Abstract
The use of dental implants in the partial and complete edentulism has become the primary treatment regimen in the modern dentistry. Erbium chromium-doped yattrium-scandium-gallium-garnet (Er,Cr:YSGG) laser is most often used in dentistry in implant surgery and management of peri-implantitis. The aim of the present study was to assess the biocompatibility of Er,Cr:YSGG laser-treated titanium alloy (Ti-6Al-4V) and its surface characteristics to understand the impact of the laser on the titanium alloy surfaces.
Materials and methods
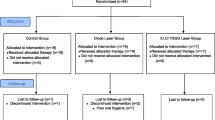
A total of 20 discs of titanium alloy (Ti-6Al-4V) were used. Ten discs were irradiated with Er,Cr:YSGG laser which was operating in a normal room atmosphere and temperature at power 2 W. Biocompatibility was investigated in vitro via MTT assay. Surface analysis of laser-treated and laser-untreated discs was examined with a scanning electron microscope.
Result
Laser-treated group showed superior cell viability compared to untreated group. No undesirable changes were observed by SEM.
Conclusion
We can conclude that Er,Cr:YSGG laser safely could improve the biocompatibility of dental implant.




Similar content being viewed by others
References
Seth S, Kalra P (2013) Effect of dental implant parameters on stress distribution at bone-implant interfaces. Inter J Sci Res 2:121–124
Abdel-Hady Gepreel M, Niinomi M (2013) Biocompatibility of Ti-alloys for long-term implantation. J Mech Behav Biomed Mate 20:407–415
Yamazoe J, Nakagawa M, Matono Y, Takeuchi A, Ishikawa K (2007) The development of Ti alloys for dental implant with high corrosion resistance and mechanical strength. Dent Mater J 26:260–267
Piotrowski B, Baptista AA, Patoor E, Bravetti P, Eberhardt A, Laheurte P (2014) Interaction of bone-dental implant with new ultra low modulus alloy using a numerical approach. Mater Sci Engin C 38:151–160
Koike M, Hummel SK, Ball JD, Okabe T (2012) Fabrication of titanium removable dental prosthesis frameworks with a 2-step investment coating method. J Prosthet Dent 107:393–399
Baltriukiene D, Sabaliuskas V, Balciusas E, Melninkaitis A, Liufkelskene E, Bukelskiene V (2014) The effect of laser-treated titanium surface on human gingival fibroblast behavior. J Biomed Mater Res A 102(3):713–720
Kearns VR, Williams RL, Mirvakily F, Doberty PJ, Martin N (2013) Guided gingival fibroblast attachment to titanium surface: an in vitro study. J Clin Periodontol 40(1):99–108
O’Brien WJ (2009) Dental materials and their selection, 4th edn. Quintessence Publishing, Chicago, p 23
Frankova J, Pivodova V, Ruzicka F, Tomankova K, Vrlkova J (2013) Comparing biocompatibility of gingival fibroblast and bacterial strains on a different modified titanium discs. J Biomed Mater Res A 101(10):2915–2924
Arisan V, Karabuda CZ, Ozdemir T (2010) Implant surgery using bone- and mucosa-supported stereolithographic guides in totally edentulous jaws: surgical and post-operative outcomes of computer-aided vs.standard techniques. Clin Oral Implants Res 21(9):980–988
Nickenig H-J, Wichmann M, Schlegel KA, Nkenke E, Eitner S (2010) Radiographic evaluation of marginal bone levels during healing period, adjacent to parallel-screw cylinder implants inserted in the posterior zone of the jaws, placed with flapless surgery. Clin Oral Implants Res 21(12):1386–1393
Pourzarandian A, Watanabe H, Aoki A, Ichinose S, Sasaki KM, Nitta H, Ishikawa I (2004) Histological and TEM examination of early stages of bone healing after Er:YAG laser irradiation. Photomed Laser Surg 22(4):342–350
Yoshino T, Aoki A, Oda S, Takasaki AA, Mizutani K, Sasaki KM, Kinoshita A, Watanabe H, Ishikawa I, Izumi Y (2009) Long-term histologic analysis of bone tissue alteration and healing following Er:YAG laser irradiation compared to electrosurgery. J Periodontol 80(1):82–92
Garg AK (2007) Lasers in dental implantology: innovation improves patient care. Dent Implantol 18:57–61
Featherstone JD (2000) Caries detection and prevention with laser energy. In: Convissar FA (ed) Dent Clin North Am, vol 44. Saunders, Philadelphia, pp 955–966
Gimbel CB (2000) Hard tissue procedures. In: Convissar FA (ed) Dent Clin North Am, vol 44. Saunders, Philadelphia, pp 931–948
Kim S-W, Kwon Y-H, Chung J-H, Shin S-I, Herr Y (2010) The effect of Er:YAG laser irradiation on the surface microstructure and roughness of hydroxyapatite-coated implant. J Periodontal Implant Sci 40:276–282
Matsumoto K, Hossain MM, Kawano H, Kimura Y (2002) Clinical assessment of Er,Cr: YSGG laser application for cavity preparation. J Clin Laser Med Surg 20:17–21
Gomez-Santos L, Arnabat-Dominguez J, Sierra-Rebolledo A, Gay-Escoda C (2010) Thermal increment due to Er,Cr:YSGG and CO2 laser irradiation of different implant surfaces. A pilot study. Med Oral Patol Oral Cir Bucal 15:782–787
Lee JH, Heo SJ, Koak JY, Kim SK, Lee SJ, Lee SH (2008) Cellular responses on anodized titanium discs after laser irradiation. Lasers Surg Med 40:738–742
Park JH, Heo SJ, Koak JY, Kim SK, Han CH, Lee JH (2012) Effects of laser irradiation on machined and anodized titanium disks. Int J Oral Maxillofac Implants 27:265–272
Wataha JC, Lockwood PE, Bouillaguet S, Noda M (2003) In vitro biological response to core and flowable dental restorative materials. Dent Mater 19:25–31
Issa Y, Watts DC, Brunton PA, Waters CM, Duxbury AJ (2004) Resin composite monomers alter MTT and LDH activity of human gingival fibroblasts in vitro. Dent Mater 20:12–20
Bonakdar S et al (2010) Preparation and characterization of polyvinyl alcohol hydrogels crosslinked by biodegradable polyurethane for tissue engineering of cartilage. Mater Sci Eng C 30(4):636–643
Kim HJ, Kim SH, Kim MS, Lee EJ, Oh HG, Oh WM, Park SW, Kim WJ, Lee GJ, Choi NG, Koh JT, Dinh DB, Hardin RR, Johnson K, Sylvia VL, Schmitz JP, Dean DD (2005) Varying Ti-6Al-4V surface roughness induces different early morphologic and molecular responses in MG63osteoblast-like cells. J Biomed Mater Res A 74(3):366–373
Nothdurft FP, Fontana D, Ruppenthal S, May A, Aktas C, Mehraein Y (2014) Differential behavior of fibroblasts and epithelial cells on structured implant abutment materials: a comparison of materials and surface topographies. Clin Implant Dent Relat Res 16:640–648
Atapour M, Pilchak A, Frankel GS, Williams JC, Fathi MH, Shamanian M (2010) Corrosion behavior of Ti-6Al-4V with different thermomechanical treatments and microstructures. Corrosion 66(6):1–9
Martin E (2004) Lasers in dental implantology. Dent Clin North Am 48:999–1015
Kreisler M, Gotz H, Duschner H (2002) Effect of Nd:YAG, Ho: YAG, Er:YAG, CO2, and GaAIAs laser irradiation on surface properties of endosseous dental implants. Int J Oral Maxillofac Implants 17:202–211
Kotsovilis S, Karoussis IK, Trianti M, Fourmousis I (2008) Therapy of peri-implantitis: a systematic review. J Clin Periodontol 35:621–629
Miller RJ (2004) Treatment of the contaminated implant surface using Er,Cr:YSGG laser. Implant Dent 13:165–170
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Abd El daym, D.A., Gheith, M.E., Abbas, N.A. et al. Biocompatibility of erbium chromium-doped yattrium-scandium-gallium-garnet (Er,Cr:YSGG 2780 nm) laser-treated titanium alloy used for dental applications (in vitro study). Laser Dent Sci 2, 119–124 (2018). https://doi.org/10.1007/s41547-018-0029-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-018-0029-0