Abstract
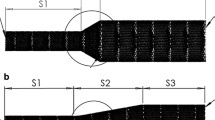
The rupture of intracranial aneurysms might lead to permanent disability or even death. One possible endovascular treatment is the deployment of flow diverters (FDs), which reduces flow into the sac and promotes thrombosis. Computational fluid dynamics simulations were used to assess the flow patterns and dynamics. The concept of energy loss, as a measure of necessary work done to overcome flow resistance, was utilized to correlate with clinical outcome. If a surgical operation is successful, the flow would be diverted to a shorter path and energy loss should be reduced. Conversely, persistent flow in the sac, associated with treatment failure, would display an increased energy loss as blood is then squeezed through the stent pores. Four illustrative clinical cases, involving both bifurcation and sidewall aneurysms, were selected. To reduce the numerical complexity, earlier works in the literature had used a porous medium approximation for the FDs. Here, the FD was simulated explicitly as a virtual (or computer-generated) stent, which would likely provide a more accurate description. Furthermore, quantitative comparisons between the approaches of virtual stenting and a porous medium with typical parameters were conducted by examining the effective flow influx into the aneurysm.











Similar content being viewed by others
References
Vlak, M. H., Algra, A., Brandenburg, R., & Rinkel, G. J. (2011). Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systemic review and meta-analysis. The Lancet Neurology, 10(7), 626–636.
Humphrey, J. D., & Taylor, C. A. (2008). Intracranial and abdominal aortic aneurysms: Similarities, differences, and need for a new class of computational models. Annual Review of Biomedical Engineering, 10, 221–246.
Pierot, L., Cognard, C., Anxionnat, R., & Ricolfi, F. (2012). Endovascular treatment of ruptured intracranial aneurysms: factors affecting midterm quality anatomic results: Analysis in a prospective, multicenter series of patients (CLARITY). American Journal of Neuroradiology, 33(8), 1475–1480.
Gonzalez, N. R., Duckwiler, G., Jahan, R., Murayama, Y., & Viñuela, F. (2006). Challenges in the endovascular treatment of giant intracranial aneurysms. Neurosurgery, 59(5), S3–113.
Jou, L., & Mawad, M. (2011). Timing and size of flow impingement in a giant intracranial aneurysm at the internal carotid artery. Medical & Biological Engineering & Computing, 49(8), 891–899.
Leung, G., Tsang, A., & Lui, W. (2012). Pipeline embolization device for intracranial aneurysm: A systematic review. Clinical Neuroradiology, 22(4), 295–303.
Shapiro, M., Raz, E., Becske, T., & Nelson, P. (2014). Variable porosity of the pipeline embolization device in straight and curved vessels: A guide for optimal deployment strategy. American Journal of Neuroradiology, 35(4), 727–733.
Byrne, J., Beltechi, R., Yarnold, J., Birks, J., & Kamran, M. (2010). Early experience in the treatment of intra-cranial aneurysms by endovascular flow diversion: A multicentre prospective study. PLoS ONE, 5(9), e12492.
Wang, C., Tian, Z., Liu, J., Jing, L., Paliwal, N., Zhang, Y., et al. (2016). Hemodynamic alterations for various stent configurations in idealized wide-neck basilar tip aneurysm. Journal of Medical and Biological Engineering, 36(3), 379–385.
Kallmes, D., Ding, Y., Dai, D., Kadirvel, R., Lewis, D., & Cloft, H. (2009). A second-generation, endoluminal, flow-disrupting device for treatment of saccular aneurysms. American Journal of Neuroradiology, 30(6), 1153–1158.
Brinjikji, W., Murad, M., Lanzino, G., Cloft, H., & Kallmes, D. (2013). Endovascular treatment of intracranial aneurysms with flow diverters a meta-analysis. Stroke, 44(2), 442–447.
Caruso, M. V., Gramigna, V., Serraino, G. F., Renzulli, A., & Fragomeni, G. (2015). Influence of aortic outflow cannula orientation on epiaortic flow pattern during pulsed cardiopulmonary bypass. Journal of Medical and Biological Engineering, 35(4), 455–463.
Cebral, J., Mut, F., Weir, J., & Putman, C. (2011). Quantitative characterization of the hemodynamic environment in ruptured and unruptured brain aneurysms. American Journal of Neuroradiology, 32(1), 145–151.
Lee, C. J., Zhang, Y., Takao, H., Murayama, Y., & Qian, Y. (2013). A fluid–structure interaction study using patient-specific ruptured and unruptured aneurysm: The effect of aneurysm morphology, hypertension and elasticity. Journal of Biomechanics, 46(14), 2402–2410.
Takao, H., Murayama, Y., Otsuka, S., Qian, Y., Mohamed, A., Masuda, S., et al. (2012). Hemodynamic differences between unruptured and ruptured intracranial aneurysms during observation. Stroke, 43(5), 1436–1439.
Li, G., Hu, R., & Gao, F. (2015). Numerical simulation of coronary artery stenosis before and after stenting. Journal of Medical and Biological Engineering, 35(4), 528–534.
Cebral, J., Mut, F., Raschi, M., Scrivano, E., Ceratto, R., Lylyk, P., et al. (2011). Aneurysm rupture following treatment with flow-diverting stents: Computational hemodynamics analysis of treatment. American Journal of Neuroradiology, 32(1), 27–33.
Goubergrits, L., Schaller, J., Kertzscher, U., Woelken, T., Ringelstein, M., & Spuler, A. (2014). Hemodynamic impact of cerebral aneurysm endovascular treatment devices: Coils and flow diverters. Expert Review of Medical Devices, 11(4), 361–373.
Kim, Y. H., Xu, X., & Lee, J. S. (2010). The effect of stent porosity and strut shape on saccular aneurysm and its numerical analysis with lattice Boltzmann method. Annals of Biomedical Engineering, 38(7), 2274–2292.
Kulcsár, Z., Augsburger, L., Reymond, P., Pereira, V. M., Hirsch, S., Mallik, A. S., et al. (2012). Flow diversion treatment: Intra-aneurismal blood flow velocity and WSS reduction are parameters to predict aneurysm thrombosis. Acta Neurochirurgica, 154(10), 1827–1834.
Tang, A. Y. S., Chung, W. C., Liu, E. T. Y., Qu, J. Q., Tsang, A. C. O., Leung, G. K. K., et al. (2015). Computational fluid dynamics study of bifurcation aneurysms treated with pipeline embolization device: Side branch diameter study. Journal of Medical and Biological Engineering, 35(3), 293–304.
Chong, W., Zhang, Y., Qian, Y., Lai, L., Parker, G., & Mitchell, K. (2014). Computational hemodynamics analysis of intracranial aneurysms treated with flow diverters: Correlation with clinical outcomes. American Journal of Neuroradiology, 35(1), 136–142.
Xiang, J., Damiano, R. J., Lin, N., Snyder, K. V., Siddiqui, A. H., Levy, E. I., et al. (2015). High-fidelity virtual stenting: Modeling of flow diverter deployment for hemodynamic characterization of complex intracranial aneurysms. Journal of Neurosurgery, 123(4), 832–840.
Zhang, Y., Chong, W., & Qian, Y. (2013). Investigation of intracranial aneurysm hemodynamics following flow diverter stent treatment. Medical Engineering & Physics, 35(5), 608–615.
Qian, Y., Takao, H., Umezu, M., & Murayama, Y. (2011). Risk analysis of unruptured aneurysms using computational fluid dynamics technology: Preliminary results. American Journal of Neuroradiology, 32(10), 1948–1955.
Hu, P., Qian, Y., Lee, C., Zhang, H., & Ling, F. (2015). The energy loss may predict rupture risks of anterior communicating aneurysms: A preliminary result. International Journal of Clinical and Experimental Medicine, 8(3), 4128–4133.
Liu, J., Xiang, J., Zhang, Y., Wang, Y., Li, H., Meng, H., et al. (2014). Morphologic and hemodynamic analysis of paraclinoid aneurysms: Ruptured versus unruptured. Journal of Neurointerventional Surgery, 6, 658–663.
Farnoush, A., Avolio, A., & Qian, Y. (2013). Effect of bifurcation angle configuration and ratio of daughter diameters on hemodynamics of bifurcation aneurysms. American Journal of Neuroradiology, 34(2), 391–396.
Farnoush, A., Avolio, A., & Qian, Y. (2014). A growth model of saccular aneurysms based on hemodynamic and morphologic discriminant parameters for risk of rupture. Journal of Clinical Neuroscience, 21(9), 1514–1519.
Ren, X., Qiao, A., Song, H., Song, G., & Jiao, L. (2016). Influence of bifurcation angle on in-stent restenosis at the vertebral artery origin: a simulation study of hemodynamics. Journal of Medical and Biological Engineering, 36(4), 555–562.
Tsang, A. C., Tang, A. Y., Chung, W. C., Leung, G. K., & Chow, K. W. (2016). Correlating hemodynamic changes and occlusion time after flow diverter treatment of bilateral large internal carotid artery aneurysms. Clinical Neuroradiology, 26(4), 477–480.
Augsburger, L., Reymond, P., Rufenacht, D., & Stergiopulos, N. (2011). Intracranial stents being modeled as a porous medium: Flow simulation in stented cerebral aneurysms. Annals of Biomedical Engineering, 39(2), 850–863.
Sforza, D., Putman, C., & Cebral, J. (2009). Hemodynamics of cerebral aneurysms. Annual Review of Fluid Mechanics, 41, 91–107.
Cebral, J. R., Castro, M. A., Appanaboyina, S., Putman, C. M., Millan, D., & Frangi, A. F. (2005). Efficient pipeline for image-based patient-specific analysis of cerebral aneurysm hemodynamics: Technique and sensitivity. IEEE Transactions on Medical Imaging, 24(4), 457–467.
Shojima, M., Oshima, M., Takagi, K., Torii, R., Hayakawa, M., Katada, K., et al. (2004). Magnitude and role of wall shear stress on cerebral aneurysm—Computational fluid dynamic study of 20 middle cerebral artery aneurysms. Stroke, 35(11), 2500–2505.
Marzo, A., Singh, P., Larrabide, I., Radaelli, A., Coley, S., Gwilliam, M., et al. (2011). Computational hemodynamics in cerebral aneurysms: The effects of modeled versus measured boundary conditions. Annals of Biomedical Engineering, 39(2), 884–896.
Ku, D., Giddens, D., Zarins, C., & Glagov, S. (1985). Pulsatile flow and atherosclerosis in the human carotid bifurcation. Positive correlation between plaque location and low oscillating shear stress. Arteriosclerosis, Thrombosis, and Vascular Biology, 5(3), 293–302.
Reymond, P., Bohraus, Y., Perren, F., Lazeyras, F., & Stergiopulos, N. (2011). Validation of a patient-specific one-dimensional model of the systemic arterial tree. American Journal of Physiology-Heart and Circulatory Physiology, 301(3), H1173–H1182.
Benard, N., Coisne, D., Donal, E., & Perrault, R. (2003). Experimental study of laminar blood flow through an artery treated by a stent implantation: Characterisation of intra-stent wall shear stress. Journal of Biomechanics, 36(7), 991–998.
Berg, P., Iosif, C., Ponsonnard, S., Yardin, C., Janiga, G., & Mounayer, C. (2016). Endothelialization of over-and undersized flow-diverter stents at covered vessel side branches: An in vivo and in silico study. Journal of Biomechanics, 49(1), 4–12.
Womersley, J. R. (1955). Method for the calculation of velocity, rate of flow and viscous drag in arteries when the pressure gradient is known. The Journal of Physiology, 127(3), 553–563.
Pereira, V., Bonnefous, O., Ouared, R., Brina, O., Stawiaski, J., Aerts, H., et al. (2013). A DSA-based method using contrast-motion estimation for the assessment of the intra-aneurysmal flow changes induced by flow-diverter stents. American Journal of Neuroradiology, 34(4), 808–815.
Carty, G., Chatpun, S., & Espino, D. M. (2016). Modeling blood flow through intracranial aneurysms: A comparison of Newtonian and non-Newtonian viscosity. Journal of Medical and Biological Engineering, 36(3), 396–409.
ASME V&V 20. (2009). Standard for verification and validation in computational fluid dynamics and heat transfer. New York, NY: American Society of Mechanical Engineers.
Acknowledgements
Partial financial support was provided by the Innovation and Technology Support Program (ITS/150/15) of the Hong Kong Special Administrative Region Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Appendix
Appendix
Some technical details concerning the quality assurance of the accuracy of the simulations are given here. Two columns of data are listed in the following table, which describes the number of cells used in all utilized meshes. The parameter ‘Energy Loss’ was calculated at a time point when β had the largest variation across different meshes. The adjectives, ‘Large’, ‘Medium’ and ‘Small’ were then used to designate these meshes. According to [44], the Grid Convergence Index (GCI) was calculated and recorded for one of the cases.
- Case 1:
-
Successful case
- Case 1a:
-
Pre-operation
Details of the grid size are tabulated in Table 6. The number of cells utilized in this study was 539,662.
The ‘Energy Loss’ parameter was therefore quite insensitive to the number of cells (error < 0.5%) once a threshold was reached, a feature also illustrated in Fig. 12.
1.1 Analysis
The refinement ratio, r, was approximately 1.44, while the observed order of convergence, p, was very close to 2.50. For the three-grid study, a factor of safety (Fs), given by Fs = 1.25, was used to calculating the GCI for the finer grids [44]. Using these established procedures, the standard calculations yielded:
A quality assurance check was conducted to test whether the solutions were in the asymptotic range:
This value of approximate unity thus confirmed that the solution was within the appropriate asymptotic range. Similar patterns were observed for other simulations reported in the text.
Rights and permissions
About this article
Cite this article
Chiu, T.L., Tang, A.Y.S., Tsang, A.C.O. et al. A Computational Hemodynamics Analysis on the Correlation Between Energy Loss and Clinical Outcomes for Flow Diverters Treatment of Intracranial Aneurysm. J. Med. Biol. Eng. 39, 27–42 (2019). https://doi.org/10.1007/s40846-018-0376-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-018-0376-z