Abstract
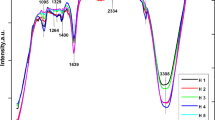
Due to the similarity of synthetic hydroxyapatite (HA) to natural bone tissue, but, because of its low degradation rate, the current study focuses on silicon-substituted HA (Si-HA) synthesis, characterization, and biological evaluations. Si-HA was successfully prepared through sol-gel processing route and characterized using SEM, EDX, XRD, and FTIR. Si-HA particles were found to be non-cytotoxic following exposure to adipose stem cells (ADSCs). In fact, Si-HA particles showed a high level of matrix mineralization following prolonged and continuous exposure to ADSCs. It is suggested that the incorporation of Si in HA structure positively affects cellular behavior, associated with a higher degradation rate, and subsequently greater level of ionic product release from Si-HA particles.
Lay Summary
Hydroxyapatite (HA) has long been applied as bone substitutes but its low degradation rate limits its application. One approach is the incorporation of silicon (Si) within HA structure. This study confirms that Si-substituted HA enhance stem cell proliferation and promote osteogenic differentiation. Hence, Si-HA could be utilized in composites, scaffolds, and coatings for bone-related disorders.




Similar content being viewed by others
References
Olszta MJ, Cheng X, Jee SS, Kumar R, Kim Y-Y, Kaufman MJ, et al. Bone structure and formation: a new perspective. Materials Science and Engineering: R: Reports. 2007;58:77–116.
Sobczak-Kupiec A, Pluta K, Drabczyk A, Włoś M, Tyliszczak B. Synthesis and characterization of ceramic-polymer composites containing bioactive synthetic hydroxyapatite for biomedical applications. Ceram Int. 2018;44:13630–8.
Kolmas J, Krukowski S, Laskus A, Jurkitewicz M. Synthetic hydroxyapatite in pharmaceutical applications. Ceram Int. 2016;42:2472–87.
Tracy BM, Doremus R. Direct electron microscopy studies of the bone—hydroxylapatite interface. J Biomed Mater Res. 1984;18:719–26.
Hellmich C, Ulm F-J. Average hydroxyapatite concentration is uniform in the extracollagenous ultrastructure of mineralized tissues: evidence at the 1–10-μm scale. Biomech Model Mechanobiol. 2003;2:21–36.
Weiner S, Wagner HD. The material bone: structure-mechanical function relations. Annu Rev Mater Sci. 1998;28:271–98.
Poinern GE, Brundavanam RK, Mondinos N, Jiang Z-T. Synthesis and characterisation of nanohydroxyapatite using an ultrasound assisted method. Ultrason Sonochem. 2009;16:469–74.
De Bruijn J, Van Blitterswijk C, Davies J. Initial bone matrix formation at the hydroxyapatite interface in vivo. J Biomed Mater Res. 1995;29:89–99.
Radin S, Ducheyne P. The effect of calcium phosphate ceramic composition and structure on in vitro behavior. II. Precipitation. J Biomed Mater Res. 1993;27:35–45.
Patel N, Best S, Bonfield W, Gibson IR, Hing K, Damien E, et al. A comparative study on the in vivo behavior of hydroxyapatite and silicon substituted hydroxyapatite granules. J Mater Sci Mater Med. 2002;13:1199–206.
Höland W, Vogel W, Naumann K, Gummel J. Interface reactions between machinable bioactive glass-ceramics and bone. J Biomed Mater Res. 1985;19:303–12.
Webster TJ, Ergun C, Doremus RH, Bizios R. Hydroxylapatite with substituted magnesium, zinc, cadmium, and yttrium. II. Mechanisms of osteoblast adhesion. J Biomed Mater Res. 2002;59:312–7.
Hutmacher DW, Schantz JT, Lam CXF, Tan KC, Lim TC. State of the art and future directions of scaffold-based bone engineering from a biomaterials perspective. J Tissue Eng Regen Med. 2007;1:245–60.
Gibson I, Best S, Bonfield W. Chemical characterization of silicon-substituted hydroxyapatite. J Biomed Mater Res. 1999;44:422–8.
Carlisle EM. Silicon: a possible factor in bone calcification. Science. 1970;167:279–80.
El Yacoubi A, Massit A, Fathi M, El Idrissi BC, Yamni K. Characterization of silicon-substituted hydroxyapatite powders synthesized by a wet precipitation method. IOSR J Appl Chem. 2014;7:24–9.
Moheet IA, Luddin N, Ab Rahman I, Kannan TP, Ghani NRNA. Evaluation of mechanical properties and bond strength of nano-hydroxyapatite-silica added glass ionomer cement. Ceram Int. 2018;44:9899–906.
Hijón N, Cabanas MV, Pena J, Vallet-Regí M. Dip coated silicon-substituted hydroxyapatite films. Acta Biomater. 2006;2(2):567–74.
Latifi S, Fathi M, Golozar M. Preparation and characterisation of bioactive hydroxyapatite–silica composite nanopowders via sol–gel method for medical applications. Adv Appl Ceram. 2011;110:8–14.
Kim HW, Kim HE, Salih V, Knowles JC. Hydroxyapatite and titania sol–gel composite coatings on titanium for hard tissue implants; mechanical and in vitro biological performance. J Biomed Mater Res B. 2005;72:1–8.
Andersson J, Areva S, Spliethoff B, Lindén M. Sol–gel synthesis of a multifunctional, hierarchically porous silica/apatite composite. Biomaterials. 2005;26:6827–35.
Malakauskaite-Petruleviciene M, Stankeviciute Z, Niaura G, Prichodko A, Kareiva A. Synthesis and characterization of sol–gel derived calcium hydroxyapatite thin films spin-coated on silicon substrate. Ceram Int. 2015;41:7421–8.
Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H, et al. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13:4279–95.
Alabdulkarim Y, Ghalimah B, Al-Otaibi M, Al-Jallad HF, Mekhael M, Willie B, et al. Recent advances in bone regeneration: the role of adipose tissue-derived stromal vascular fraction and mesenchymal stem cells. J Limb Lengthen Reconstr. 2017;3:4.
Reumann MK, Linnemann C, Aspera-Werz RH, Arnold S, Held M, Seeliger C, et al. Donor site location is critical for proliferation, stem cell capacity, and osteogenic differentiation of adipose mesenchymal stem/stromal cells: implications for bone tissue engineering. Int J Mol Sci. 2018;19.
Beigi MH, Atefi A, Ghanaei HR, Labbaf S, Ejeian F, Nasr-Esfahani MH. Activated platelet-rich plasma improves cartilage regeneration using adipose stem cells encapsulated in a 3D alginate scaffold. J Tissue Eng Regen Med. 2018;12:1327–38.
Milner DJ, Bionaz M, Monaco E, Cameron JA, Wheeler MB. Myogenic potential of mesenchymal stem cells isolated from porcine adipose tissue. Cell Tissue Res. 2018;372:507–22.
Wang Y-H, Wu J-Y, Kong SC, Chiang M-H, Ho M-L, Yeh M-L, et al. Low power laser irradiation and human adipose-derived stem cell treatments promote bone regeneration in critical-sized calvarial defects in rats. PLoS One. 2018;13:e0195337.
Houreh AB, Labbaf S, Ting H-K, Ejeian F, Jones JR, Esfahani M-HN. Influence of calcium and phosphorus release from bioactive glasses on viability and differentiation of dental pulp stem cells. J Mater Sci. 2017;52:8928–41.
Gholami S, Labbaf S, Houreh AB, Ting H-K, Jones JR, Esfahani M-HN. Long term effects of bioactive glass particulates on dental pulp stem cells in vitro. Biomedical Glasses. 2017;3:96–103.
Miron R, Hedbom E, Saulacic N, Zhang Y, Sculean A, Bosshardt D, et al. Osteogenic potential of autogenous bone grafts harvested with four different surgical techniques. J Dent Res. 2011;90:1428–33.
Porter AE, Patel N, Skepper JN, Best SM, Bonfield W. Effect of sintered silicate-substituted hydroxyapatite on remodelling processes at the bone–implant interface. Biomaterials. 2004;25:3303–14.
Bang L, Long B, Othman R. Carbonate hydroxyapatite and silicon-substituted carbonate hydroxyapatite: synthesis, mechanical properties, and solubility evaluations. Sci World J. 2014:2014.
Porter AE, Botelho CM, Lopes MA, Santos JD, Best SM, Bonfield W. Ultrastructural comparison of dissolution and apatite precipitation on hydroxyapatite and silicon-substituted hydroxyapatite in vitro and in vivo. J Biomed Mater Res A. 2004;69:670–9.
Bianco A, Cacciotti I, Lombardi M, Montanaro L. Si-substituted hydroxyapatite nanopowders: synthesis, thermal stability and sinterability. Mater Res Bull. 2009;44:345–54.
Arcos D, Rodrı́guez-Carvajal J, Vallet-Regı́ M. The effect of the silicon incorporation on the hydroxylapatite structure. A neutron diffraction study. Solid State Sci. 2004;6:987–94.
Zheng Y, Dong G, Deng C. Effect of silicon content on the surface morphology of silicon-substituted hydroxyapatite bio-ceramics treated by a hydrothermal vapor method. Ceram Int. 2014;40:14661–7.
Aminian A, Solati-Hashjin M, Samadikuchaksaraei A, Bakhshi F, Gorjipour F, Farzadi A, et al. Synthesis of silicon-substituted hydroxyapatite by a hydrothermal method with two different phosphorous sources. Ceram Int. 2011;37:1219–29.
Dong G, He L, Pang D, Wei L, Deng C. An in situ study of the deposition of a calcium phosphate mineralized layer on a silicon-substituted hydroxyapatite sensor modulated by bovine serum albumin using QCM-D technology. Ceram Int. 2016;42:18648–56.
Bang L, Ishikawa K, Othman R. Effect of silicon and heat-treatment temperature on the morphology and mechanical properties of silicon-substituted hydroxyapatite. Ceram Int. 2011;37:3637–42.
Porter AE. Nanoscale characterization of the interface between bone and hydroxyapatite implants and the effect of silicon on bone apposition. Micron. 2006;37:681–8.
Porter AE, Best SM, Bonfield W. Ultrastructural comparison of hydroxyapatite and silicon-substituted hydroxyapatite for biomedical applications. Biomed Mater Res A. 2004;68:133–41.
Maeno S, Niki Y, Matsumoto H, Morioka H, Yatabe T, Funayama A, et al. The effect of calcium ion concentration on osteoblast viability, proliferation and differentiation in monolayer and 3D culture. Biomaterials. 2005;26:4847–55.
Marie PJ. The calcium-sensing receptor in bone cells: a potential therapeutic target in osteoporosis. Bone. 2010;46:571–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eatemad, M., Labbaf, S., Houreh, A.B. et al. Silicon-Substituted Hydroxyapatite Particles and Response of Adipose Stem Cells In Vitro. Regen. Eng. Transl. Med. 5, 290–296 (2019). https://doi.org/10.1007/s40883-019-00108-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-019-00108-3