dysfunction or as isolated symptoms. It is important for physicians to be aware of clues that might increase suspicion of an underlying genetic disorder, and to recognize that consultation with a medical geneticist is recommended for diagnosis and to provide the patient optimal care in either situation.
Similar content being viewed by others
References
Ahrens-Nicklas RC, Slop G, Ficiciolu C. Adolescent presentations of inborn errors of metabolism. J Adolesc Health. 2015;56:477–82. https://doi.org/10.1016/j.jadohealth.2015.01.008.
Saudubray J-M, Garcia-Cazorla A. Inborn errors of metabolism overview: pathophysiology, manifestations, evaluation, and management. Pediatr Clin N Am. 2018;65:179–208.
Mak CM, Lee H-CH, Chan AY-W, Lam C-W. Inborn errors of metabolism and expanded newborn screening: review and update. Crit Rev Clin Lab Sci. 2013;50:142–62.
Estrov Y, Scaglia F, Bodamer OAF. Psychiatric symptoms of inherited metabolic disease. J Inherit Metab Dis. 2000;23:2–6.
Walterfang M, Bonnot O, Mocellin R, Velakoulis D. The neuropsychiatry of inborn errors of metabolism. J Inherit Metab Dis. 2013;36:687–702. https://doi.org/10.1007/s10545-013-9618-y Epub 2013 May 23.
Gambello MJ, Li H. Current strategies for the treatment of inborn errors of metabolism. J Genet Genomics. 2018;45:61–70.
Horvath GA, Stowe RM, Ferreira CR, Blau D. Clinical and biochemical footprints of inherited metabolic diseases. III Psychiatric presentations. Mol Genet Metab. 2020;130:1–6.
Demily C, Sedel F. Psychiatric manifestations of treatable hereditary metabolic disorders in adults. Ann General Psychiatry. 2014;13:27–35.
Trakadis YJ, Fulginiti V, Walterfang M. Inborn errors of metabolism associated with psychosis: literature review and case-control study using exome data from 5090 adult individuals. J Inherit Metab Dis. 2018;41:613–21. https://doi.org/10.1007/s10545-017-0023-9.
Bonnot O, Herrera PM, Tordjman S, Walterfang M. Secondary psychosis induced by metabolic disorders. Front Neurosci. 2015;9:177. https://doi.org/10.3389/fnins.2015.00177.
Sriretnakumar V, Harripaul R, Vincent JB, Kennedy JL, So J. Enrichment of pathogenic variants in genes associated with inborn errors of metabolism in psychiatric populations. Am J Med Genet. 2019;180B:46–54.
Nia S. Psychiatric signs and symptoms in treatable inborn errors of metabolism. J Neurol. 2014;261(Suppl 2):S559–68.
El-Hattab AW. Inborn errors of metabolism. Clin Perinatol. 2015;42:413–39.
Simon NG, Herkes GK. The neurologic manifestations of the acute porphyrias. J Clin Neurosci. 2011;18:1147–53.
Bonkovsky HL, Maddukuri VC, Yazici C, Anderson KE, Bissell DM, Bloomer JR, et al. Acute prophyrias in the USA: features of 108 subjects from porphyrias consortium. Am J Med. 2014;127:1233–41. https://doi.org/10.1016/j.amjmed.2014.06.036 Epub 2014 Jul 10.
Manceau H, Gouya L, Puy H. Acute hepatic and erythropoietic porphyrias: from ALA syntheses 1 and 2 to new molecular bases and treatments. Curr Opin Hematol. 2017;24:198–207.
Ellencweig N, Schoenfeld N, Zemishlany Z. Acute intermittent porphyria: psychosis as the only clinical manifestation. Israel J Psychiatry Relat Sci. 2006;43:52–6.
Holroyd S, Seward RL. Psychotropic drugs in acute intermittent porphyria. Clin Pharmacol Ther. 1999;66:323–5.
Wu F, Wang J, Pu C, Qiao L, Jiang C. Wilson’s disease: a comprehensive review of the molecular mechanisms. Int J Mol Sci. 2015;16:6419–31. https://doi.org/10.3390/ijms16036419.
Lutsenko S. Modifying factors and phenotypic diversity in Wilson’s disease. Ann N Y Acad Sci. 2014;1315:56–63. https://doi.org/10.1111/nyas.12420 Epub 2014 Apr 4.
Rosencrantz R, Schilsky M. Wilson disease: pathogenesis and clinical considerations in diagnosis and treatment. Semin Liver Dis. 2011;31:245–59.
Zimbrean PC, Schilsky ML. Psychiatric aspects of Wilson disease: a review. Gen Hosp Psychiatry. 2014;36:53–62. https://doi.org/10.1016/j.genhosppsych.2013.08.007 Epub 2013 Oct 9.
Dening TR, Berrios GE. Wilson’s disease: a longitudinal study of psychiatric symptoms. Biol Psychiatry. 1990;28:255–65.
Valentino PL, Roberts EA, Beer S, Miloh T, Arnon R, Vittorio JM, Schilsky ML. Management of Wilson disease diagnosed in infancy: an appraisal of available experience to generate discussion. J Pediatr Gastroenterol Nut 2020; 70:547–54. https://doi.org/10.1097/MPG0000000000002608.
Poujois A, Devedjian JC, Moreau C, Devos D, Chaine P, Woimant F, et al. Bioavailable trace metals in neurological diseases. Curr Treat Options Neurol. 2016;18:46. ISSN 1092-8480. https://doi.org/10.1007/s11940-016-0426-1.
Weiss KH, Schäfer M, Gotthardt DN, Angerer A, Mogler C, Schirmacher P, et al. Outcome and development of symptoms after orthotopic liver transplantation for Wilson disease. Clin Transpl. 2013;27:914–22. https://doi.org/10.1111/ctr.12259 Epub 2013 Oct 9.
Srinivas K, Sinha S, Taly AB, Prashanth LK, Arunodaya GR, Janardhana Reddy YC, et al. Dominant psychiatric manifestations in Wilson’s disease: a diagnostic and therapeutic challenge. J Neurol Sci. 2008;266:104–8 Epub 2007 Sep 27.
Svetel M, Potrebić A, Pekmezović T, Tomić A, Kresojević N, Jesić R, et al. Neuropsychiatric aspects of treated Wilson’s disease. Parkinsonism Relat Disord. 2009;15:772–5.
Bone A, Kuehl AK, Angelino AF. A neuropsychiatric perspective of phenylketonuria. I: overview of phenylketonuria and its neuropsychiatric sequelae. Psychosomatics. 2012;53:517–23. https://doi.org/10.1016/j.psym.2012.04.010.
Erlich KJ. Case report: neuropsychiatric symptoms in PKU disease. J Pediatr Health Care. 2020;33:718–21.
Pilotto A, Blau N, Leks E, Schulte C, Deuschl C, Zipser C, et al. Cerebrospinal fluid biogenic amines depletion and brain atrophy in adult patients with phenylketonuria. J Inherit Metab Dis. 2019;42:398–406.
Feillet F, Agostoni C. Nutritional issues in treating phenylketonuria. J Inherit Metab Dis. 2010;33:659–64. https://doi.org/10.1007/s10545-010-9043-4 Epub 2010 Feb 12.
Ris MD, Weber AM, Hunt MM, Berry HK, Williams SE, Leslie N. Adult psychosocial outcome in early-treated phenylketonuria. J Inherit Metab Dis. 1997;20:499–508.
Blau N, Longo N. Alternative therapies to address the unmet needs of patients with phenylketonuria. Expert Opin Pharmacother. 2015;16:791–800.
Fowler B. Disorders of homocysteine metabolism. J Inherit Metab Dis. 1997;20:270–85.
Ramakrishnan S, Sulochana KN, Lakshmi S, Selvi R, Angayarkanni N. Biochemistry of homocysteine in health and disease. Indian J Biochem Biophys. 2006;43:275–83.
Watkins D, Rosenblatt DS. Inborn errors of cobalamin absorption and metabolism. Am J Med Genet. 2011;157:33–44. https://doi.org/10.1002/ajmg.c.30288 Epub 2011 Feb 10.
Reif A, Pfuhlmann B, Lesch KP. Homocysteinemia as well as methylenetetrahydrofolate reductase polymorphism are associated with affective psychoses. Prog Neuro-Psychopharmacol Biol Psychiatry. 2005;29:1162–8.
Ryan MM, Sidhu RK, Alexander J, Megerian JT. Homocystinuria presenting as psychosis in an adolescent. J Child Neurol. 2002;17:859–60.
Almuqbil MA, Waisbren SE, Levy HL, Picker JD. Revising the psychiatric phenotype of homocystinuria. Genet Med. 8:1827–31.
Regland B, Germgård T, Gottfries CG, Grenfeldt B, Koch-Schmidt AC. Homozygous thermolabile methylenetetrahydrofolate reductase in schizophrenia-like psychosis. J Neural Transm (Vienna). 1997;104:931–41.
Nazki FH, Sameer AS, Ganaie BA. Folate: metabolism, genes, polymorphisms and associated diseases. Gene. 2014;533:11–20.
Huemer M, Diodato D, Schwahn B, Schiff M, Bandeira A, Benoist J-F, et al. Guidelines for the diagnosis and management of cobalamin-related remethylation disorders cblC, cblD, cblE, cblF, cblG, cblJ and MTHFR deficiency. J Inherit Metab Dis. 2017;40:21–48. https://doi.org/10.1007/ss10545-016-9991-4.
Yadav U, Kumar P, Gupta S, Rai V. Role of MTHFR C677T gene polymorphism in the susceptibility of schizophrenia: an updated meta-analysis. Asian J Psychiatr. 2016;20:41–51. https://doi.org/10.1016/j.ajp.2016.02.002 Epub 2016 Feb 15.
Martinelli D, Deodato F, Dionisi-Vici C. Cobalamin C defect: natural history, pathophysiology, and treatment. J Inherit Metab Dis. 2011;34:127–35. https://doi.org/10.1007/s10545-010-9161-z Epub 2010 Jul 15. Review.
Wang S, Chuan C, Wen B, Zhao Y. Clinical feature and outcome of late-onset cobalamin C disease patients with neuropsychiatric presentations: a Chinese case series. Neuropsychiatr Dis Treat. 2019;15:549–55.
Huemer M, Scholl-Burgi S, Hadaya K, Kern I, Beer R, Seppi K, et al. Three new cases of late-onset cblC defect and review of the literature illustrating when to consider inborn errors of metabolism beyond infancy. Orphanet J Rare Dis. 2014;9:161. https://doi.org/10.1186/s13023-014-0161-1.
Tonini MC, Bignamini V, Mattioli M. Headache and neuropsychiatric disorders in the puerperium: a case report with suspected deficiency of urea cycle enzymes. Neurol Sci. 2011;32(Suppl 1):S157–9. https://doi.org/10.1007/s10072-011-0518-3.
Batshaw ML, Tuchman M, Summar M, Seminara J, Members of the Urea Cycle Disorders Consortium. A longitudinal study of urea cycle disorders. Mol Genet Metab. 2014;113:127–30. https://doi.org/10.1016/j.ymgme.2014.08.001 Epub 2014 Aug 10. Review.
Thurlow VR, Asafu-Adjaye M, Agalou S, Rahman Y. Fatal ammonia toxicity in an adult due to an undiagnosed urea cycle defect: under-recognition of ornithine transcarbamylase deficiency. Ann Clin Biochem. 2010;47:279–81. https://doi.org/10.1258/acb.2010.009250 Epub 2010 Apr 20.
Bigot A, Brunault P, Lavigne C, Feillet F, Odent S, Kaphan E, et al. Psychiatric adult-onset of urea cycle disorders: a case series. Mol Genet Metab Rep. 2017;12:103–9.
Gallagher RC, Lam C, Wong D, Cederbaum S, Sokol RJ. Significant hepatic involvement in patients with ornithine transcarbamylase deficiency. J Pediatr. 2014;164:720–5.
Fassier T, Guffon N, Acquaviva C, D'Amato T, Durand DV, Domenech P. Misdiagnosed post-partum psychosis revealing a late onset urea cycle disorder. Am J Psychiatry. 2010;168:576–80. https://doi.org/10.1176/appi.ajp.2010.10071032.
Gordon N. Ornithine transcarbamylase deficiency: a urea cycle defect. Eur J Paediatr Neurol. 2003;7:115–21.
Kyo M, Mii H, Takekita Y, Tokuhara D, Yazaki M, Nakamori Y, et al. Case of adult-onset type II citrullinemia treated as schizophrenia for a long time. Psychiatry Clin Neurosci. 2015;69:306–7. https://doi.org/10.1111/pcn.12253 Epub 2014 Dec 29.
Sun A. Lysosomal storage disease overview. Ann Transl Med. 2018;6:476. https://doi.org/10.21037/atm.2018.11.39.
Platt FM, d’Azzo A, Davidson BL, Neufeld EF, Tifft CJ. Lysosomal storage diseases. Nat Rev Dis Primers. 2018;4:27. https://doi.org/10.1038/s41572-01809925-4.
Staretz-Chacham O, Choi JH, Wakabayashi K, Lopez G, Sidransky E. Psychiatric and behavioral manifestation of lysosomal storage disorders. Am J Med Genetics Part B. 2010;153B:1253–65.
Holve S, Hu D, McCandless SE. Metachromatic leukodystrophy in the Navajo: fallout of the American-Indian wars of the nineteenth century. Am J Med Genet. 2001;101:203–8.
Van Rappard DF, de Vries ALC, Oostrom KJ, Boelens JJ, Hollak CEM, van der Knapp MJ, et al. Slowly progressive psychiatric symptoms: think metachromatic leukodystrophy. J Am Acad Child Adolesc Psychiatry. 2018;57:74–6.
Hyde TM, Ziegler JC, Weinberger DR. Psychiatric disturbances in metachromatic leukodystrophy: insights into the neurobiology of psychosis. Arch Neurol. 1992;49:401–6.
Strölin M, Krägeloh-Mann I, Kehrer C, Wilke M. Demyelination load as predictor for disease progression in juvenile metachromatic leukodystrophy. Ann Clin Transl Neurol. 2017;4:403–10.
Krägeloh-Mann I, Groeschel S, Kehrer C, Opherk K, Nägele T, Handgretinger R, et al. Juvenile metachromatic leukodystrophy 10 years post-transplant compared with a non-transplanted cohort. Bone Marrow Transplant. 2013;48:369–75.
Van den Broek BTA, Page K, Paviglianiti A, Hol J, Allewelt H, Volt F, et al. Early and late outcomes after cord blood transplantation for pediatric patients with inherited leukodystrophies. Blood Adv. 2018;2:49–60.
McDowell GA, Mules EH, Fabacher P, Shapira E, Blitzer MG. The presence of two different infantile Tay-Sachs disease mutations in a Cajun population. Am J Hum Genet. 1992;S1:1071–7.
Solovyeva VV, Shaimardanova AA, Chulpanova DS, Kitaeva KV, Chakrabarti L, Rizvanov AA. New approaches to Tay-Sachs disease therapy. Front Physiol. 2018;9:1663. https://doi.org/10.3389/fphys.2018.01663 eCollection 2018.
Turkel SB, Levine M. Ultrastructural study of fetal Tay-Sachs disease. Ultrastruct Res. 1976;55:302.
Hurowitz GI, Silver JM, Brin MF, Williams DT, Johnson WG. Neuropsychiatric aspects of adult-onset Tay-Sachs disease: two case reports with several new findings. J Neuropsychiatr Clin Neurosci. 1993;5:30–6.
Benussi A, Alberici A, Premi E, Castiglioni I, Padovani A, Borroni B. Phenotypic heterogeneity of Niemann-Pick disease type C in monozygotic twins. J Neurol. 2015;262:642–7. https://doi.org/10.1007/s00415-014-7619-x Epub 2014 Dec 24.
Vanier MT, Millat G. Niemann-Pick disease type C. Clin Genet. 2003;64:269–81.
Sandu S, Jacüowski-Dohrmann S, Ladner A, Haberhausen M, Bachmann C. Niemann-Pick disease type C1 presenting psychosis in an adolescent male. Eur Child Adolesc Psychiatry. 2009;18:583–5. https://doi.org/10.1007/s00787-009-0010-2 Epub 2009 Mar 7.
Raja M, Azzoni A, Giona F, Regis S, Grossi S, Filocamo M, et al. Movement and mood disorder in two brothers with Gaucher disease. Clin Genet. 2007;72:357–61.
Geraets RD, Koh SY, Hastings ML, Kielian T, Pearce DA, Weimer JM. Moving towards effective therapeutic strategies for neuronal ceroid lipofuscinosis. Orphanet J Rare Dis. 2016;11:40–52.
Cotman SL, Karaa A, Staropoli JF, Sims KB. Neuronal ceroid lipofuscinosis: impact of recent genetic advances and expansion of the clinicopathologic spectrum. Curr Neurol Neurosci Rep. 2012;13:366. https://doi.org/10.1007/s11910-013-366-z.
Gairing S, Wiest R, Metzler S, Theodoridou A, Hoff P. Fabry’s disease and psychosis: causality or coincidence? Psychopathol. 2011;44:201–4. https://doi.org/10.1159/000322794 Epub 2011 Mar 17.
Tsuboi K, Yamamoto H. Efficacy and safety of enzyme-replacement therapy with agalsidase alfa in 36 treatment-naïve Fabry disease patients. BMC Pharmacol Toxicol. 2017;18:43. https://doi.org/10.1186/s40360-017-0152-7.
McCafferty EH, Scott LJ. Migalastat: a review in Fabry disease. Drugs. 2019;79:543–54. https://doi.org/10.1007/s40265-019-01090-4.
Tomatsu S, Fujii T, Fuüshi M, Oguma T, Shimada T, Maeda M, et al. Newborn screening and diagnosis of mucopolysaccharidoses. Mol Genet Metab. 2013;110:42–53.
Opoka-Winiarska V, Jurecka A, Emeryk A, Tylki-Szymańska A. Osteoimmunology in mucopolysaccharidosis type I, II, VI, and VII: immunologic regulation of the osteoarticular system in the course of metabolic inflammation. Osteoarthr Cartil. 2013;21:1813–23. https://doi.org/10.1016/j.joca.2013.08.001 Epub 2013 Aug 13.
Zelei T, Csetneki K, Vokó Z, Siffel C. Epidemiology of Sanfilippo syndrome: results of a systematic literature review. Orphanet J Rare Dis. 2018;13:53. https://doi.org/10.1186/s13023-018-0796-4.
Muenzer J. Early initiation of enzyme replacement therapy for the mucopolysaccharidoses. Mol Genet Metab. 2014;111:63–72.
Andrade F, Aldámiz-Echevarría L, Llarena M, Couce ML. Sanfilippo syndrome: overall review. Pediatr Int. 2015;57:331–8. https://doi.org/10.1111/ped.12636.
Moser HW, Mahmood A, Raymond GV. X-linked adrenoleukodystrophy. Nature Clin Prac Neurol. 2007;3:140–51.
Kassmann CM. Myelin peroxisomes – essential organelles for the maintenance of white matter in the nervous system. Biochimie. 2014;98:111–8. https://doi.org/10.1016/j.biochi.2013.09.020 Epub 2013 Oct 9. Review.
Kemp S, Huffnagel IC, Linthorst G, Wanders RJ, Engelen M. Adrenoleukodystrophy – neuroendocrine pathogenesis and redefinition of natural history. Nat Rev Endocrinol. 2016;12:606–15.
Ferrer I, Aubourg P, Pujol A. General aspects and neuropathology of X-linked adrenoleukodystrophy. Brain Pathol. 2010;20:817–30. https://doi.org/10.1111/j.1750-3639.2010.00390.x Review.
Berger J, Pujol A, Aubourg P, Forss-Petter S. Current and future pharmacological treatment strategies in X-linked adrenoleukodystrophy. Brain Pathol. 2010;20:845–56. https://doi.org/10.1111/j.1750-3639.2010.00393.x.
Haren KV, Engelen M. Decision making adrenoleukodystrophy: when is a good outcome really a good outcome? JAMA Neurol. 2017;74:641–2. https://doi.org/10.1001/jamaneurol.2017.0095.
Takemoto Y, Suzuki Y, Tamakoshi A, Onodera O, Tsuji S, Hashimoto T, et al. Epidemiology of X-linked adrenoleukodystrophy in Japan. J Hum Genet. 2002;47:590–3. https://doi.org/10.1007/s100380200090.
Huffnagel IC, Laheji FK, Aziz-Bose R, Tritos NA, Marino R, Linthorst GE, et al. The natural history of adrenal insufficiency in X-linked adrenoleukodystrophy: an international collaboration. J Clin Endocrinol Metab. 2019;104:118–26. https://doi.org/10.1210/jc.2018-81307.
Patterson MC. Inborn errors of metabolism for neurology residents. Semin Pediatr Neurol. 2011;18:95–7. https://doi.org/10.1016/j.spen.2011.06.016.
Tran C, Patel J, Stacy H, Mamak EG, Faghfoury H, Raiman J, et al. Long-term outcome of patients with X-linked adrenoleukodystrophy: a retrospective cohort study. Eur J Paediatr Neurol. 2017;21:600–9.
Kitchin W, Cohen-Cole SA, Mickel SF. Adrenoleukodystrophy: frequency of presentation as a psychiatric disorder. Biol Psychiatry. 1987;22:1375–87.
Garside S, Rosebush PI, Levinson AJ, Mazurek MF. Late-onset adrenoleukodystrophy associated with long-standing psychiatric symptoms. J Clin Psychiatry. 1999;60:460–8.
Groeschel S, Kühl JS, Bley AE, Kehrer C, Weschke B, Döring M, et al. Long-term outcome of allogeneic hematopoietic stem cell transplantation in patients with juvenile metachromatic leukodystrophy compared with nontransplanted control patients. JAMA Neurol. 2016;73:1133–40.
Kühl J-S, Kupper J, Baqué H, Ebell W, Gärtner J, Korenke C, et al. Potential risks to stable long-term outcome of allogenic hematopoietic stem cell transplantation for children with cerebral x-linked adrenoleukodystrophy. JAMA Netw Open. 2018;1:e180769. https://doi.org/10.1001/jamanetworkopen.2018.0769.
Eichler F, Duncan D, Musolino PL, Orchard PJ, De Olieveira S, Thrasher AJ, et al. Hematopoietic stem-cell gene therapy for cerebral adrenoleukodystrophy. N Engl J Med. 2017;377:1630–8.
Bessey A, Chilcott JB, Leaviss J, Sutton A. Economic impact of screening for X-linked adrenoleukodystrophy within a newborn blood spot screening programme. Orphanet J Rare Dis. 2018;13:179. https://doi.org/10.1186/s13021-018-0921-4.
Kaufman KR, Zuber N, Rueda-Lara MA, Tobia A. MELAS with recurrent complex partial seizures, nonconvulsive status epilepticus, psychosis, and behavioral disturbances: case analysis with literature review. Epilepsy Behav. 2010;18:494–7. https://doi.org/10.1016/j.yebeh.2010.05.020 Epub 2010 Jun 26.
Sproule DM, Kaufmann P. Mitochondrial encephalopathy, lactic acidosis, and stroke like episodes: basic concepts, clinical phenotype, and therapeutic management of MELAS syndrome. Ann N Y Acad Sci. 2008;1142:133–58. https://doi.org/10.1196/annals.1444.011.
Ko A, Lee S-J, Lee Y-M. Focal cerebellar infarction as an initial sign of mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes. J Inherit Metab Dis. 2019;42:575–6.
Anglin RE, Garside SL, Tarnopolsky MA, Mazurek MF, Rosebush PI. The psychiatric manifestations of mitochondrial disorders: a case and review of the literature. J Clin Psychiatry 2012; 73:506–512. https://doi.org/10.4088/JCP.11r07237.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Statement
This manuscript is based on literature review.
Ethical Approval
Patient charts were not reviewed. This article does not contain any data from a new study with human participants performed by any of the authors. Institutional Review Board clearance was not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Turkel, S.B., Wong, D. & Randolph, L. Psychiatric Symptoms Associated with Inborn Errors of Metabolism. SN Compr. Clin. Med. 2, 1646–1660 (2020). https://doi.org/10.1007/s42399-020-00403-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00403-z