Abstract
Purpose of review
In the recent years, more cases of poultry meat allergy, both IgE- or non-IgE-mediated, are being reported. Patients have varied clinical reactivity at various levels of sensitivity to different meat preparations. The lack of validated biomarkers renders accurate diagnosis challenging. In this review, we aim to provide an overview of the current status of poultry meat allergy along with a description on the allergens implicated.
Recent findings
Poultry meat allergy occurs as a result of cross-reactions with known allergens of egg yolk or bird feathers or as genuine IgE-mediated sensitivity to allergens in poultry meat. Individuals can also develop non-IgE-mediated hypersensitivity reactions to poultry meat. Chicken serum albumin is the main responsible allergen in secondary cases, while myosin light chain, α parvalbumin, enolase, aldolase, hemoglobin, and α-actin have been recognized as potential eliciting allergens in genuine poultry meat allergy.
Summary
There is a wide phenotypic variation among patients with poultry meat allergy, regarding clinical severity and cross-reactivity features. Recognizing the various clinical entities of reactions to poultry meat is an important step towards accurate diagnosis and providing management options that are well received by patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Poultry meat also known as lean meat or white meat is considered a healthier alternative to red meat. They are a major source of “high quality” protein, essential fatty acids, and micronutrients such as vitamin B3, B12, and selenium [1]. Food allergy (FA) to poultry meat occurs in both children and adults [2, 3•]. As an IgE-mediated FA, which may involve mild to severe symptoms, it can be a primary allergy to poultry or a secondary allergy in subjects previously allergic to eggs and/or bird feathers (“egg-bird/bird-egg syndrome”) or to fish (“fish-chicken syndrome”) (Fig. 1) [2]. Chicken meat allergy is the most studied poultry meat allergy. Non-IgE-mediated reactions to chicken meat include contact dermatitis, eosinophilic esophagitis (EoE). or food protein-induced enterocolitis (FPIES).
In this review, we aim to provide an overview of poultry meat allergy, shed light on the responsible allergens, and discuss the various clinical phenotypes associated with this condition.
Current state of poultry meat consumption
Poultry is a broad term for domestic fowls comprising mainly chickens, turkeys, ducks, and geese. Being a good source of easily digestible proteins, essential nutrients and having a low fat content, poultry, and chicken in particular is the most consumed meat globally. Poultry meat is often recommended as part of a balanced diet especially for growing children, pregnant, and breast feeding women, stages in life when protein requirement is in high demand [1].
Over the last 50 years, it is estimated that the average annual growth of industrial poultry farming was 5%; in contrast, it was only 3.1% and 1.5% for pork and beef, respectively. Today, the poultry meat consumption is yet reported to be > 15 kg per capita worldwide [4]. With the increasing global population and the current shift in trend from red to white meat consumption, the demand for poultry meat is projected to increase by 121% between the years 2005 and 2050 [5].
IgE-mediated poultry meat allergy: the primary type
Poultry meat was traditionally thought to be an uncommon cause of primary FA. Indeed, this food group does not appear in most of the targeted epidemiological studies involving large number of patients. However, allergies to poultry meat have been gaining recognition in the recent years with current estimates of 0.6–5% atopic individuals experiencing chicken meat intolerance [3•, 6].
Pathogenesis and clinical presentation
IgE-mediated primary poultry meat allergies are reported mostly in adolescents and young adults, mean age of 25 years, in contrast to other FA (milk, egg, peanut allergy), which occur more commonly in early childhood [2, 7]. For a few individuals, the onset of symptoms was during childhood [8, 9]. Among the cases reported, only a handful had a prior personal history of atopy in the form of FA to legumes, pork, and fish [10, 11•, 12, 13].
Clinically, primary allergies to poultry meat can vary from mild to severe symptoms. Most patients are referred for an oral allergy syndrome (OAS) and/or hives following ingestion of cooked chicken meat. However, severe anaphylaxis can occur [2, 14], especially after exercise [15]. Hemmer et al. reported cases of allergic reactions following contact with raw chicken meat as well [2]. An instance of severe hand edema and intense pruritus occurring post contact with a sponge that was used for cleaning the pot in which chicken was cooked was also noted by Liccardi et al. [16]. Inhalation of fumes or cooking vapors of chicken or turkey meat can also elicit severe respiratory symptoms [16, 17]. Allergic reactions to poultry meat classically occurs immediately or within half an hour following ingestion, contrary to red meat allergy (“α-Gal syndrome”) [18]. Table 1 depicts an overview on reported cases of primary poultry meat allergy.
Cross-reactivity chicken vs avian meats
Chicken meat is the main cause of genuine poultry meat allergy. However, many individuals experienced symptoms following turkey meat consumption as well [9, 20, 21]. Kelso et al. reported individuals presenting with OAS following intake of a variety of avian meat with skin prick test (SPT) positive for chicken, turkey, dove, and quail [14]. However, taking into consideration, some individuals with sensitivity to chicken meat tolerated turkey and other poultry meat [19], and as allergic reactions to other poultry meat are mostly mild and well tolerated [2, 10], a general recommendation of eliminating all other avian meat from the diet of individual is best taken based on an individual clinical evaluation.
Cross-reactivity chicken vs shrimp or fish
Hemmer et al. coined a new term “fish-shrimp-meat syndrome” describing individuals with concomitant genuine poultry meat as well as fish and shrimp allergy. In their observation, 30% of the subjects with poultry meat allergy self-reported concurrent fish allergy, while 63% and 42% had specific IgE (sIgE) levels > 0.35 kUA/l against cod and shrimp, respectively [2]. Kuehn et al. proposed the definition “fish-chicken syndrome” to characterize 29 patients with allergy to both poultry meat and fish [11•]. Both studies developed the notion that pronounced sIgE level might indicate the primary sensitizer.
Cross-reactivity chicken vs red meat
Red meat allergy to either pork or beef is rare. It is mostly reported in atopic individuals who are sensitized to bovine serum albumin present in beef, who also experience symptoms on ingestion of cow’s milk. Another syndrome, called “pork-cat syndrome,” occurs when patients are sensitized to inhalant allergen in cats such as Fed d 2 (cat serum albumin) and also develop allergic reaction on pork meat consumption due to the cross-reactivity with pork serum albumin [26]. In a study of 43 patients suffering from mammalian meat allergy, 50% of the subjects showed an IgE cross-reactivity to poultry meat [27]. Clinically relevant simultaneous allergies to both red meat and poultry is however highly uncommon. A case report published by Hilger et al. presented a woman with a personal history of pork allergy (on contact with raw pork, inhaling vapors of pork meat, and on consumption of cooked pork), who years later experienced allergic reactions following intake of cooked chicken leg. On further evaluation, it was shown that the patient had developed sIgE to both chicken and porcine hemoglobin α-chain (homology of ~ 57%) and porcine and chicken serum albumin (homology of ~ 45%) [10]. Hemmer et al. also observed that 7% of their patients with chicken meat allergy had concurrent cross-reactivity to red meat as well. Nonetheless, serum albumin was not the common eliciting allergen in their patients. A possible common allergen could be α-parvalbumin, which shows a high sequence identity between mammal and poultry meat [2].
Cross-reactivity chicken vs crocodile meat
Ballardini et al. reported a case of severe crocodile meat allergy in a 13-year-old boy who had a known history of poultry meat allergy (chicken and turkey) since he was 5 years of age. sIgE were positive to both chicken and crocodile meat extract, as well as α-parvalbumin. Chicken and crocodile α-parvalbumin were 90% homologous, which the cross-reactivity between both foods [24].
IgE-mediated poultry meat allergy: the secondary type bird-egg syndrome
The first case of bird-egg syndrome was published in 1985 by de Maat-Bleeker et al. describing a 65-year-old female, who developed urticaria and angioedema following ingestion of hen’s egg yolk. Symptoms started in adult life and coincided with the acquisition of a pet parrot [28]. Since then, allergy to poultry meat, either self-reported or as a positive SPT to poultry meat extracts has been reported in patients with this syndrome [29, 30].
Pathogenesis and clinical presentation
Individuals are primarily sensitized to avian aeroallergens (feathers, dander, and bird droppings). They then develop cross-reactive allergic symptoms to egg yolk proteins, usually later in adulthood [31]. A few cases have been reported in children as well [32]. Patients react to either undercooked, soft boiled, or raw eggs, but not to fully cook hard boiled eggs. Most cases of bird-egg syndrome show positivity to chicken or other poultry meat extract on SPT or by in vitro assays [33, 34]. However, most individuals are able to tolerate poultry meat. This is attributed to the fact that the responsible allergen for this condition is a heat labile protein, namely, serum albumin [2, 35]. Serum albumins are high molecular weight (~ 70 kDa), highly cross-reactive, multi-functional proteins abundantly found in egg yolk (referred to as chicken serum albumin or α-livetin or Gal d 5), animal dander, bird feathers, and muscle tissue. These proteins have an amino acid sequence very similar to human serum albumin, and yet peculiarly, they can sensitize atopic individuals and incite an allergic reaction [35]. As poultry meat like chicken is mostly consumed well cooked, patients with bird-egg syndrome rarely experience significant clinical symptoms following intake of poultry meat. Actual prevalence data on poultry meat allergy in patients with bird-egg syndrome is not available, but poultry meat intolerance have been reported in 3/8 (37%) adults presenting with allergic respiratory symptoms to feathers and in 22% of children with dual egg and bird allergy [36, 37].
Bird-egg syndrome is frequently involved in occupational cutaneous and respiratory allergies. Individuals with a history of atopic dermatitis who are routinely exposed to raw poultry by cutaneous or respiratory route (cooks, butchers, food industry) may develop contact dermatitis to poultry meat [38]. Cases of contact urticaria when handling raw avian meat were also reported in 4/8 adult patients allergic to bird feathers by Quirce et al. [33]. In a group of 57 women working in poultry food industry, 49, 43.9, 38.6, and 5.3% were suffering from chronic cough, dyspnea, rhinitis, and occupational asthma, respectively. Allergic work-up showed a positive IgE and SPT to avian meat in 36.8% of the employees [39]. Hypersensitivity pneumonitis, especially through meat and feather exposure in slaughterhouses, should be thought of [40]. Serum albumin and other avian antigens have been proposed in such non-IgE-mediated manifestations.
Egg-bird syndrome
Allergies to egg proteins are regarded as the most common FA during childhood. Globally, current data estimates that 0.5–2.5% of children suffer from egg allergy, most commonly during the first year of their lives [7, 41]. Patients with hen’s egg allergy often have cross-reactive allergic reactions to other poultry eggs such as duck, turkey, geese, or quail’s egg. However, cross-reactivity to chicken and other avian meat is relatively rare [42]. Cheikh et al. reported a case of anaphylaxis following chicken meat consumption in a 13-year-old patient who had a personal history of egg allergy. The child continued developing severe allergic symptoms after ingesting undercooked grilled chicken meat, on contact with bird feathers, and even following inhalation of aeroallergens while in the vicinity of a poultry pen. She however did not experience any reactions when she accidentally consumes fully cooked chicken meat. SPT were positive for extracts of chicken meat, chicken feather and egg [43].
Pathogenesis
Contrary to poultry meat allergy in bird-egg syndrome that is mostly observed in adults, poultry meat allergy in egg-bird syndrome seems to be common in children [43, 44]. Primary sensitization to egg proteins occurs via the gastrointestinal mucosa following ingestion which then cross-reacts with proteins present in poultry meat. The heat labile chicken serum albumin has been implicated as the causative allergen in this syndrome as well, which explains why patients tolerated cooked chicken meat.
Allergens in IgE-mediated poultry meat allergy
Myosin light chain 1
An IgE reactivity to myosin light chain 1 (MLC 1) was first described by González-Mancebo et al., in a 20-year-old woman referred for an allergy to chicken. She was also sensitized to α-parvalbumin [23]. Klug et al. further confirmed MLC, which was then named as Gal d 7, as the primary allergen in primary poultry meat allergy [3•]. This was also corroborated by Hemmer et al. in a series of 21 Austrian and Spanish patients with genuine poultry meat allergy [2]. MLC are low molecular weight (16–24 kDa) muscle protein belonging to the calmodulin gene family. Along with myosin heavy chain, they constitute the myosin protein complex [3•]. MLC exists in various isoforms, with MLC 1 or Gal d 7 ~ 23 kDa being the major allergen and MLC 3 (~ 13–18 kDa) a truncated isoform as a minor allergen in chicken meat [2]. Functionally, myosin are mostly responsible for motor functions by interacting with actin filaments. MLC have been shown to be able withstand acids and alkalis, thus retaining its allergenicity after digestion [45]. They are markedly heat stable protein as well that can resists denaturation even when exposed to high temperatures, thus explaining why patients with primary poultry meat allergy experience allergic reactions to both raw and cooked poultry meat [2, 45]. Chicken MLC 1 protein shows a strong degree of homology with MLC 1 from other poultry such as turkey, duck, and goose; hence, individuals primarily sensitized to chicken meat can develop cross-reactive allergic reactions to other poultry meat as well [2]. MLC have also been identified as a novel minor allergen responsible for shrimp and crayfish allergies as well [45, 46]. Since homology between chicken and fish MLC is high (63–65%), cross-reactive allergic reactions between chicken and fish are a possibility. Based on immunoblot inhibition experiments, Hemmer et al. were able to demonstrate that MLC-dependent cross-reactions between fish and chicken meat may occur [2].
Parvalbumin
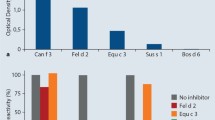
A first isolated case of a 23-year-old woman presenting with asthma after chicken consumption, with IgE reactivity to parvalbumin, was published by González-de-Olano et al. [12]. Kuehn et al. validated the involvement of α-parvalbumin in a series of patients with primary allergy to poultry meat [21]. Subsequently, α-parvalbumin has been concluded to be the “culprit” allergen in many other cases of allergy to poultry meat and as the main responsible allergen in individuals with “Fish-chicken syndrome” or “Fish-shrimp-meat syndrome” [11•, 12, 23]. Parvalbumin, an acidic muscle protein, is the major allergen involved in fish allergies [47]. It is a low molecular weight protein (10–12 kDa) abundantly found in fast contracting muscles and to a small extent in the endocrine and central nervous system as well [12]. Parvalbumin belong to the family of calcium-binding “EF hand proteins” [7, 12]. Functionally, they are responsible for regulating the intracellular calcium ion concentration during muscle relaxation. They are highly stable molecules that are able to resists chemical, thermal, and proteolytic conditions [48]. Kuehn et al. demonstrated that parvalbumin could be detected in various chicken meat samples irrespective of their processing methods, thus explaining the reactivity of patients to processed meat [11•]. The authors also observed that parvalbumin was detectable mainly in chicken leg and wing (raw or cooked) rather than in breast tissue [11•]. Parvalbumin exists in two evolutionary lineage, notably, α- and β-parvalbumin. While α-parvalbumin was believed to be weakly allergenic, β-parvalbumin is recognized as the main culprit allergen in fish allergies. Nonetheless, the α-lineage is being identified as a one of the major allergens in poultry meat allergies in recent literatures [11•, 12, 48]. In a study by Kuehn et al. of 29 patients with allergies to both chicken and fish, 69% and had a positive sIgE to chicken α-parvalbumin. This novel chicken allergen was then named Gal d 8 [11•]. Alpha and beta-parvalbumin share a high degree of homology (~ 66%) with ~ 51% sequence identity. Clinically relevant cross-reactivity between fish and avian parvalbumin can occur [11•, 24]. The prevalence of such cross-sensitivity still needs to be determined by larger studies.
Enolases and aldolases
These are glycolytic enzymes belonging to the “TIM barrel” protein family. Functionally they play an important role in cellular metabolic processes such as glycolysis. These enzymes are well known minor fish allergens [47]. However, they are now also recognized as chicken allergens. Kuehn et al. identified IgE positivity of 72% and 83% to chicken enolase and aldolase, respectively, in patients allergic to chicken and fish. Among 7 patients with isolated chicken meat allergy, 6/7 were positive to enolase and aldolase. These allergens were recorded as Gal d 9 and Gal d 10 for chicken enolase and aldolase, respectively [11•]. Contrary to parvalbumin, enolase and aldolase are less resistant to processing methods such as heating. Nonetheless, it was reported these enzymes were still detectable in cooked chicken breast samples [11•].
Hemoglobin
After analyzing the case of a woman with a history of occupational allergy to pork who later developed symptoms after ingesting chicken, Hilger et al. identified proteins with molecular weights of 12 and 14 kDa as possible allergens. These proteins were discovered to represent α- and β-chain of chicken hemoglobin, respectively [10]. Hemoglobin is an iron-binding globulin protein, which principally serves as an oxygen carrier in the blood [49]. Animal hemoglobin has not been recognized as an allergen for humans previously. On the other hand, hemoglobin of the invertebrate Chironomus thummi (commonly known as blood worms) has been described as an allergen in humans. González-Fernández et al. also named hemoglobin as a major allergen of Anisakis simplex (Ani s 13) [50]. Human and chicken hemoglobin chain shares a very high amino acid sequence identity (70%). Nonetheless, under certain exposure conditions, vertebrate hemoglobin can generate sIgE regardless of their high sequence homology to human hemoglobin [10].
Other allergens
Barbarroja-Escudero et al. studied the serum of a woman referred for recurrent anaphylaxis to fish and who subsequently developed anaphylaxis to chicken and turkey. The authors discovered cross-reactive allergens of 33 and 42 kDa; the latter was identified as α-actin [25]. This allergen was previously reported in a case of allergy to Nile perch [51].
What studies in dogs tell us?
Chicken is the third most common food allergen in dogs (15% of FA) and cats (5% of FA) [52]. Olivry et al. have recently identified allergens already described in humans, Gal d 5, enolase and glyceraldehyde-3-phosphate, beyond pyruvate kinase, creatine kinase, lactate dehydrogenase, and triosephosphate isomerase as the major allergens in dogs allergic to chicken meat. Troponin C2 was considered a minor allergen [53].
Diagnosis of IgE-mediated poultry meat allergy
The diagnosis is commonly based on the history, clinical examination, skin, and/or sIgE testing.
Skin testing
Prick testing with commercial meat extract is no longer available in many countries, and extracts can be of poor quality depending on how they were produced [50]. Nowadays, clinicians most often perform prick-to-prick tests with raw or cooked poultry meat, a technique validated by some scientific societies [54]. Several studies have also shown that prick-to-prick is sometimes more sensitive than prick-testing with commercial allergenic extracts, especially if the native material is the authentic, symptom-triggering food [55].
Component resolved diagnosis (CRD)
Quantification of sIgE is currently only available for the recombinant Gal d 5. For allergens implicated in primary poultry meat, IgE quantification is not available yet on the existing multiplex systems such as Thermo Fischer ImmunoCAP-ISAC, FABER or MADx ALEX2.
Challenges with diagnosis of poultry meat allergy
Characterization of patients into clinical phenotypes largely depends on medical history and clinical examination. Primary vs secondary poultry meat allergy might be diagnosed based on the presence or absence of sIgE to chicken serum albumin, egg white proteins, and bird feathers [3•]. The gold standard for diagnosing FA is oral food challenge (OFC), which is cost- and resource-demanding. OFC-based studies on chicken meat allergy are rare given those limitations. To date, there are no specific recommendations for carrying out provocation tests on meat, particularly concerning the method of cooking and the dose to be administered. The EAACI and AAAI recommendations for the standardization of OFC (PRACTALL) propose administering gradual incremental doses starting with 3 mg up to 3 g of protein [56]. However, these general OFC dose recommendations may not be applicable to poultry meat allergy as the average serving dose for a 2-year-old child and an adult is 20 and 100 g of chicken, which equivalents to 5.4 and 27 g of protein, respectively. To rule out the diagnosis of chicken allergy, it is therefore recommended to administer a total cumulative dose reaching the serving-dose adapted to the patient’s age.
IgE-mediated poultry meat allergy: what else?
Management and prognosis
A majority of allergic reactions to poultry meat were mild to moderate cases of OAS, urticaria, or systemic gastrointestinal upset such as nausea or vomiting. Avoiding the culprit meat was the mainstay management for these individuals. A few cases of severe allergic reactions needing emergency medical management have been reported [16, 17]. Barnig et al. reported a case of recurrent severe anaphylactic reactions on exposure to vapors of roast chicken. The patient was successfully treated with omalizumab [17]. Natural history of poultry allergy has not been studied due to the limited number of cases. Egg-bird syndrome occurs during early childhood and usually resolves before adolescence. Natural evolution of egg-bird syndromes differs according to the persistence of exposure to avian aeroallergens.
Future prospects
While avoidance strategy is the primary step when addressing FA, accidental exposure resulting in severe near fatal reactions is known to occur [16]. Food allergen immunotherapy has emerged as a promising therapeutic modality for patients with FA [57]. Interestingly, recovery from a chicken meat allergy has been described in an adult with bird-egg syndrome after oral desensitization with egg [58].
Non-IgE mediated allergy to poultry
Poultry protein-induced enterocolitis syndrome
FPIES is essentially characterized by the occurrence of vomiting, 1 to 4 h after ingestion of the suspect food, sometimes accompanied by delayed onset diarrhea and classically not associated with hives or wheezing [59]. It is mostly seen in young infants and children who would often require hospitalization for dehydration or shock [60••]. The current estimated incidence of FPIES in birth cohorts is 0.14–0.7% [59]. Cow’s milk, rice, oats, fish, soy, and eggs are the major food involved in FPIES. Two cases of severe acute enteropathy related to chicken ingestion were first published in 1982 by Vitoria et al. After an oral challenge with chicken meat in one case, the patient developed protracted vomiting, bloody diarrhea, and followed by shock with a jejunal biopsy showing villous atrophy [61]. Since then, multiple cases of FPIES associated with poultry meat consumption have been reported. The Australian Paediatric Surveillance Unit (APSU) process reported 230 FPIES between 2012 and 2014, and chicken was involved in 19 children (8%) [62]. In a retrospective study by Xepapadaki et al., among the 15,114 Greek children referred for suspected allergies, 72 were diagnosed with acute FPIES (prevalence 0.47%), and chicken was involved in 2.8% of these cases [63]. Over a 10-year period, 160 FPIES were diagnosed at a US center, 3 of which were attributed to chicken ingestion (1.9%) [64]. In a recent French series involving 179 patients where 10 patients had multiple FA, chicken was incriminated in 2/179 patients (1.1%) [65]. Poultry FPIES seem to resolve spontaneously, well before the resolution of fish allergy. Rare acute FIEPS to chicken with cross-allergy to various avian meats may develop in adulthood (2 unpublished cases observed by the authors).
The underlying pathogenesis of this condition is not clearly understood yet, but it is believed to be a non-IgE-mediated reaction to food proteins. Apart from the occasional cases of FPIES associated with IgE-mediated sensitization, skin tests, measurement of specific antibodies, and cell activation tests with the suspected food allergen are mostly inconclusive [66, 67]. Considering the lack of validated biomarkers, the diagnosis of FPIES currently relies on fulfilling a set of diagnostic clinical criteria [66]. FPIES is therefore a source of medical dilemma often resulting in diagnostic delays.
Eosinophilic esophagitis and poultry meat
Eosinophilic esophagitis (EoE) is now considered a common cause of esophageal disease. Cases of EoE have rapidly increased in the last 20 years, affecting all ages with a prevalence of around 0.4% in European countries [68]. A case of EoE associated with a proven poultry meat allergy was first published in 2006 [69]. In a recent meta-analysis, Zhan et al. identified recommended diets for EoE. Chicken avoidance was advised in approximately 10% of patients [70]. However, the culpability of poultry appeared to vary among teams, and poultry avoidance was mostly suggested for children in the USA. In a series of 941 cases of EoE in US children, an allergy to chicken meat accounted for 5% of EoE [71]. Cases of bird-egg syndrome with EoE on consuming chicken meat were reported in two Spanish women aged 55 and 39 years, respectively. Both patients were allergic to chicken meat and also suffered from asthma when occupationally exposed to birds [72, 73]. The patient reported by Garcia Rodriguez et al. was persistently allergic to both egg white and yolk proteins since childhood. She received oral immunotherapy (OIT) for egg yolk and egg white. Three years after starting OIT (and several anaphylactic reactions after egg ingestion), she was partially tolerant to egg but developed EoE that regressed with high doses of omeprazole and an egg-free diet [72]. In their series of patients with primary poultry meat allergy, Klug et al. observed one patient with fish-chicken syndrome who also presented with symptoms of EoE following poultry meat consumption [3•].
Conclusion
Poultry meat allergy is relatively rare. However, the burden of this allergy may be underestimated. Chicken is the most commonly implicated culprit, which probably reflects food consumption habits. It may be a primary allergy or a cross-allergy to birds and egg (as in bird-egg syndrome) or a cross-allergy to fish as well. The clinical presentation of poultry allergy is multifaceted, and the digestive manifestations should not be neglected. Although the last ten years have seen great progress in the characterization of poultry meat allergens, no work on immunotherapy has been published yet and to date; therapeutic management remains limited to avoidance diet and emergency kits prescriptions.
Change history
10 July 2022
The original version of this paper was updated to correct the layout of body texts.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Marangoni F, Corsello G, Cricelli C, Ferrara N, Ghiselli A, Lucchin L, et al. Role of poultry meat in a balanced diet aimed at maintaining health and wellbeing: an Italian consensus document. Food Nutr Res. 2015;59:27606.
Hemmer WKC, Swoboda I. Update on the bird-egg syndrome and genuine poultry meat allergy. Allergo J Int. 2016;25:68–75.
• Klug C, Hemmer W, Roman-Carrasco P, Focke-Tejkl M, Quirce S, Boyano-Martinez T, et al. Gal d 7-a major allergen in primary chicken meat allergy. J Allergy Clin Immunol. 2020;146(1):169–79 e5. The authors identified a novel protein as a major allergen for poultry meat allergy.
OECD, Food, Nations AOotU. OECD-FAO Agricultural Outlook 2021–20302021.
Mottet A, Tempio G. Global poultry production: current state and future outlook and challenges. World’s Poult Sci J. 2019;73(2):245–56.
Besler MRP. Chicken meat (Gallus domesticus). Intern Symp Food Allergens. 2001;3(4):193–201.
Matricardi PM, Kleine-Tebbe J, Hoffmann HJ, Valenta R, Hilger C, Hofmaier S, et al. EAACI molecular allergology user’s guide. Pediatr Allergy Immunol. 2016;27(Suppl 23):1–250.
Can CYM, Ciplak G. Chicken meat anaphylaxis in a child with no allergies to eggs or feathers. Iran J Pediatr. 2014;24:786–7.
Cahen YDFR, Wüthrich B. Food allergy with monovalent sensitivity to poultry meat. Clin Exp Allergy. 1998;28(8):1026–30.
Hilger C, Swiontek K, Hentges F, Donnay C, de Blay F, Pauli G. Occupational inhalant allergy to pork followed by food allergy to pork and chicken: sensitization to hemoglobin and serum albumin. Int Arch Allergy Immunol. 2010;151(2):173–8.
Kuehn A, Codreanu-Morel F, Lehners-Weber C, Doyen V, Gomez-Andre SA, Bienvenu F, et al. Cross-reactivity to fish and chicken meat - a new clinical syndrome. Allergy. 2016;71(12):1772-81. A new clincal syndrome was described along with the identification of the responsible allergens for such a condition
González-de-Olano DBB, Maroto AS, Vivanco F, Pastor-Vargas C. Asthma after chicken consumption due to cross-reactivity between fish and chicken parvalbumin. J Investig Allergol Clin Immunol. 2012;22:227–8.
Sokolova A, Célia Costa A, Conceição Santos M, Bartolomé B, Pereira BM. Severe allergy to poultry meat without sensitisation to egg proteins with concomitant Leguminosae allergy. Case report. Allergol Immunopathol. 2009;37(3):168–71.
Kelso JMCG, Helm RM, Burks AW. Common allergens in avian meat. J Allergy Clin Immunol. 1999;104:202–4.
Kajita N, Morikawa E, Yoshida K, Kinoshita K, Narita M. A rare case of food-dependent exercise-induced anaphylaxis triggered by chicken meat. Pediatr Int. 2022;64(1): e15100.
Liccardi GSZ, Noschese P, Nentwich I, Amato DM, D’Amato G. Allergy to chicken meat without sensitization to egg proteins: a case report. J Allergy Clin Immunol. 1997;100(4):577–9.
Barnig CHC, Muti D, Blaumeiser M, Purohit A, Hentges F, De Blay F. Anaphylaxis to vapors of roasting chicken controlled by omalizumab. J Investig Allergol Clin Immunol. 2012;22(6):439–40.
Apostolovic D, Tran TA, Starkhammar M, Sanchez-Vidaurre S, Hamsten C, Van Hage M. The red meat allergy syndrome in Sweden. Allergo J Int. 2016;25(2):49–54.
Vila LBE, Sanz ML. Chicken meat induces oral allergy syndrome: a case report. Ann Allergy Asthma Immunol. 1998;80:195–6.
Zacharisen MC. Severe allergy to chicken meat. WMJ. 2006;105(5):50–2.
Kuehn A, Lehners C, Hilger C, Hentges F. Food allergy to chicken meat with IgE reactivity to muscle alpha-parvalbumin. Allergy. 2009;64(10):1557–8.
Theler B, Brockow K, Ballmer-Weber BK. Clinical presentation and diagnosis of meat allergy in Switzerland and Southern Germany. Swiss Med Wkly. 2009 May 2;139(17–18):264–70.
González-Mancebo EPC, González-de-Olano D, Gandolfo-Cano M, Melendez A, Cuesta J, Zapatero A, Bartolomé B. Identification of allergens in chicken meat allergy. J Investig Allergol Clin Immunol. 2011;21(4):326–7.
Ballardini N NA, Hamsten C, Vetander M, Melén E, Nilsson C, Ollert M, Flohr C, Kuehn A, van Hage M. Anaphylactic reactions to novel foods: case report of a child with severe crocodile meat allergy. Pediatrics. 2017;139(4).
Barbarroja-Escudero J, Sánchez-González MJ, Bartolomé B, Pastor-Vargas C, Rodríguez-Rodríguez M, Cuesta-Herranz J, et al. Actin as a possible cross-reactive allergen between fish and poultry. J Investig Allergol Clin Immunol. 2019;29(2):152–4.
Wilson JM, Platts-Mills TAE. Red meat allergy in children and adults. Curr Opin Allergy Clin Immunol. 2019;19(3):229–35.
Ayuso RLS, Tanaka L, Ibañez MD, Pascual C, Burks AW, Sussman GL, Goldberg B, Lopez M, Reese G. IgE antibody response to vertebrate meat proteins including tropomyosin. Ann Allergy Asthma Immunol. 1999;83(5):399–405.
de Maat-Bleeker F, van Dijk AG, Berrens L. Allergy to egg yolk possibly induced by sensitization to bird serum antigens. Ann Allergy. 1985;54(3):245–8.
Hoffman DR, Guenther DM. Occupational allergy to avian proteins presenting as allergy to ingestion of egg yolk. J Allergy Clin Immunol. 1988;81(2):484–8.
Besler MFA, Restani P. Allergen data collection: chicken meat (Gallus domesticus). Internet Symp Food Allergens. 2001;3(4):193–201.
Dona DW, Suphioglu C. Egg allergy: diagnosis and immunotherapy. Int J Mol Sci. 2020;21(14).
Añíbarro B, García-Ara C, Ojeda JA. Bird-egg syndrome in childhood. J Allergy Clin Immunol. 1993;92(4):628–30.
Quirce S, Marañón F, Umpiérrez A, de las Heras M, Fernández-Caldas E, Sastre J. Chicken serum albumin (Gal d 5*) is a partially heat-labile inhalant and food allergen implicated in the bird-egg syndrome. Allergy. 2001;56(8):754–62.
Szépfalusi Z, Ebner C, Pandjaitan R, Orlicek F, Scheiner O, Boltz-Nitulescu G, et al. Egg yolk alpha-livetin (chicken serum albumin) is a cross-reactive allergen in the bird-egg syndrome. J Allergy Clin Immunol. 1994;93(5):932–42.
Chruszcz M, Mikolajczak K, Mank N, Majorek KA, Porebski PJ, Minor W. Serum albumins-unusual allergens. Biochim Biophys Acta. 2013;1830(12):5375–81.
Bausela BA, García-Ara MC, Martín Esteban M, Boyanó Martínez TB, Diaz Pena JM, Ojeda Casas JA. Peculiarities of egg allergy in children with bird protein sensitization. Ann Allergy Asthma Immunol. 1997;78(2):213–6.
AñibarroBausela B, Martín Esteban M, Martínez Alzamora F, Pascual Marcos C, Ojeda Casas JA. Egg protein sensitization in patients with bird feather allergy. Allergy. 1991;46(8):614–8.
Berbegal L, DeLeon FJ, González I, Silvestre JF. Protein contact dermatitis caused by chicken meat in bird-egg syndrome. Contact Dermatitis. 2017;77(4):253–4.
Zuskin E, Kanceljak B, Mustajbegovic J, Schachter EN, Stilinovic L. Respiratory symptoms and immunological status in poultry food processing workers. Int Arch Occup Environ Health. 1994;66(5):339–42.
Rouzet A, Valot B, Reboux G, Millon L, Roussel S. Common proteins located in pigeon, budgerigar, and hen droppings related to bird fancier’s lung. J Investig Allergol Clin Immunol. 2018;28(3):182–4.
Rona RJ, Keil T, Summers C, Gislason D, Zuidmeer L, Sodergren E, et al. The prevalence of food allergy: a meta-analysis. J Allergy Clin Immunol. 2007;120(3):638–46.
Tan JW, Joshi P. Egg allergy: an update. J Paediatr Child Health. 2014;50(1):11–5.
CheikhRouhou S, Bachouch I, Racil H, Chaouch N, Zarrouk M, Salmi L, et al. Anaphylaxis due to chicken meat. Rev Mal Respir. 2012;29(1):98–100.
Martínez Alonso JC, Domínguez Ortega FJ, Fuentes Gonzalo MJ. Angioedema due to sensitization to chicken meat. Allergol Immunopathol (Madr). 2003;31(1):50–2.
Zhang YX, Chen HL, Maleki SJ, Cao MJ, Zhang LJ, Su WJ, et al. Purification, characterization, and analysis of the allergenic properties of myosin light chain in Procambarus clarkii. J Agric Food Chem. 2015;63(27):6271–82.
Ayuso R, Grishina G, Bardina L, Carrillo T, Blanco C, Ibáñez MD, et al. Myosin light chain is a novel shrimp allergen, Lit v 3. J Allergy Clin Immunol. 2008;122(4):795–802.
Klueber J, Schrama D, Rodrigues P, Dickel H, Kuehn A. Fish allergy management: from component-resolved diagnosis to unmet diagnostic needs. Curr Treat Opt Allergy. 2019;6(4):322–37.
Kuehn A, Swoboda I, Arumugam K, Hilger C, Hentges F. Fish allergens at a glance: variable allergenicity of parvalbumins, the major fish allergens. Front Immunol. 2014;5:179.
Huehns ER, Shooter EM. Human Haemoglobins. J Med Genet. 1965;2(1):48–90.
González-Fernández J, Daschner A, Nieuwenhuizen NE, Lopata AL, Frutos CD, Valls A, et al. Haemoglobin, a new major allergen of Anisakis simplex. Int J Parasitol. 2015;45(6):399–407.
Tomm JM, van Do T, Jende C, Simon JC, Treudler R, von Bergen M, et al. Identification of new potential allergens from Nile perch (Lates niloticus) and cod (Gadus morhua). J Investig Allergol Clin Immunol. 2013;23(3):159–67.
Mueller RS, Olivry T, Prélaud P. Critically appraised topic on adverse food reactions of companion animals (2): common food allergen sources in dogs and cats. BMC Vet Res. 2016;12:9.
Olivry T, Pucheu-Haston CM, Mayer U, Bergvall K, Bexley J. Identification of major and minor chicken allergens in dogs. Vet Dermatol. 2022;33(1):46-e16.
Worm M, Reese I, Ballmer-Weber B, Beyer K, Bischoff SC, Classen M, et al. Guidelines on the management of IgE-mediated food allergies: S2k-Guidelines of the German Society for Allergology and Clinical Immunology (DGAKI) in collaboration with the German Medical Association of Allergologists (AeDA), the German Professional Association of Pediatricians (BVKJ), the German Allergy and Asthma Association (DAAB), German Dermatological Society (DDG), the German Society for Nutrition (DGE), the German Society for Gastroenterology, Digestive and Metabolic Diseases (DGVS), the German Society for Oto-Rhino-Laryngology, Head and Neck Surgery, the German Society for Pediatric and Adolescent Medicine (DGKJ), the German Society for Pediatric Allergology and Environmental Medicine (GPA), the German Society for Pneumology (DGP), the German Society for Pediatric Gastroenterology and Nutrition (GPGE), German Contact Allergy Group (DKG), the Austrian Society for Allergology and Immunology (Æ-GAI), German Professional Association of Nutritional Sciences (VDOE) and the Association of the Scientific Medical Societies Germany (AWMF). Allergo J Int. 2015;24:256–93.
Levin C, Warshaw E. Protein contact dermatitis: allergens, pathogenesis, and management. Dermatitis. 2008;19(5):241–51.
Sampson HA, Gerth van Wijk R, Bindslev-Jensen C, Sicherer S, Teuber SS, Burks AW, et al. Standardizing double-blind, placebo-controlled oral food challenges: American Academy of Allergy, Asthma & Immunology-European Academy of Allergy and Clinical Immunology PRACTALL consensus report. J Allergy Clin Immunol. 2012;130(6):1260–74.
Schoos AM, Bullens D, Chawes BL, Costa J, De Vlieger L, DunnGalvin A, et al. Immunological outcomes of allergen-specific immunotherapy in food allergy. Front Immunol. 2020;11: 568598.
Rial MJ, Valverde-Monge M, Gómez-Cardeñosa A, Vera-Berríos R, Pastor-Vargas C, Cuesta-Herranz J. Desensitization to cross-reacting allergen in egg yolk and chicken meat. J Allergy Clin Immunol Pract. 2019;7(2):696–7.
Cianferoni A. Food protein-induced enterocolitis syndrome epidemiology. Ann Allergy Asthma Immunol. 2021;126(5):469–77.
Agyemang A, Nowak-Wegrzyn A. Food protein-induced enterocolitis syndrome: a comprehensive review. Clin Rev Allergy Immunol. 2019;57(2):261–71. Authors provided a comprehensive overview of a non-IgE-mediated reaction to food including to poultry meat.
Vitoria JC, Camarero C, Sojo A, Ruiz A, Rodriguez-Soriano J. Enteropathy related to fish, rice, and chicken. Arch Dis Child. 1982;57(1):44–8.
Mehr S, Frith K, Barnes EH, Campbell DE. Food protein-induced enterocolitis syndrome in Australia: a population-based study, 2012–2014. J Allergy Clin Immunol. 2017;140(5):1323–30.
Xepapadaki P, Kitsioulis NA, Manousakis E, Manolaraki I, Douladiris N, Papadopoulos NG. Remission patterns of food protein-induced enterocolitis syndrome in a Greek pediatric population. Int Arch Allergy Immunol. 2019;180(2):113–9.
Caubet JC, Ford LS, Sickles L, Järvinen KM, Sicherer SH, Sampson HA, et al. Clinical features and resolution of food protein-induced enterocolitis syndrome: 10-year experience. J Allergy Clin Immunol. 2014;134(2):382–9.
Lemoine A, Colas AS, Le S, Delacourt C, Tounian P, Lezmi G. Food protein-induced enterocolitis syndrome: a large French multicentric experience. Clin Transl Allergy. 2022;12(2): e12112.
Nowak-Węgrzyn A, Chehade M, Groetch ME, Spergel JM, Wood RA, Allen K, et al. International consensus guidelines for the diagnosis and management of food protein-induced enterocolitis syndrome: executive summary-Workgroup Report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. J Allergy Clin Immunol. 2017;139(4):1111-26.e4.
Barni S, Vazquez-Ortiz M, Giovannini M, Liccioli G, Sarti L, Cianferoni A, et al. Diagnosing food protein-induced enterocolitis syndrome. Clin Exp Allergy. 2021;51(1):14–28.
Arias Á, Lucendo AJ. Prevalence of eosinophilic oesophagitis in adult patients in a central region of Spain. Eur J Gastroenterol Hepatol. 2013;25(2):208–12.
Martín-Muñoz MF, Lucendo AJ, Navarro M, Letrán A, Martín-Chávarri S, Burgos E, et al. Food allergies and eosinophilic esophagitis–two case studies. Digestion. 2006;74(1):49–54.
Zhan T, Ali A, Choi JG, Lee M, Leung J, Dellon ES, et al. Model to determine the optimal dietary elimination strategy for treatment of eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2018;16(11):1730-7.e2.
Spergel JM, Brown-Whitehorn TF, Cianferoni A, Shuker M, Wang ML, Verma R, et al. Identification of causative foods in children with eosinophilic esophagitis treated with an elimination diet. J Allergy Clin Immunol. 2012;130(2):461-7.e5.
García Rodríguez R, Méndez Díaz Y, Moreno Lozano L, Extremera Ortega A, Gómez TE. Eosinophilic esophagitis after egg oral immunotherapy in an adult with egg-allergy and egg-bird syndrome. J Investig Allergol Clin Immunol. 2017;27(4):266–7.
Gomez Torrijos E, García Rodriguez C, Rodriguez J, De la Roca F, Cárdenas R, Alfaya F, et al. Occupational asthma and eosinophilic esophagitis in a patient with egg-bird syndrome. J Investig Allergol Clin Immunol. 2015;25(1):61–2.
Funding
This work was supported by the Ministry of Research, Luxembourg, and the PRIDE program grant (PRIDE i2TRON PRIDE19/14254520) by Fonds National de la Recherche (FNR), Luxembourg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Naphisabet Wanniang declares that she has no conflict of interest. Françoise Codreanu-Morel declares that she has no conflict of interest. Annette Kuehn declares that she has no conflict of interest. Martine Morisset declares that she has no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human participants or animal performed by any of the authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Annette Kuehn and Martine Morisset contribute equally and share the senior co-authorship of this review.
This article is part of the Topical Collection on Food Allergy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wanniang, N., Codreanu-Morel, F., Kuehn, A. et al. Poultry Meat allergy: a Review of Allergens and Clinical Phenotypes. Curr Treat Options Allergy 9, 187–203 (2022). https://doi.org/10.1007/s40521-022-00309-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40521-022-00309-2