Abstract
Purpose
Recent evidence indicates that people with normal glucose tolerance (NGT) but 1-h post-load plasma glucose (1-h OGTT) ≥ 155 mg/dl have an increased risk for developing Type 2 diabetes mellitus (T2DM), determining a new risk category with deeper metabolic impairment. The aim of this study was to identify, among women with gestational diabetes (GDM), which alterations at OGTT during pregnancy are more frequently associated with 1-h OGTT ≥ 155 mg/dl at post-partum examination.
Methods
Among 297 women affected by GDM, we retrospectively evaluated 244 resulted NGT after delivery. Based on post-partum glucose levels at 1-h OGTT, these people were divided into 188 cases (77.0%) with 1-h OGTT < 155 mg/dl (L-NGT) and 56 (23.0%) with 1-h OGTT ≥ 155 mg/dl (H-NGT).
Results
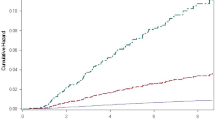
Abnormal glucose levels at 1-h OGTT during pregnancy (≥ 180 mg/dl) were more frequent in H-NGT than in L-NGT (39.3 vs. 24.6%, odds ratio 3.7 [95% CI 1.4–9.6]; p = 0.016). Moreover, H-NGT showed more frequently the simultaneous alteration of all three OGTT plasma glucose values during pregnancy (10.7 vs. 2.1%, odds ratio 4.5 [95% CI 1.5–20.3]; p = 0.038) and less frequently the alteration of fasting plasma glucose alone (14.3 vs. 30.8%, odds ratio 0.4 [95% CI 0.1–0.7]; p = 0.028).
Conclusions
Abnormal 1-h OGTT during pregnancy predicts an increased risk for post-partum 1-h OGTT ≥ 155 mg/dl in women with previous GDM. Even if NGT after delivery, these women may require a closer long-term post-partum follow-up, being at higher risk to develop future glucose intolerance.


Similar content being viewed by others
References
American Diabetes Association (2016) Standards of medical care in diabetes—2016. Diabetes Care 39(suppl 1):S1–S112
Associazione Medici Diabetologi (AMD)—Società Italiana di Diabetologia (SID) (2016) Standard italiani per la cura del diabete mellito 2016. Available at http://www.standarditaliani.it. Accessed 18 Apr 2017
Ferrara A (2007) Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care 30:S141–S146
American Diabetes Association (2004) Gestational diabetes mellitus. Diabetes Care 27:S88–S90
Nesbitt TS, Gilbert WM, Herrchen B (1998) Shoulder dystocia and associated risk factors with macrosomic infants born in California. Am J Obstet Gynecol 179:476–480
Kim C, Newton KM, Knopp RH (2002) Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 25:1862–1868
Chiefari E, Arcidiacono B, Foti D, Brunetti A (2017) Gestational diabetes mellitus: an updated overview. J Endocrinol Invest. doi:10.1007/s40618-016-0607-5
HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358:1991–2002
Committee on Obstetric Practice (2009) ACOG Committee Opinion No. 435: postpartum screening for abnormal glucose tolerance in women who had gestational diabetes mellitus. Obstet Gynecol 113:1419–1421
Hunt KJ, Conway DL (2008) Who returns for postpartum glucose screening following gestational diabetes mellitus? Am J Obstet Gynecol 198(404):e1–e6
Lawrence JM, Black MH, Hsu JW, Chen W, Sacks DA (2010) Prevalence and timing of postpartum glucose testing and sustained glucose dysregulation after gestational diabetes mellitus. Diabetes Care 33:569–576
Russell MA, Phipps MG, Olson CL, Welch HG, Carpenter MW (2006) Rates of postpartum glucose testing after gestational diabetes mellitus. Obstet Gynecol 108:1456–1462
Almario CV, Ecker T, Moroz LA, Bucovetsky L, Berghella V, Baxter JK (2008) Obstetricians seldom provide postpartum diabetes screening for women with gestational diabetes. Am J Obstet Gynecol 198(528):e1–e5
Abdul-Ghani MA, Abdul-Ghani T, Ali N, Defronzo RA (2008) One-hour plasma glucose concentration and the metabolic syndrome identify subjects at high risk for future type 2 diabetes. Diabetes Care 31:1650–1655
Abdul-Ghani MA, Lyssenko V, Tuomi T, Defronzo RA, Groop L (2009) Fasting versus postload plasma glucose concentration and the risk for future type 2 diabetes: results from the Botnia Study. Diabetes Care 32:281–286
Priya M, Anjana RM, Chiwanga FS, Gokulakrishnan K, Deepa M, Mohan V (2013) 1-hour venous plasma glucose and incident prediabetes and diabetes in Asian Indians. Diabetes Technol Ther 15:497–502
Succurro E, Marini MA, Arturi F, Grembiale A, Lugarà M, Andreozzi F et al (2009) Elevated 1-hour post-load plasma glucose levels identifies subjects with normal glucose tolerance but early carotid atherosclerosis. Atherosclerosis 207:245–249
Sciacqua A, Miceli S, Carullo G, Greco L, Succurro E, Arturi F et al (2011) One-hour postload plasma glucose levels and left ventricular mass in hypertensive patients. Diabetes Care 34:1406–1411
Marini MA, Succurro E, Frontoni S, Mastroianni S, Arturi F, Sciacqua A et al (2012) Insulin sensitivity, beta-cell function, and incretin effect in individuals with elevated 1-hour post-load plasma glucose levels. Diabetes Care 35:868–872
Sesti G, Fiorentino TV, Succurro E, Perticone M, Arturi F, Sciacqua A et al (2014) Elevated 1-h post-load plasma glucose levels in subjects with normal glucose tolerance are associated with unfavorable inflammatory profile. Acta Diabetol 51:927–932
Fiorentino TV, Marini MA, Andreozzi F, Arturi F, Succurro E, Perticone M et al (2015) One-Hour Postload Hyperglycemia is a stronger predictor of type 2 diabetes than impaired fasting glucose. J Clin Endocrinol Metab 100:3744–3751
Bianchi C, Miccoli R, Trombetta M, Giorgino F, Frontoni S, Faloia E, GENFIEV Investigators et al (2013) Elevated 1-hour postload plasma glucose levels identify subjects with normal glucose tolerance but impaired β-cell function, insulin resistance, and worse cardiovascular risk profile: the GENFIEV study. J Clin Endocrinol Metab 98(5):2100–2105. doi:10.1210/jc.2012-3971
Carpenter MW, Coustan DR (1982) Criteria for screening tests for gestational diabetes. Am J Ostet Gynecol 144(7):768–773
International Association of Diabetes and Pregnancy Study Groups Consensus Panel (2010) International Association Of Diabetes And Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682
Cozzolino M, Serena C, Maggio L, Rambaldi MP, Simeone S, Mello G, Pasquini L, Di Tommaso M, Mecacci F (2017) Analysis of the main risk factors for gestational diabetes diagnosed with International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria in multiple pregnancies. J Endocrinol Invest. doi:10.1007/s40618-017-0646-6
Unwin N, Shaw J, Zimmet P, Alberti KG (2002) Impaired glucose tolerance and impaired fasting glycemia: the current status on definition and intervention. Diabet Med 19:708–723
Kuang L, Huang Z, Hong Z, Chen A, Li Y (2015) Predictability of 1-h postload plasma glucose concentration: a 10-year retrospective cohort study. J Diabetes Investig 6:647–654. doi:10.1111/jdi.12353
Bellamy L, Casas JP, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373:1773–1779
Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R (2007) Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 30:753–759
Abdul-Ghani MA, Tripathy D, DeFronzo RA (2006) Contributions of beta-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting Glucose. Diabetes Care 29:1130–1139
Laakso M, Zilinskaite J, Hansen T, Boesgaard TW, Väntinnen M, Stancáková A (2008) Insulin sensitivity, insulin release and glucagon-like peptide-1 levels in persons with impaired fasting glucose and/o impaired glucose tolerance in the EUGENE2 study. Diabetologia 51:502–511
Acknowledgements
The authors thank Prof. Giuliana Arcidiacono, Ph.D. in English and Anglo-American Studies, University of Catania, for the language revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
RV. participated in the Novo Nordisk Advisory Board in 2015 and 2016. L.S. participated in the Lilly Advisory Board in 2017. The other authors have nothing to disclose.
Ethical approval
The ethical committee approval is not required in our institution for retrospective studies. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and its later amendments.
Informed consent
For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tumminia, A., Milluzzo, A., Cinti, F. et al. Abnormal 1-hour post-load glycemia during pregnancy impairs post-partum metabolic status: a single-center experience. J Endocrinol Invest 41, 567–573 (2018). https://doi.org/10.1007/s40618-017-0774-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0774-z