Abstract
Purpose of Review
The management of chronic wounds, a debilitating condition, presents a considerable challenge to healthcare professionals and a significant burden on services. When these wounds are exposed to the external environment, they are susceptible to microbial infection, which further complicates their management and worsens clinical outcomes.
Recent Findings
Bacteria typically exist in wounds as part of a biofilm, which is often polymicrobial in nature, alongside bacteria and fungi that are described as being more virulent and tolerant towards antimicrobials and antiseptics. Despite advancing knowledge in polymicrobial biofilm wound infections with respect to bacteria, the role of fungi is largely ignored, and their influence in chronicity and clinical management is not fully appreciated or understood.
Summary
The purpose of this review is to explore the significance of fungi within chronic wound environments and, in doing so, understand the importance of interkingdom interactions in wound management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic wounds are simply acute wounds that do not follow traditional healing processes. Although their definition is somewhat simple, the management of chronic wounds can be complex, resulting in wound management costing an estimated £8.3 billion in the UK [1]. This failure to properly heal can arise due to several factors, such as a dysregulated immune system or microbial infection [2]. Chronic wounds encompass a number of different wounds, such as diabetic foot ulcers (DFUs), venous leg ulcers, and pressure ulcers [2]. DFUs, in particular, are associated with alarmingly high mortality rates that are comparable to cancer, and in some cases, mortality rates can be higher, such as in the case of pancreatic and breast cancer [3, 4]. Although genetic and environmental factors contribute towards healing failure and mortality rates, wound infection also contributes significantly. However, administering effective treatments for these infections is accompanied by the problem of the discerning commensal, opportunist from a pathogen. Therefore, understanding who the ‘usual suspects’ are expected to be present as part of the skin microflora can aid in solving this puzzle.
With the ever-increasing accessibility of next-generation sequencing (NGS) methods, our ability to delve into the world of the human microbiome to identify microorganisms that are important in health and disease has increased in tandem. This has meant that our knowledge of organisms presents within the microbiome of infected wound beds has increased in recent years. The bacterial microbiome of the skin and chronic wounds is well-defined. This largely depends on the environment of the skin site. For example, Cutibacterium spp. was more abundant in sebaceous sites and genera such as Staphylococcus and Corynebacterium spp. dominated more moist sites such as the feet and inside of knee and elbow creases [5].
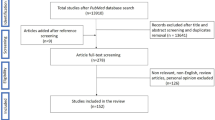
Studying the microbiome of chronic wounds has been a subject of great interest in recent years, with 32 studies being identified covering 4880 patients as identified in our own PubMed search in March 2022 (data not shown) using the following terms adapted from a recent microbiome meta-analysis [6]: ((wound OR diabet* foot OR diabet* foot ulcer OR DFU OR laceration OR ischemic OR neuropathic OR pressure) NOT (review)) AND ((microb* OR bacteri* OR archea* OR fung* OR mycob*) AND (structure OR composition OR diversity OR community) AND (sequencing OR metabarcoding OR amplicon OR metagenom* OR 16S OR “ITS”)). In a large-scale microbiome study performed by Wolcott and colleagues (2016), the microbiome of 2963 chronic wound samples from DFUs, nonhealing surgical wounds, venous leg ulcers, and decubitus ulcers was defined [7]. Results from these analyses identified Staphylococcus, Pseudomonas, Corynebacterium, and Streptococcus as the most abundant genera in all wound types. Additionally, the top 20 most abundant genera in all samples showed comparable levels of diversity and abundance across each wound type. Based on the findings of this study, neither wound type nor patient demographics influence the microbial composition of the chronic wound microbiome. However, a feature of these analyses that is missing is a consideration of how these organisms grow together within the wound environment. Indeed, there is unequivocal evidence that the biofilm phenotype is a dominant feature of chronic wounds, with a meta-analysis identifying nearly 80% of cases with biofilms, accompanied by increased antimicrobial tolerance and virulence [8•].
Wound Biofilms: a Limited Viewpoint on Bacteria
Biofilms have been classically defined as a community of cells adhered to a surface, encased in a self-produced extracellular matrix (ECM). Microorganisms that transition from free-floating to sessile, biofilm cells exhibit increased antimicrobial tolerance and virulence compared to their planktonic counterparts [9, 10]. This biofilm-associated phenotype can often complicate the management of DFUs and chronic wounds. However, it is worth noting that biofilms in vivo, particularly those in chronic wounds, differ from the traditional ‘mushroom-like’ structure that was first described in Pseudomonas grown under continuous-flow conditions, whereby bacterial cells adhere and multiply, forming a ‘stalk’ that then blooms outwards, creating a shape reminiscent of a closed-cup mushroom. Despite this, they still possess the traits normally associated with biofilms, such as increased virulence and antimicrobial tolerance, which come as a result of ECM production [11]. Biofilms in chronic wounds have adhered to one another more so than they are bound to the host or one another, and this creates a smaller, aggregation of cells between 5 and 200 µm in diameter [12]. These non-surface-attached aggregates are now well described and are part of a reconceptualised thinking of the biofilm lifecycle, though notably excluding the role of fungi [13].
Early studies that focused on biofilm infections in chronic wounds gave particular attention to bacteria such as Pseudomonas aeruginosa, an opportunistic pathogen that is not often found as part of the healthy skin microbiome, but can be readily isolated from chronic wounds [5, 14]. These studies showed that P. aeruginosa also formed bacterial aggregates within the host and utilised an arsenal of virulence factors such as the LasR quorum sensing system [11]. While many studies have focused on single-species biofilms, it is important to note that the chronic wound microbiome is a complex entity; therefore, studies must give attention to multi-species biofilms. To date, several multi-species biofilm models exist to study chronic wounds, all of which favour S. aureus and P. aeruginosa (Table 1). A number of these make use of the Lubbock chronic wound biofilm (LCWM) model, which utilises Bolton broth, plasma, and lysed blood [15]. The benefit of this growth media is that biofilms formed by coagulase-positive organisms such as S. aureus result in the formation of aggregates that mimic the biofilm phenotype observed in vivo [15].
Previous studies have highlighted the increased recalcitrance to antimicrobials of multi-species biofilms compared to single-species biofilms. In a rat model, higher rates of infection were observed from a dual-species inoculum consisting of S. aureus and P. aeruginosa [16]. Similarly, the anaerobic bacteria, Prevotella bivia increases S. aureus pathogenicity in a murine infection model [17]. A study by Dalton and colleagues showed similar findings when using a multi-species bacterial biofilm model to interrogate inter-species interactions. These complex multi-species biofilms, containing Enterococcus faecalis, Finegoldia magna, P. aeruginosa, and S. aureus, resulted in healing impairment while remaining viable over a period of 12 days. These authors reported a decrease in wound healing and increased antimicrobial tolerance to treatments compared to single-species biofilm counterparts [18].
Although the addition of multiple species to biofilm models increases their relevance, it is important to note the utilisation of appropriate growth media and substrates to effectively mimic in vivo conditions [19]. A recent publication evaluated the role of dual-species biofilms formed by P. aeruginosa and Staphylococcus aureus in chronic wounds using a novel, layered substrate [20•]. To create this model, firstly, a subcutaneous fat layer was created and this was followed by a surrogate dermis layer, before the addition of bacterial inoculum. Following bacteria growth, this model more accurately represented the biofilm phenotype often seen in vivo and supported viable bacteria for up to 9 days, which could be used to test antimicrobial washes and dressings. Authors showed these dressings only exhibited a mild anti-biofilm effect, which agrees with clinical findings and highlights the importance of using appropriate substrates and conditions when studying disease biology in vitro [20•, 21]. This study makes a large step in the right direction concerning the development of accurate and reproducible chronic wound biofilms, though remarkably, these models fail to take into account the role of fungi.
Deciphering the Role of Fungi in Chronic Wounds
Despite having a general definition that covers all microorganisms within a biological niche, the word ‘microbiome’ is typically used to specifically reference bacteria, and separate terms such as virome and archaeome are now employed to specify between viruses and archaea, respectively. The mycobiome, which is specific to fungi, is an under-represented and under-appreciated area of microbiome research. For example, in the gut, fungi comprise less than 1% of all microorganisms [22]. However, there are several arguments to suggest that fungi are more important than previously thought. Being more than 100 times larger than bacteria, fungi make up a considerable part of the collective microbiota biomass in addition to causing infections with high levels of morbidity and mortality.
As the first line of defence against foreign microorganisms, the skin is home to a myriad of bacteria, fungi, and viruses [23]. Using culture-dependant techniques, Malassezia, Aspergillus, and Candida species are recognised as some of the most cultured fungi from the skin. This has then been confirmed using NGS [24, 25]. Despite being readily identified and isolated from healthy skin, the role that fungi play in chronic wounds and how they alter regular wound healing mechanisms is still debated within the literature. The role of fungi in health and disease is subject to debate, not just in chronic wounds but also in respiratory and oral infections [26]. With this being said, Chellan and colleagues identified fungi infecting diabetic foot ulcers (DFUs) in 22% of patients, with Candida spp. being the most abundant [27]. More recently, culture-independent studies have identified fungi in up to 80% of samples [25]. Not only does this reinforce previous reports that culture-dependant techniques underestimate microbial colonisation and infection rates, but also indicates that previous predictions stating fungi are mere ‘bystanders’ to chronic wound infections are worth rethinking as they likely play a more active role in infection.
The mycobiome composition is often determined by the body site, much like its bacterial counterpart, with Malassezia spp., dominating most sites. However, the mycobiome of the foot and more moist areas is far more diverse and is comprised of genera such as Candida, Aspergillus, and Penicillium [23]. Findings by Kalan and co-workers (2016) showed that an increased abundance of Ascomycota is significantly associated with longer healing times [25]. These reports show that the mycobiome may influence wound healing in a similar way to that of the bacterial microbiota, where increased bacterial diversity is associated with longer healing times [28].
Fungi have a reputation for being opportunistic pathogens, so combining an open wound with antibiotics (given as a first-line treatment option) and fungi colonising the surrounding skin creates an ideal environment for fungal infection. Despite this obvious logic, fungi are often the subject of debate in disease biology as they are often thought to not play any active role in infection, though there is substantial evidence from the oral cavity that this is not the case [29]. An initial study in 2010 with the intention of identifying fungal infection in wounds in diabetes patients found fungal infections in nearly 30% of cases, with Candida spp. being the most prevalent, followed by members of the Aspergillus and Trichosporon genera [27]. For Candida spp., in particular, it has been shown that conditions in diabetic wounds and ulcers are optimal for inducing a shift from commensal to a pathogen. Higher blood glucose levels result in Candida isolates displaying a higher degree of enzyme activity, which is hypothesised to make these organisms more virulent [30]. These clinical studies highlight the importance of considering fungi in chronic wounds and should also drive consideration for antifungal therapy.
Challenges of Studying the Mycobiome
As previously stated, there are significant discrepancies between culture-dependent and independent methodologies in microorganism identification [31]. Despite the increased sensitivity that comes with molecular diagnostics such as NGS, the application of this to the mycobiome as a diagnostic method does not come without its downfalls. Challenges in mycobiome research come at many stages, from sample processing to the final data analysis stages. For example, some challenges are common across micro- and mycobiome studies, such as untimely processing or freezing of samples, and repeated freeze-thawing of samples can influence microbiota diversity [32, 33]. Additionally, harsher methods of cell lysis are required due to the robust nature of the fungal cell wall; therefore, the choice of DNA extraction method is important. For instance, chemical/enzymatic lysis can increase DNA yields while favouring the lysis of yeasts (e.g. C. albicans), whereas physical lysis produces higher DNA yields in filamentous fungi such as Aspergillus fumigatus [34, 35]. Issues can also arise in the data analysis and bioinformatic stages with incomplete fungal reference databases, leading to large numbers of unclassified operational taxonomic units (OTUs) [36]. Several other factors contribute towards the difficulties of mycobiome research. However, the minutia of details behind these which fall out with the scope of this review has been extensively reviewed by Tiew and colleagues [37].
Modelling Interkingdom Wound Biofilms
There is growing evidence to support the notion that bacteria and fungi influence one another’s behaviour, which in turn can have a clinical impact [38]. However, these interactions are best studied in vitro to gain a deeper understanding of the antagonistic and synergistic virulence potential of interkingdom interactions. Therefore, it is important to model these infections to accurately study the functionality of the chronic wound microbiome. Although a number of research groups have developed multi-species biofilm models to study microbial dynamics within chronic wounds (Table 1), these are largely devoid of fungi within their composition.
A multi-species biofilm model containing C. albicans and the prolific wound pathogens, Staphylococcus aureus and Pseudomonas aeruginosa, was initially described by our group, and was one of the first to consider fungi in these models. The data showed that the presence of C. albicans was responsible for driving the recalcitrant nature of the biofilm, where antimicrobial treatments merely influenced biofilm composition rather than reducing overall biofilm biomass [39]. Although these data highlight the importance of fungi within wound infections, it is limited to a small number of species. We therefore enhanced the complexity of the model to a complex, 11-species interkingdom biofilm model adjacent to 3-dimensional tissue [40•]. This biofilm consortium more accurately models wound conditions by the inclusion of additional aerobic and anaerobic bacteria. Data from this study showed that although challenging wound biofilms with antiseptics can significantly reduce viable biofilm cells, a considerable portion of the biofilm remains. The residual biofilm cells that were able to persist following antiseptic exposure presented differential stimulatory effects within the epidermis model, with H2O2 and povidone-iodine being perhaps the more appropriate antiseptics due to their more effective immune-modulatory effects [40•]. Additionally, this study highlighted how differing atmospheric O2 concentrations can influence the overall composition of the biofilm, with C. albicans dominating biofilms grown in O2 and CO2 conditions, whereas Staphylococcus hominis dominated biofilms growing in anaerobic environments. These data further stress the point made above, in that the conditions in that biofilm models are constructed should be carefully considered to effectively replicate in vivo conditions.
Fungal-Bacterial Biofilm Interactions
With a myriad of different organisms inhabiting chronic wounds, understanding the interactions between these organisms is crucial in understanding their roles in disease. There are numerous bacteria-bacteria interactions that take place within wound environments, which have been well documented elsewhere [41]. However, fungal-bacterial interactions are less well known. Many studies focusing on these interactions do so in the context of oral or respiratory disease, meaning not only should findings be translated to chronic wounds with caution, but also more studies must study interkingdom dynamics in a chronic wound model.
Candida—Staphylococcus Interactions
Interactions between fungi and bacteria found in DFU infections may drive antimicrobial tolerance and virulence [40•]. For example, a well-studied interkingdom relationship between C. albicans and S. aureus, two organisms often found in DFUs and chronic wounds are known to increase S. aureus tolerance to antibiotics by increasing extracellular DNA production and fungal ECM components, as well as increasing virulence by upregulating the agr quorum sensing pathway, resulting in increased toxin production [42,43,44]. This increase in tolerance and virulence is reciprocal, which has been confirmed by S. aureus upregulating C. albicans biofilm and virulence genes (Fig. 1) [45]. The presence of C. albicans within an interkingdom chronic wound biofilm was identified as a driving force behind antimicrobial tolerance, highlighting the importance of fungi in wound biofilms and why targeting the fungal scaffold within these biofilms may yield more positive treatment outcomes [39].
Interkingdom biofilm interactions. Interactions between C. albicans and bacteria of interest have been summarised to highlight their implications. S. aureus and C. albicans possess a synergistic interaction with the fungus, driving bacterial tolerance and biofilm formation, while S. aureus returns the favour by increasing fungal biofilm formation and virulence. However, C. albicans interactions with P. aeruginosa and Strep. agalactiae are more complex, with some beneficial and some antagonistic interactions occurring. For example, P. aeruginosa kills hyphal cells while quorum-sensing molecules drive efflux pump activity. Similarly, on one hand, Strep. agalactiae represses filamentation by downregulating HWP and EFG, whereas on the other, it binds directly to C. albicans hyphae to promote its own growth
Candida—Streptococcus Interactions
Another bacterial genus commonly found in the chronic wound microbiome is Streptococcus [14]. Streptococcus agalactiae is the most abundant species of Streptococcus found in chronic wounds, and unlike many other members of the Streptococcus genus, interactions between this bacterium and C. albicans are still subject to debate, with some reports stating Strep. agalactiae inhibiting C. albicans hyphal formation by repressing expression of HWP and EFG [46]. However, others report that C. albicans increases Strep. agalactiae colonisation in a murine infection model, while also documenting the presence of hyphae in these infections [47]. Additional studies are in agreement that interactions between C. albicans and group B Streptococci, such as Strep. agalactiae, are beneficial for organisms, with close binding occurring between fungus and bacterium, which likely promotes bacterial colonisation and virulence (Fig. 1) [48]. It is important to note that the absence of hyphae may not necessarily come as a detriment to C. albicans. For example, as hyphae are highly immunogenic, maintaining a budding yeast phenotype may help promote chronic colonisation in the wound bed. This is in line with a recent study whereby P. aeruginosa wound isolates were defective in virulence functions, suggesting such factors are not required for microbial fitness in wounds [49].
Candida—Pseudomonas Interactions
An interkingdom consortium that is also commonplace within wound environments is that of C. albicans and P. aeruginosa [50]. The interactions that occur between these two organisms are more complex than that of Staphylococcus, as interactions primarily happen indirectly via quorum-sensing molecules rather than direct binding, and antagonistic and synergistic interactions can seemingly take place simultaneously. For example, P. aeruginosa induces upregulation of C. albicans stress pathways, killing hyphal cells [51, 52]. While on the other hand, using transcriptomic and proteomic approaches, Bandara and colleagues showed that P. aeruginosa quorum sensing also promotes fluconazole resistance in C. albicans through upregulation of efflux pumps and ergosterol biosynthesis (Fig. 1) [53]. Despite many antagonistic interactions taking place in vitro, their behaviour in vivo appears more synergistic with ventilator-associated pneumonia patients; colonised by Candida, who are at a much greater risk of P. aeruginosa infection [54].
Conclusion
Although reports describing the importance of fungi within biofilms are limited, there exists growing evidence suggesting that they play an active role within infected wounds to be considered when advising treatment regimens. However, to acquire a better understanding of the role of fungal and polymicrobial biofilms within chronic wounds and to develop more effective treatment strategies, additional studies that acknowledge the fungal component of interkingdom biofilms are required.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Guest JF, Fuller GW, Vowden P. Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open. 2020;10(12):e045253.
Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care (New Rochelle). 2015;4(9):560–82.
Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res. 2020;13(1):16.
Armstrong DG, Wrobel J, JM R. Guest editorial: are diabetes-related wounds and amputations worse than cancer? Int Wound J. 2007;4(4):286–7.
Oh J, Byrd AL, Park M, Kong HH, Segre JA. Temporal stability of the human skin microbiome. Cell. 2016;165(4):854–66.
Butcher MC, Short B, Veena CLR, Bradshaw D, Pratten JR, McLean W, et al. Meta-analysis of caries microbiome studies can improve upon disease prediction outcomes. APMIS. 2022;130:763.
Wolcott RD, Hanson JD, Rees EJ, Koenig LD, Phillips CD, Wolcott RA, et al. Analysis of the chronic wound microbiota of 2,963 patients by 16S rDNA pyrosequencing. Wound Repair Regen. 2016;24(1):163–74.
• Malone M, Bjarnsholt T, McBain AJ, James GA, Stoodley P, Leaper D, et al. The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. J Wound Care. 2017;26(1):20–5. This systematic review highlights the importance of biofilms in chronic wounds and reports that they are found in 80% of cases.
Di Domenico EG, Farulla I, Prignano G, Gallo MT, Vespaziani M, Cavallo I, et al. Biofilm is a major virulence determinant in bacterial colonization of chronic skin ulcers independently from the multidrug resistant phenotype. Int J Mol Sci. 2017;18(5):1077.
Høiby N, Bjarnsholt T, Givskov M, Molin S, Ciofu O. Antibiotic resistance of bacterial biofilms. Int J Antimicrob Agents. 2010;35(4):322–32.
Bjarnsholt T, Kirketerp-Møller K, Jensen PØ, Madsen KG, Phipps R, Krogfelt K, et al. Why chronic wounds will not heal: a novel hypothesis. Wound Repair Regen. 2008;16(1):2–10.
Bjarnsholt T, Alhede M, Alhede M, Eickhardt-Sørensen SR, Moser C, Kühl M, et al. The in vivo biofilm. Trends Microbiol. 2013;21(9):466–74.
Sauer K, Stoodley P, Goeres DM, Hall-Stoodley L, Burmølle M, Stewart PS, et al. The biofilm life cycle: expanding the conceptual model of biofilm formation. Nat Rev Microbiol. 2022;20(10):608–20.
Smith K, Collier A, Townsend EM, O’Donnell LE, Bal AM, Butcher J, et al. One step closer to understanding the role of bacteria in diabetic foot ulcers: characterising the microbiome of ulcers. BMC Microbiol. 2016;16:54.
Sun Y, Dowd SE, Smith E, Rhoads DD, Wolcott RD. In vitro multispecies Lubbock chronic wound biofilm model. Wound Repair Regen. 2008;16(6):805–13.
Hendricks KJ, Burd TA, Anglen JO, Simpson AW, Christensen GD, Gainor BJ. Synergy between Staphylococcus aureus and Pseudomonas aeruginosa in a rat model of complex orthopaedic wounds. JBJS. 2001;83(6):855–61.
Mikamo H, Kawazoe K, Izumi K, Watanabe K, Ueno K, Tamaya T. Studies on the pathogenicity of anaerobes, especially Prevotella bivia, in a rat pyometra model. Infect Dis Obstet Gynecol. 1998;6(2):61–5.
Dalton T, Dowd SE, Wolcott RD, Sun Y, Watters C, Griswold JA, et al. An in vivo polymicrobial biofilm wound infection model to study interspecies interactions. PLoS ONE. 2011;6(11):e27317.
Cornforth DM, Dees JL, Ibberson CB, Huse HK, Mathiesen IH, Kirketerp-Møller K, et al. Pseudomonas aeruginosa transcriptome during human infection. Proc Natl Acad Sci. 2018;115(22):E5125–34.
• Chen X, Lorenzen J, Xu Y, Jonikaite M, Thaarup IC, Bjarnsholt T, et al. A novel chronic wound biofilm model sustaining coexistence of Pseudomonas aeruginosa and Staphylococcus aureus suitable for testing of antibiofilm effect of antimicrobial solutions and wound dressings. Wound Repair Regen. 2021;29(5):820–9. This study develops a novel, semi-solid biofilm substratum which mimics a wound bed. Biofilms grown on this new substrate respond similarly to anti-microbial dressings when compared to in vivo studies.
Schwarzer S, James GA, Goeres D, Bjarnsholt T, Vickery K, Percival SL, et al. The efficacy of topical agents used in wounds for managing chronic biofilm infections: a systematic review. J Infect. 2020;80(3):261–70.
Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464(7285):59–65.
Findley K, Oh J, Yang J, Conlan S, Deming C, Meyer JA, et al. Topographic diversity of fungal and bacterial communities in human skin. Nature. 2013;498(7454):367–70.
Kalan L, Grice EA. Fungi in the wound microbiome. Adv Wound Care (New Rochelle). 2018;7(7):247–55.
Kalan L, Loesche M, Hodkinson BP, Heilmann K, Ruthel G, Gardner SE, et al. Redefining the chronic-wound microbiome: fungal communities are prevalent, dynamic, and associated with delayed healing. mBio. 2016;7(5):e01058-16.
Pendleton KM, Huffnagle GB, Dickson RP. The significance of Candida in the human respiratory tract: our evolving understanding. Pathog Dis. 2017;75(3):ftx029.
Chellan G, Shivaprakash S, Ramaiyar SK, Varma AK, Varma N, Sukumaran MT, et al. Spectrum and prevalence of fungi infecting deep tissues of lower-limb wounds in patients with type 2 diabetes. J Clin Microbiol. 2010;48(6):2097–102.
Loesche M, Gardner SE, Kalan L, Horwinski J, Zheng Q, Hodkinson BP, et al. Temporal stability in chronic wound microbiota is associated with poor healing. J Invest Dermatol. 2017;137(1):237–44.
Delaney C, Kean R, Short B, Tumelty M, McLean W, Nile CJ, et al. Fungi at the scene of the crime: innocent bystanders or accomplices in oral infections? Curr Clin Microbiol Rep. 2018;5(3):190–200.
Fatahinia M, Poormohamadi F, Mahmoudabadi AZ. Comparative study of esterase and hemolytic activities in clinically important Candida species, isolated from oral cavity of diabetic and non-diabetic individuals. Jundishapur J Microbiol. 2015;8(3):e20893.
Dickson RP, Erb-Downward JR, Prescott HC, Martinez FJ, Curtis JL, Lama VN, et al. Analysis of culture-dependent versus culture-independent techniques for identification of bacteria in clinically obtained bronchoalveolar lavage fluid. J Clin Microbiol. 2014;52(10):3605–13.
Cuthbertson L, Rogers GB, Walker AW, Oliver A, Hoffman LR, Carroll MP, et al. Implications of multiple freeze-thawing on respiratory samples for culture-independent analyses. J Cyst Fibros. 2015;14(4):464–7.
Nilsson RH, Anslan S, Bahram M, Wurzbacher C, Baldrian P, Tedersoo L. Mycobiome diversity: high-throughput sequencing and identification of fungi. Nat Rev Microbiol. 2019;17(2):95–109.
Vesty A, Biswas K, Taylor MW, Gear K, Douglas RG. Evaluating the impact of DNA extraction method on the representation of human oral bacterial and fungal communities. PLoS ONE. 2017;12(1):e0169877.
Fredricks DN, Smith C, Meier A. Comparison of six DNA extraction methods for recovery of fungal DNA as assessed by quantitative PCR. J Clin Microbiol. 2005;43(10):5122–8.
Mac Aogáin M, Chaturvedi V, Chotirmall SH. MycopathologiaGENOMES: the new ‘home’ for the publication of fungal genomes. Mycopathol. 2019;184(5):551–4.
Tiew PY, Mac Aogain M, Ali N, Thng KX, Goh K, Lau KJX, et al. The mycobiome in health and disease: emerging concepts, methodologies and challenges. Mycopathol. 2020;185(2):207–31.
Peleg AY, Hogan DA, Mylonakis E. Medically important bacterial–fungal interactions. Nat Rev Microbiol. 2010;8(5):340–9.
Townsend EM, Sherry L, Kean R, Hansom D, Mackay WG, Williams C, et al. Implications of antimicrobial combinations in complex wound biofilms containing fungi. Antimicrob Agents Chemother. 2017;61(9):e00672.
• Brown JL, Townsend E, Short RD, Williams C, Woodall C, Nile CJ, et al. Assessing the inflammatory response to in vitro polymicrobial wound biofilms in a skin epidermis model. NPJ Biofilms Microbiomes. 2022;8(1):19. This study develops and characterises a complex, polymicrobial biofilm relevant to chronic wounds involving fungi and multiple bacterial species. This study also shows how anti-septics can influence the host response to the biofilm.
Durand B, Pouget C, Magnan C, Molle V, Lavigne JP, Dunyach-Remy C. Bacterial interactions in the context of chronic wound biofilm: a review. Microorganisms. 2022;10(8):1500.
Kong EF, Tsui C, Kucharíková S, Andes D, Dijck PV, Jabra-Rizk MA. Commensal protection of Staphylococcus aureus against antimicrobials by Candida albicans biofilm matrix. mBio. 2016;7(5):e01365-16.
Todd OA, Fidel PL Jr, Harro JM, Hilliard JJ, Tkaczyk C, Sellman BR, et al. Candida albicans Augments Staphylococcus aureus virulence by engaging the Staphylococcal agr Quorum Sensing System. mBio. 2019;10(3):e00910.
Vila T, Kong EF, Montelongo-Jauregui D, Van Dijck P, Shetty AC, McCracken C, et al. Therapeutic implications of C. albicans-S. aureus mixed biofilm in a murine subcutaneous catheter model of polymicrobial infection. Virulence. 2021;12(1):835–51.
Short B, Delaney C, McKloud E, Brown JL, Kean R, Litherland GJ, et al. Investigating the transcriptome of Candida albicans in a dual-species Staphylococcus aureus biofilm model. Front Cell Infect Microbiol. 2021;11:791523.
Yu XY, Fu F, Kong WN, Xuan QK, Wen DH, Chen XQ, et al. Streptococcus agalactiae inhibits Candida albicans hyphal development and diminishes host vaginal mucosal TH17 response. Front Microbiol. 2018;9:198.
Shing SR, Ramos AR, Patras KA, Riestra AM, McCabe S, Nizet V, et al. The fungal pathogen Candida albicans promotes bladder colonization of group B Streptococcus. Front Cell Infect Microbiol. 2020;9:437.
Pidwill GR, Rego S, Jenkinson HF, Lamont RJ, Nobbs AH. Coassociation between group B Streptococcus and Candida albicans promotes interactions with vaginal epithelium. Infect Immun. 2018;86(4):e00669.
Morgan SJ, Lippman SI, Bautista GE, Harrison JJ, Harding CL, Gallagher LA, et al. Bacterial fitness in chronic wounds appears to be mediated by the capacity for high-density growth, not virulence or biofilm functions. PLoS Pathog. 2019;15(3):e1007511.
Dhamgaye S, Qu Y, Peleg AY. Polymicrobial infections involving clinically relevant gram-negative bacteria and fungi. Cell Microbiol. 2016;18(12):1716–22.
Fourie R, Cason ED, Albertyn J, Pohl CH. Transcriptional response of Candida albicans to Pseudomonas aeruginosa in a polymicrobial biofilm. G3 Genes Genomes Genetics. 2021;11(4):jkab042.
Hogan DA, Kolter R. Pseudomonas-Candida interactions: an ecological role for virulence factors. Sci. 2002;296(5576):2229–32.
Bandara HMHN, Wood DLA, Vanwonterghem I, Hugenholtz P, Cheung BPK, Samaranayake LP. Fluconazole resistance in Candida albicans is induced by Pseudomonas aeruginosa quorum sensing. Sci Rep. 2020;10(1):7769.
Hamet M, Pavon A, Dalle F, Pechinot A, Prin S, Quenot J-P, et al. Candida spp. airway colonization could promote antibiotic-resistant bacteria selection in patients with suspected ventilator-associated pneumonia. Intensive Care Med. 2012;38(8):1272–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Pathogenesis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Short, B., Bakri, A., Baz, A. et al. There Is More to Wounds than Bacteria: Fungal Biofilms in Chronic Wounds. Curr Clin Micro Rpt 10, 9–16 (2023). https://doi.org/10.1007/s40588-022-00187-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40588-022-00187-x