Abstract
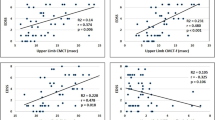
Conventional analysis of motor-evoked potential (MEP) is performed in time domain using amplitude and latency, which encapsulates information relevant to the cortical excitability of the brain. The study investigated the importance of time-frequency analysis by comparing MEPs in time-frequency domains (TFD) of healthy versus stroke survivors. Six healthy subjects and ten patients with stroke were enrolled. Single-pulse transcranial magnetic stimulation (TMS) at resting motor threshold (RMT) was given at extensor digitorum communis muscle cortical representation to obtain MEP. MEPs were obtained at resting motor threshold (100% RMT subjects and patients), supra-threshold range (100–170% RMT), and different voluntary contractions (100% RMT) to subjects. Fast Fourier transform and continuous wavelet transform (CWT) were used for analysis. Frequency spectrum showed 98% and 66% of signal power in 0–100 Hz for subjects and patients, respectively. Top 10, top 25, and top 50 percentile power of CWT were calculated for each MEP. Frequency spectrum of top 10 and top 25 percentile power of subjects were different (p < 0.05) and dispersed to 0–500 Hz for patients; both groups having a 40-Hz peak. Total power of MEP was found to be low (p < 0.05) in patients as compared to subjects and top 10, top 25, and top 50 percentile power showed decrease. Clinical scores—MAS and FM—were observed to be correlated to frequency and time-frequency features (p < 0.05). Frequency spectrum belonging top 10 percentile power of different level voluntary contractions showed statistical significance (p < 0.05). However, no significant differences were observed for MEPs at different supra-threshold intensities. Results suggest time-frequency analysis might provide objective ways to quantify TMS measures for stroke patients.





Similar content being viewed by others
References
Lefaucheur J-P, Andre-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125:2150–206.
Sliwinska MW, Vitello S, Devlin JT. Transcranial magnetic stimulation for investigating causal brain-behavioral relationships and their time course. JoVE (Journal of Visualized Experiments). 2014 Jul 18(89):e51735.
Cantarero G, Celnik P. 11 applications of TMS to study brain connectivity. Brain Stimul Methodol. 2015; https://books.google.co.in/books?hl=en&lr=&id=lJc3BwAAQBAJ&oi=fnd&pg=PA191&dq=Applications+of+TMS+to+Study+Brain+Connectivity.+Brain+Stimulation:+Methodologies+and+Interventions&ots=Y50YdyLPcR&sig=HmJikFd_vZ3wtZXpOWDKEBRbBVQ. Accessed 2 Oct 2016.
Rossi S, Hallett M, Rossini PM, Pascual-Leone A, Avanzini G, Bestmann S, et al. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120:2008–39. https://doi.org/10.1016/j.clinph.2009.08.016.
Chen R, Cros D, Curra A, Di Lazzaro V, Lefaucheur JP, Magistris MR, et al. The clinical diagnostic utility of transcranial magnetic stimulation: report of an IFCN committee. Clin Neurophysiol. 2008;119:504–32.
Rossini PM, Barker AT, Berardelli A, Caramia MD, Caruso G, Cracco RQ, et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol. 1994;91:79–92. https://doi.org/10.1016/0013-4694(94)90029-9.
Rossini PM, Burke D, Chen R, Cohen LG, Daskalakis Z, Di Iorio R, et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: basic principles and procedures for routine clinical and research application: an updated report from an I.F.C.N. Committee. Clin Neurophysiol. 2015;126:1071–107. https://doi.org/10.1016/j.clinph.2015.02.001.
Escudero JV, Sancho J, Bautista D, Escudero M, López-Trigo J. Prognostic value of motor evoked potential obtained by transcranial magnetic brain stimulation in motor function recovery in patients with acute ischemic stroke. Stroke. 1998;29:1854–9 http://www.ncbi.nlm.nih.gov/pubmed/9731608. Accessed 9 May 2018.
Bestmann S, Krakauer JW. The uses and interpretations of the motor-evoked potential for understanding behaviour. Exp Brain Res. 2015;233:679–89. https://doi.org/10.1007/s00221-014-4183-7.
Rothwell JC. Techniques and mechanisms of action of transcranial stimulation of the human motor cortex. J Neurosci Methods. 1997;74:113–22.
Hess CW, Mills KR, Murray NM. Responses in small hand muscles from magnetic stimulation of the human brain. J Physiol. 1987;388:397–419 http://www.ncbi.nlm.nih.gov/pubmed/3079553. Accessed 2 Oct 2016.
Zhang H, Oweis Y, Mozaffari-Naeini H, Venkatesha S, Thakor NV, Natarajan A. Continuous quantitative motor evoked potentials for spinal cord injury detection. 2nd Int IEEE EMBS Conf Neural Eng. 2005;2005:430–3.
Héroux ME, Taylor JL, Gandevia SC. Correction: the use and abuse of transcranial magnetic stimulation to modulate corticospinal excitability in humans. PLoS One. 2016;11:e0147890. https://doi.org/10.1371/journal.pone.0147890.
Grunhaus L, Polak D, Amiaz R, Dannon PN. Motor-evoked potential amplitudes elicited by transcranial magnetic stimulation do not differentiate between patients and normal controls. Int J Neuropsychopharmacol. 2003;6:371–8.
Butler AJ, Kahn S, Wolf SL, Weiss P, Barker A, Beric A, et al. Finger extensor variability in TMS parameters among chronic stroke patients. J Neuroeng Rehabil. 2005;2:10. https://doi.org/10.1186/1743-0003-2-10.
Hu Y, Luk KD, Lu WW, Holmes A, Leong JC. Prevention of spinal cord injury with time-frequency analysis of evoked potentials: an experimental study. J Neurol Neurosurg Psychiatry. 2001;71:732–40 http://www.ncbi.nlm.nih.gov/pubmed/11723192. Accessed 16 Nov 2016.
Braun JC, Hanley DF, Thakor NV. Detection of neurological injury using time-frequency analysis of the somatosensory evoked potential. Electroencephalogr Clin Neurophysiol Potentials Sect. 1996;100:310–8. https://doi.org/10.1016/0168-5597(96)95115-1.
Wang Y, Zhang Z, Li X, Cui H, Xie X, Luk KD-K, et al. Usefulness of time–frequency patterns of somatosensory evoked potentials in identification of the location of spinal cord injury. J Clin Neurophysiol. 2015;32:341–5. https://doi.org/10.1097/WNP.0000000000000167.
Zhang Z-G, Yang J-L, Chan S-C, Luk KD-K, Hu Y. Time-frequency component analysis of somatosensory evoked potentials in rats. Biomed Eng Online. 2009;8:4. https://doi.org/10.1186/1475-925X-8-4.
Wang Y, Li G, Luk KDK, Hu Y. Component analysis of somatosensory evoked potentials for identifying spinal cord injury location. Sci Rep. 2017;7:2351. https://doi.org/10.1038/s41598-017-02555-w.
Wang Y, Cui H, Pu J, Luk KDK, Hu Y. Time-frequency patterns of somatosensory evoked potentials in predicting the location of spinal cord injury. Neurosci Lett. 2015;603:37–41. https://doi.org/10.1016/J.NEULET.2015.07.002.
Hu Y, Luk KDK, Lu WW, Leong JCY. Application of time-frequency analysis to somatosensory evoked potential for intraoperative spinal cord monitoring. J Neurol Neurosurg Psychiatry. 2003;74:82–7. https://doi.org/10.1136/JNNP.74.1.82.
Wolf SL, Butler AJ, Campana GI, Parris TA, Struys DM, Weinstein SR, et al. Intra-subject reliability of parameters contributing to maps generated by transcranial magnetic stimulation in able-bodied adults. Clin Neurophysiol. 2004;115:1740–7. https://doi.org/10.1016/J.CLINPH.2004.02.027.
Lazar RB. Principles of neurologic rehabilitation: McGraw-Hill, Health Professions Division; 1998. https://lib.ugent.be/en/catalog/rug01:000417398. Accessed 10 Jul 2018
Grosse P, Cassidy MJ, Brown P. EEG-EMG, MEG-EMG and EMG-EMG frequency analysis: physiological principles and clinical applications. Clin Neurophysiol. 2002;113:1523–31.
Homan RW, Herman J, Purdy P. Cerebral location of international 10–20 system electrode placement. Electroencephalogr Clin Neurophysiol. 1987;66:376–82.
Werhahn KJ, Fong JKY, Meyer B-U, Priori A, Rothwell JC, Day BL, et al. The effect of magnetic coil orientation on the latency of surface EMG and single motor unit responses in the first dorsal interosseous muscle. Electroencephalogr Clin Neurophysiol Potentials Sect. 1994;93:138–46.
Awiszus F. Chapter 2 TMS and threshold hunting. Suppl Clin Neurophysiol. 2003;56:13–23. https://doi.org/10.1016/S1567-424X(09)70205-3.
Kobayashi M, Pascual-Leone A. Transcranial magnetic stimulation in neurology. Lancet Neurol. 2003;2:145–56. https://doi.org/10.1016/S1474-4422(03)00321-1.
Day BL, Dressler D, Maertens de Noordhout A, Marsden CD, Nakashima K, Rothwell JC, et al. Electric and magnetic stimulation of human motor cortex: surface EMG and single motor unit responses. J Physiol. 1989;412:449–73. https://doi.org/10.1113/jphysiol.1989.sp017626.
Angelova S, Ribagin S, Raikova R, Veneva I. Power frequency spectrum analysis of surface EMG signals of upper limb muscles during elbow flexion—a comparison between healthy subjects and stroke survivors. J Electromyogr Kinesiol. 2018;38:7–16. https://doi.org/10.1016/J.JELEKIN.2017.10.013.
Henneman E. The size-principle: a deterministic output emerges from a set of probabilistic connections. Journal of experimental biology. 1985 Mar 1;115(1):105–12.
Brown P. Muscle sounds in Parkinson’s disease. Lancet. 1997;349:533–5. https://doi.org/10.1016/S0140-6736(97)80086-4.
Lodha N, Chen Y-T, McGuirk T, Fox EJ, Kautz SA, Christou EA, et al. EMG synchrony to assess impaired corticomotor control of locomotion after stroke. J Electromyogr Kinesiol. 2017;37:35–40. https://doi.org/10.1016/J.JELEKIN.2017.08.007.
Fang Y, Daly JJ, Sun J, Hvorat K, Fredrickson E, Pundik S, et al. Functional corticomuscular connection during reaching is weakened following stroke. Clin Neurophysiol. 2009;120:994–1002. https://doi.org/10.1016/j.clinph.2009.02.173.
Rothwell J, Thompson P, Day B, Boyd S, Marsden C. Stimulation of the human motor cortex through the scalp. Exp Physiol. 1991;76:159–200.
Acknowledgments
The authors would like to express sincere gratitude to healthy subjects and patients who agreed to participate in the study. Also, they thank Mr. Vikas Kumar and Ms. Komal at TMS laboratory for their support during data acquisition and Mr. Dixit Sharma for the help in data analysis.
Funding
This work was supported by Science and Engineering Research Board (SERB), DST, Government of India (YSS/2015/000697). Neha Singh was supported with research fellowship funds from the Ministry of Human Resource and Development (MHRD), Government of India.
Author information
Authors and Affiliations
Contributions
Conceptualization: NS, AM; data curation: NS,MS; formal analysis: NS, AM; funding acquisition: AM; methodology: NS, AM; resources: NK, SA, PS; supervision: AM; writing the original draft: NS, AM; writing the review and editing: NS, AM, KKD, NK, PS.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board (IRB) at the All India Institute of Medical Science, New Delhi (IEC/NP-99/13.03.2015).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Electronic Supplementary Material
ESM 1
(DOCX 69 kb)
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Singh, N., Saini, M., Kumar, N. et al. Time-Frequency Analysis of Motor-Evoked Potential in Patients with Stroke vs Healthy Subjects: a Transcranial Magnetic Stimulation Study. SN Compr. Clin. Med. 1, 764–780 (2019). https://doi.org/10.1007/s42399-019-00113-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-019-00113-1