Abstract
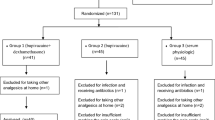
Determine the efficacy of the lesser palatine nerve block (LPNB) in pain management during and after peritonsillar abscess (PTA) drainage. A single-center, prospective, controlled study conducted in a tertiary referral center between April 2015 and September 2017. Twenty-four patients with a PTA were selected initially for our study. Two patients were excluded due to parapharyngeal and mediastinal extension. The remaining 22 patients were divided into two groups: the first group comprised 10 patients who underwent ipsilateral LPNB before PTA drainage. The second (control) group consisted of 12 patients in which only 10% lidocaine spray was used before PTA drainage. Intraoperative and postoperative pain was evaluated using a questionnaire with a 10-point numeric scale. The mean pain score in the study group was 1.9 (50% of the patients reported no pain) and it was 8.4 in the control group. The mean postoperative pain score after surgical drainage was 0.8 (60% of patients reported no pain) in the study group and 3.3 in the control group. No complications of the procedure were reported. The LPNB is a simple, safe, and efficacious anesthetic technique to reduce pain in patients undergoing surgical drainage of a PTA.




Similar content being viewed by others
References
Klug TE, Rusan M, Fuursted K, Ovesen T. Peritonsillar abscess: complication of acute tonsillitis or Webers gland infection? Otolaryngol Head Neck Surg. 2016;155:199–207.
Galioto NJ. Peritonsillar abscess. Am Fam Physician. 2017;95(8):501–6.
Risberg S, Engfeldt P, Hugosson S. Incidence of peritonsillar abscess and relationship to age and gender: retrospective study. Scand J Infect Dis. 2008;40(10):792–6.
Suskind DL, Park J, Piccirillo JF, Lusk RP, Muntz HR. Conscious sedation: a new approach for peritonsillar abscess drainage in the pediatric population. Arch Otolaryngol Head Neck Surg. 1999;125(11):1197–200.
Roberts JR. Otolaryngologic procedures (Clinical procedures in emergency medicine). 5th ed. Philadelphia: Saunders Elsevier; 2010. p. 1197–215.
Riviello RJ, Brown NA. Otolaryngologic procedures. Roberts and Hedges (Clinical Procedures in Emergency Medicine and Acute Care). 7th ed. Philadelphia, PA: Elsevier; 2019. p. 1338–1383.
Ueno T, Tsuchiya H, Mizogami M, Takakura K. Local anesthetic failure associated with inflammation: verification of the acidosis mechanism and the hypothetic participation of inflammatory peroxynitrite. J Inflamm Res. 2008;1:41–8.
Seikaly HR, Harris JR, Villa-Roel C, Brick C, Rowe BH, Chau JK. Corticosteroids in peritonsillar abscess treatment: a blinded placebo-controlled clinical trial. Laryngoscope. 2014;124(1):97–103.
Peltier J, Quinn F. Regional anesthesia in head and neck surgery. Dr. Quinn’s Grand Rounds Presentation, UTMB, Dept. of Otolaryngology. 2006;1–8.
Horlocker T, Kopp S, Wedel D. Peripheral nerve blocks. Miller’s anesthesia. 8th ed. Philadelphia, PA: Saunders Elsevier; 2015. p. 1721–1751.
Salam GA. Regional anesthesia for office procedures: part I. Head and neck surgeries. Am Fam Physician. 2004;69(3):585–90.
Farooq M. Local infiltration anesthesia in drainage of quinsy. Int J Pathol. 2015;13(4):142–7.
Chung JH, Lee YC, Shin SY, Eun YG. Risk factors for recurrence of peritonsillar abscess. J Laryngol Otol. 2014;128(12):1084–8.
Acknowledgments
The authors would like to thank to Carlos Ruah, MD PhD, for his help in writing this manuscript and to Ms. Daniela Patrício for her help in improving the article images.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery
Rights and permissions
About this article
Cite this article
Gilberto, N., Almeida, G., Correia, F. et al. Lesser Palatine Nerve Block in Peritonsillar Abscess Drainage: a Prospective and Controlled Study. SN Compr. Clin. Med. 1, 831–836 (2019). https://doi.org/10.1007/s42399-019-00128-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-019-00128-8