Abstract
Purpose
Since the American Diabetes Association included hemoglobin A1c (HbA1c) in the diagnostic criteria for diabetes in 2010, the clinical use of HbA1c has remained controversial. We explored the use of HbA1c for diagnosing diabetes and intermediate hyperglycemia in comparison with fasting plasma glucose (FPG).
Methods
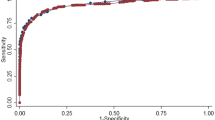
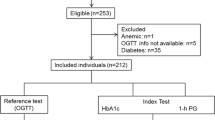
We screened 3710 adult subjects (mean age = 55.24 years) comprising 1704 males and 2006 females. We drew an receiver operating characteristic (ROC) curve to evaluate the ability of HbA1c to diagnose diabetes and intermediate hyperglycemia according to FPG. We used Kappa coefficient and Pearson’s correlation coefficient to evaluate the relationship between HbA1c and FPG in different FPG ranges.
Results
The areas under ROC curve to diagnose diabetes and intermediate hyperglycemia were 0.859 (95 % CI 0.827–0.892) and 0.633 (95 % CI 0.615–0.651). The kappa coefficients between FPG and HbA1c for diagnosis of diabetes and intermediate hyperglycemia were 0.601 (P < 0.001) and 0.104 (P < 0.001). The Pearson’s correlation coefficient of FPG and HbA1c was 0.640 (P < 0.001), but when we classified FPG as normal, intermediate hyperglycemia and diabetes, the coefficients became 0.07 (P = 0.002), 0.185 (P < 0.001) and 0.760 (P < 0.001), respectively.
Conclusions
The relationship between HbA1c and FPG changed according to the different FPG ranges. When FPG was higher, the relationship was stronger. HbA1c and FPG were highly consistent in diagnosing diabetes, but they were not in predicting intermediate hyperglycemia.



Similar content being viewed by others
References
Beckman JA, Libby P (2002) Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA 287(19):2570–2581
American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33(Suppl. 1):S62–S69
Rahbar S (1968) An abnormal haemoglobin in red cells of diabetics. Clin Chim Acta 22:296–298
Bianchi C, Miccoli R, Bonadonna RC, Giorgino F, Frontoni S, Faloia E, Marchesini G, Dolci MA, Cavalot F, Cavallo GM, Leonetti F, Del Prato S, Investigators GENFIEV (2012) Pathogenetic mechanisms and cardiovascular risk: differences between HbA1c and oral glucose tolerance test for the diagnosis of glucose tolerance. Diabetes Care 35(12):2607–2612
Lipska KJ, De Rekeneire N, Van Ness PH, Johnson KC, Kanaya A, Koster A, Strotmeyer ES, Goodpaster BH, Harris T, Gill TM, Inzucchi SE (2010) Identifying dysglycemic states in older adults: implications of the emerging use of hemoglobin A1c. J Clin Endocrinol Metab 95:5289–5295
Kumaravel B, Bachmann MO, Murray N, Dhatariya K, Fenech M, John WG, Scarpello TJ, Sampson MJ, University of East Anglia Impaired Fasting Glucose (UEA-IFG) Study Group (2012) Use of haemoglobin A1c to detect impaired fasting glucose or type 2 diabetes in a United Kingdom community based population. Diabetes Res Clin Pract 96(2):211–216
Kim CH, Kim HK, Bae SJ, Park JY, Lee KU (2011) Discordance between fasting glucose-based and hemoglobin A1c-based diagnosis of diabetes mellitus in Koreans. Diabetes Res Clin Pract 91(1):e8–e10
Inoue K, Matsumoto M, Kobayashi Y (2007) The combination of fasting plasma glucose and glycosylated hemoglobin predicts type 2 diabetes in Japanese workers. Diabetes Res Clin Pract 77(3):451–458
Droumaguet C, Balkau B, Simon D, Caces E, Tichet J, Charles MA, Eschwege E, DESIR Study Group (2006) The DESIR Study Group: use of HbA1C in predicting progression to diabetes in French men and women data from an epidemiological study on the insulin resistance syndrome (DESIR). Diabetes Care 29(7):1619–1625
Motta M, Bennati E, Cardillo E, Ferlito L, Malaguarnera M (2010) The value of glycosylated hemoglobin (HbA1c) as a predictive risk factor in the diagnosis of diabetes mellitus (DM) in the elderly. Arch Gerontol Geriatr 50(1):60–64
Olson DE, Rhee MK, Herrick K, Ziemer DC, Twombly JG, Phillips LS (2010) Screening for diabetes and pre-diabetes with proposed A1C-based diagnostic criteria. Diabetes Care 33(10):2184–2189
Nair M, Prabhakaran D, Narayan KM, Sinha R, Lakshmy R, Devasenapathy N, Daniel CR, Gupta R, George PS, Mathew A, Tandon N, Reddy KS (2011) HbA1c values for defining diabetes and impaired fasting glucose in Asian Indians. Prim Care Diabetes 5(2):95–102
Bennett CM, Guo M, Dharmage SC (2007) HbA(1c) as a screening tool for detection of type 2 diabetes: a systematic review. Diabet Med 24(4):333–343
van’t Riet E, Alssema M, Rijkelijkhuizen JM, Kostense PJ, Nijpels G, Dekker JM (2010) Relationship between A1C and glucose levels in the general Dutch population: the new Hoorn study. Diabetes Care 33(1):61–66
Kim HY, Lee SY, Suh S, Kim JH, Lee MK, Park HD (2013) The relationship between estimated average glucose and fasting plasma glucose. Clin Chem Lab Med 51(11):2195–2200
Sun X, Du T, Huo R, Xu L (2014) Hemoglobin A1c as a marker for identifying diabetes and cardiovascular risk factors: the China Health and Nutrition Survey 2009. Acta Diabetol 51(3):353–360
Lee JM, Wu EL, Tarini B, Herman WH, Yoon E (2011) Diagnosis of diabetes using hemoglobin A1c: should recommendations in adults be extrapolated to adolescents? J Pediatr 158(6):947–952 e1–e3
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, Wang L, Jiang Y, Dai M, Lu J, Xu M, Li Y, Hu N, Li J, Mi S, Chen CS, Li G, Mu Y, Zhao J, Kong L, Chen J, Lai S, Wang W, Zhao W, Ning G, 2010 China Noncommunicable Disease Surveillance Group (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310(9):948–959
Groche D, Hoeno W, Hoss G, Vogt B, Herrmann Z, Witzigmann A (2003) Standardization of two immunological HbA1c routine assays according to the new IFCC reference method. Clin Lab 49(11–12):657–661
Metus P, Ruzzante N, Bonvicini P, Meneghetti M, Zaninotto M, Plebani M (1999) Immunoturbidimetric assay of glycated hemoglobin. J Clin Lab Anal 13(1):5–8
Chang J, Hoke C, Ettinger B, Penerian G (1998) Evaluation and interference study of hemoglobin A1c measured by turbidimetric inhibition immunoassay. Am J Clin Pathol 109(3):274–278
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
The study was approved by the Ethics Committee of China Medical University.
Informed consent
Informed and written consent was obtained from each participant.
Rights and permissions
About this article
Cite this article
Guan, X., Zheng, L., Sun, G. et al. The changing relationship between HbA1c and FPG according to different FPG ranges. J Endocrinol Invest 39, 523–528 (2016). https://doi.org/10.1007/s40618-015-0389-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-015-0389-1