Abstract
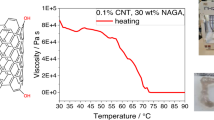
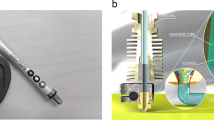
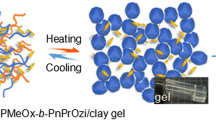
Nanoclay-enabled self-supporting printing has been emerging as a promising filament-based extrusion fabrication approach for different biomedical and engineering applications including tissue engineering. With the addition of nanoclay powders, liquid build materials may exhibit solid-like behavior upon extrusion and can be directly printed in air into complex three-dimensional structures. The objective of this study is to investigate the effect of nanoclay on the extrudability of N-isopropylacrylamide (NIPAAm) and the effect of standoff distance on the print quality during nanoclay-enabled direct printing. It is found that the addition of nanoclay can significantly improve the NIPAAm extrudability and effectively eliminate die swelling in material extrusion. In addition, with the increase of standoff distance, deposited filaments change from over-deposited to well-defined to stretched to broken, the filament width decreases, and the print fidelity deteriorates. A mathematical model is further proposed to determine the optimal standoff distance to achieve better print fidelity during nanoclay-enabled direct printing. Based on the extrudability and standoff distance knowledge from this study, NIPAAm–Laponite nanoclay and NIPAAm–Laponite nanoclay–graphene oxide nanocomposite hydrogel precursors are successfully printed into a three-layered one-dimensional responsive pattern, demonstrating the good extrudability and print quality during nanoclay-enabled printing under optimal printing conditions.







Similar content being viewed by others
References
Mironov V, Visconti RP, Kasyanov V, Forgacs G, Drake CJ, Markwald RR (2009) Organ printing: tissue spheroids as building blocks. Biomaterials 30(12):2164–2174
Ringeisen BR, Pirlo RK, Wu PK, Boland T, Huang Y, Sun W, Chrisey DB (2013) Cell and organ printing turns 15: diverse research to commercial transitions. MRS Bull 38(10):834–843
Murphy SV, Atala A (2014) 3D bioprinting of tissues and organs. Nat Biotechnol 32(8):773–785
Huang Y, Leu MC, Mazumder J, Donmez A (2015) Additive manufacturing: current state, future potential, gaps and needs, and recommendations. ASME J Manuf Sci Eng 137(1):014001-1-10
Roth EA, Xu T, Das M, Gregory C, Hickman JJ, Boland T (2004) Inkjet printing for high-throughput cell patterning. Biomaterials 25(17):3707–3715
Xu C, Chai W, Huang Y, Markwald RR (2012) Scaffold-free inkjet printing of three-dimensional zigzag cellular tubes. Biotechnol Bioeng 109(12):3152–3160
Christensen K, Xu C, Chai W, Zhang Z, Fu J, Huang Y (2015) Freeform inkjet printing of cellular structures with bifurcations. Biotechnol Bioeng 112(5):1047–1055
Barron JA, Ringeisen BR, Kim H, Spargo BJ, Chrisey DB (2004) Application of laser printing to mammalian cells. Thin Solid Films 453:383–387
Xiong R, Zhang Z, Chai W, Huang Y, Chrisey DB (2015) Freeform drop-on-demand laser printing of 3D alginate and cellular constructs. Biofabrication 7(4):045011-1-13
Khalil S, Sun W (2007) Biopolymer deposition for freeform fabrication of hydrogel tissue constructs. Mater Sci Eng C 27(3):469–478
Jin Y, Compaan AM, Bhattacharjee T, Huang Y (2016) Granular gel support-enabled extrusion of three-dimensional alginate and cellular structures. Biofabrication 8(2):025016-1-12
Jin Y, Liu C, Chai W, Compaan AM, Huang Y (2017) Self-supporting nanoclay as internal scaffold material for direct printing of soft hydrogel composite structures in air. ACS Appl Mater Interfaces 9(20):17456–17465
Jin Y, Compaan AM, Chai W, Huang Y (2017) Functional nanoclay suspension for printing-then-solidification of liquid materials. ACS Appl Mater Interfaces 9(23):20057–20066
Landers R, Hübner U, Schmelzeisen R, Mülhaupt R (2002) Rapid prototyping of scaffolds derived from thermoreversible hydrogels and tailored for applications in tissue engineering. Biomaterials 23(23):4437–4447
Fedorovich NE, De Wijn JR, Verbout AJ, Alblas J, Dhert WJ (2008) Three-dimensional fiber deposition of cell-laden, viable, patterned constructs for bone tissue printing. Tissue Eng Part A 14(1):127–133
Hockaday LA, Kang KH, Colangelo NW, Cheung PYC, Duan B, Malone E, Wu J, Girardi LN, Bonassar LJ, Lipson H, Chu CC, Butcher JT (2012) Rapid 3D printing of anatomically accurate and mechanically heterogeneous aortic valve hydrogel scaffolds. Biofabrication 4(3):035005
Bertassoni LE, Cardoso JC, Manoharan V, Cristino AL, Bhise NS, Araujo WA, Zorlutuna P, Vrana NE, Ghaemmaghami AM, Dokmeci MR, Khademhosseini A (2014) Direct-write bioprinting of cell-laden methacrylated gelatin hydrogels. Biofabrication 6(2):024105
Ozbolat IT, Hospodiuk M (2016) Current advances and future perspectives in extrusion-based bioprinting. Biomaterials 76:321–343
Chung JH, Naficy S, Yue Z, Kapsa R, Quigley A, Moulton SE, Wallace GG (2013) Bio-ink properties and printability for extrusion printing living cells. Biomater Sci 1(7):763–773
Kang KH, Hockaday LA, Butcher JT (2013) Quantitative optimization of solid freeform deposition of aqueous hydrogels. Biofabrication 5(3):035001
Schmaljohann D (2006) Thermo-and pH-responsive polymers in drug delivery. Adv Drug Deliv Rev 58(15):1655–1670
Wei H, Zhang X, Cheng C, Cheng SX, Zhuo RX (2007) Self-assembled, thermosensitive micelles of a star block copolymer based on PMMA and PNIPAAm for controlled drug delivery. Biomaterials 28(1):99–107
Gaharwar AK, Peppas NA, Khademhosseini A (2014) Nanocomposite hydrogels for biomedical applications. Biotechnol Bioeng 111(3):441–453
Xavier JR, Thakur T, Desai P, Jaiswal MK, Sears N, Cosgriff-Hernandez E, Gaharwar AK (2015) Bioactive nanoengineered hydrogels for bone tissue engineering: a growth-factor-free approach. ACS Nano 9(3):3109–3118
Jin Y, Shen Y, Yin J, Qian J, Huang Y (2018) Nanoclay-based self-supporting responsive nanocomposite hydrogels for printing applications. ACS Appl Mater Interfaces 10(12):10461–10470
Jin Y, Chai W, Huang Y (2017) Printability study of hydrogel solution extrusion in nanoclay yield-stress bath during printing-then-gelation biofabrication. Mater Sci Eng C 80:313–325
Zhang Z, Xiong R, Mei R, Huang Y, Chrisey DB (2015) Time-resolved imaging study of jetting dynamics during laser printing of viscoelastic alginate solutions. Langmuir 31(23):6447–6456
Piau JM, El Kissi N, Tremblay B (1990) Influence of upstream instabilities and wall slip on melt fracture and sharkskin phenomena during silicones extrusion through orifice dies. J Non Newton Fluid Mech 34(2):145–180
Liu L, Wang W, Ju XJ, Xie R, Chu LY (2010) Smart thermo-triggered squirting capsules for nanoparticle delivery. Soft Matter 6(16):3759–3763
Yan B, Boyer JC, Habault D, Branda NR, Zhao Y (2012) Near infrared light triggered release of biomacromolecules from hydrogels loaded with upconversion nanoparticles. J Am Chem Soc 134(40):16558–16561
Feinberg AW, Feigel A, Shevkoplyas SS, Sheehy S, Whitesides GM, Parker KK (2007) Muscular thin films for building actuators and powering devices. Science 317(5843):1366–1370
Peng X, Li Y, Zhang Q, Shang C, Bai QW, Wang H (2016) Tough hydrogels with programmable and complex shape deformations by ion dip-dyeing and transfer printing. Adv Funct Mater 26(25):4491–4500
Acknowledgements
This study was partially supported by the U.S. National Science Foundation (NSF CMMI-1634755).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jin, Y., Zhao, D. & Huang, Y. Study of extrudability and standoff distance effect during nanoclay-enabled direct printing. Bio-des. Manuf. 1, 123–134 (2018). https://doi.org/10.1007/s42242-018-0009-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42242-018-0009-y