Abstract
Background
Falls are a leading cause of injury in older women. Stepping thresholds quantify balance-reaction capabilities. It is unclear how such evaluations predict falls in comparison to, or as a complement to, other objective measures of gait, standing postural control, strength, and balance confidence.
Aims
The objective of this study was to determine if stepping thresholds are prospectively related to falls in older women.
Methods
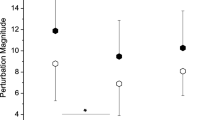
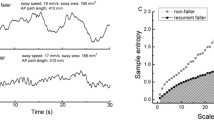
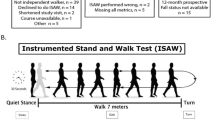
For this prospective cohort study, 125 ambulatory, community-dwelling women, age ≥ 65 years were recruited. Using a treadmill to deliver perturbations to standing participants, we determined anteroposterior single- and multiple-stepping thresholds. Here, thresholds represent the minimum perturbation magnitudes that consistently evoke one step or multiple steps. In addition, gait kinematics, obstacle-crossing kinematics, standing sway measures, unipedal stance time, the functional reach, lower extremity isometric strength, grip strength, balance confidence, and fall history were evaluated. Falls were prospectively recorded for one year.
Results
Seventy-four participants (59%) fell at least once. Posterior single-stepping thresholds were the only outcome that predicted future fall status (OR = 1.50, 95% CI 1.01–2.28; AUC = .62). A multivariate approach added postural sway with eyes closed as a second predictive variable, although predictive abilities were not meaningfully improved.
Discussion
These results align with the previous evidence that reactive balance is a prospective indicator of fall risk. Unlike previous studies, strength scaled to body size did not contribute to fall prediction.
Conclusion
Posterior single-stepping thresholds held a significant relationship with future fall status. This relationship was independent of, and superior to that of, other measures of standing balance, gait, strength, and balance confidence.

Similar content being viewed by others
References
Florence CS, Bergen G, Atherly A et al (2018) Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc 66:693–698. https://doi.org/10.1111/jgs.15304
Prevention CfDCaP-NCfI (2019) Web-based Injury Statistics Query and Reporting System (WISQARS). https://www.cdc.gov/injury/wisqars/index.html. Accessed 3 Jan 2019
Lindle RS, Metter EJ, Lynch NA et al (1997) Age and gender comparisons of muscle strength in 654 women and men aged 20–93 yr. J Appl Physiol 83:1581–1587. https://doi.org/10.1152/jappl.1997.83.5.1581
Sullivan EV, Rose J, Rohlfing T et al (2009) Postural sway reduction in aging men and women: relation to brain structure, cognitive status, and stabilizing factors. Neurobiol Aging 30:793–807. https://doi.org/10.1016/j.neurobiolaging.2007.08.021
Berg WP, Alessio HM, Mills EM et al (1997) Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing 26:261–268
Campbell AJ, Borries MJ, Spears GF et al (1990) Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 19:136–141
Davis JW, Ross PD, Nevitt MC et al (1997) Incidence rates of falls among Japanese men and women living in Hawaii. J Clin Epidem 50:589–594
Maki BE, Holliday PJ, Topper AK (1994) A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol 49:M72–84
Sturnieks DL, Menant J, Delbaere K et al (2013) Force-controlled balance perturbations associated with falls in older people: a prospective cohort study. PLoS ONE 8:e70981. https://doi.org/10.1371/journal.pone.0070981.g001
Hilliard MJ, Martinez KM, Janssen I et al (2008) Lateral balance factors predict future falls in community-living older adults. Arch Phys Med Rehabil 89:1708–1713. https://doi.org/10.1016/j.apmr.2008.01.023
Mille ML, Johnson-Hilliard M, Martinez KM et al (2013) One step, two steps, three steps more … Directional vulnerability to falls in community-dwelling older people. J Gerontol A Biol Sci Med Sci 68:1540–1548. https://doi.org/10.1093/gerona/glt062
Carty CP, Cronin NJ, Nicholson D et al (2015) Reactive stepping behaviour in response to forward loss of balance predicts future falls in community-dwelling older adults. Age Ageing 44:109–115. https://doi.org/10.1093/ageing/afu054
Carty CP, Barrett RS, Cronin NJ et al (2012) Lower limb muscle weakness predicts use of a multiple- versus single-step strategy to recover from forward loss of balance in older adults. J Gerontol A Biol Sci Med Sci 67:1246–1252. https://doi.org/10.1093/gerona/gls149
Ek S, Rizzuto D, Fratiglioni L et al (2019) Risk factors for injurious falls in older adults: the role of sex and length of follow-up. J Am Geriatr Soc 67:246–253
Gale CR, Cooper C, Aihie Sayer A (2016) Prevalence and risk factors for falls in older men and women: the English Longitudinal Study of Ageing. Age Ageing 45:789–794. https://doi.org/10.1093/ageing/afw129
Sturnieks DL, Menant J, Vanrenterghem J et al (2012) Sensorimotor and neuropsychological correlates of force perturbations that induce stepping in older adults. Gait Posture 36:356–360. https://doi.org/10.1016/j.gaitpost.2012.03.007
Crenshaw JR, Kaufman KR (2014) The intra-rater reliability and agreement of compensatory stepping thresholds of healthy subjects. Gait Posture 39:810–815. https://doi.org/10.1016/j.gaitpost.2013.11.006
Crenshaw JR, Bernhardt KA, Atkinson EJ et al (2018) The relationships between compensatory stepping thresholds and measures of gait, standing postural control, strength, and balance confidence in older women. Gait Posture. https://doi.org/10.1016/j.gaitpost.2018.06.117
Kanis JA, Johnell O, Oden A et al (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397. https://doi.org/10.1007/s00198-007-0543-5
Crenshaw JR, Bernhardt KA, Achenbach SJ et al (2017) The circumstances, orientations, and impact locations of falls in community-dwelling older women. Arch Gerontol Geriatr 73:240–247. https://doi.org/10.1016/j.archger.2017.07.011
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Ainsworth BE, Haskell WL, Leon AS et al (1993) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25:71–80. https://doi.org/10.1249/00005768-199301000-00011
Powell LE, Myers AM (1995) The Activities-Specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci 50A:M28–34
Chou L, Kaufman KR, Hahn ME et al (2003) Medio-lateral motion of the center of mass during obstacle crossing distinguishes elderly individuals with imbalance. Gait Posture 18:125–133
Hurvitz EA, Richardson JK, Werner RA et al (2000) Unipedal stance testing as an indicator of fall risk among older outpatients. Arch Phys Med Rehabil 81:587–591
Duncan PW, Studenski S, Chandler J et al (1992) Functional reach: predictive validity in a sample of elderly male veterans. J Gerontol 47:M93–98
Hof AL (1996) Scaling gait data to body size. Gait Posture 4:222–223
Friedman J, Hastie T, Tibshirani R (2010) Regularization paths for generalized linear models via coordinate descent. J Statist Soft 33:1–22
van Buuren S, Groothuis-Oudshoorn K (2011) MICE: Multivariate imputation by chained equation in R. J Stat Soft. https://doi.org/10.18637/jss.v045.i03
O'Loughlin JL, Robitaille Y, Boivin J-F et al (1993) Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 137:342–354
Moreland JD, Richardson JA, Goldsmith CH et al (2004) Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc 52:1121–1129. https://doi.org/10.1111/j.1532-5415.2004.52310.x
Gadelha AB, Neri SGR, Vainshelboim B et al (2019) Dynapenic abdominal obesity and the incidence of falls in older women: a prospective study. Aging Clin Exper Res. https://doi.org/10.1007/s40520-019-01318-z
Todd C, Skelton D (2004) What are the main risk factors for falls among older people and what are the most effective interventions to prevent these falls? World Health Organization Regional Office for Europe
Wijlhuizen GJ, de Jong R, Hopman-Rock M (2007) Older persons afraid of falling reduce physical activity to prevent outdoor falls. Prev Med 44:260–264. https://doi.org/10.1016/j.ypmed.2006.11.003
van Roden EAR, Petersen DA, Pigman J et al (2018) The contribution of counter-rotation movements during fall recovery: a validation study. J Biomech 78:102–108. https://doi.org/10.1016/j.jbiomech.2018.07.025
Runge CF, Shupert CL, Horak FB et al (1999) Ankle and hip postural strategies defined by joint torques. Gait Posture 10:161–170. https://doi.org/10.1016/S0966-6362(99)00032-6
Nonnekes J, Scotti A, Oude Nijhuis LB et al (2013) Are postural responses to backward and forward perturbations processed by different neural circuits? Neuroscience 245:109–120. https://doi.org/10.1016/j.neuroscience.2013.04.036
Mansfield A, Wong JS, Bryce J et al (2015) Does perturbation-based balance training prevent falls? Systematic review and meta-analysis of preliminary randomized controlled trials. Phys Ther 95:700–709
Van Hooren B, Meijer K, McCrum C (2018) Attractive gait training: Applying dynamical systems theory to the improvement of locomotor performance across the lifespan. Front Physiol 9:1934. https://doi.org/10.3389/fphys.2018.01934
Friedman SM, Munoz B, West SK et al (2002) Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc 50:1329–1335. https://doi.org/10.1046/j.1532-5415.2002.50352.x
Langeard A, Desjardins-Crepeau L, Lemay M et al (2019) Cognitive performances better identify fallers than mobility assessment among older adults with fear of falling. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01338-9
Lauretani F, Ticinesi A, Gionti L et al (2019) Short-physical performance battery (SPPB) score is associated with falls in older outpatients. Aging Clin Exper Res 31:1435–1442. https://doi.org/10.1007/s40520-018-1082-y
Henstra MJ, Rhebergen D, Stek ML et al (2019) The association between apathy, decline in physical performance, and falls in older persons. Aging Clin Exper Res 31:1491–1499. https://doi.org/10.1007/s40520-018-1096-5
Asai T, Misu S, Sawa R et al (2015) Multi-chronic musculoskeletal pain is a useful clinical index to predict the risk of falls in older adults with normal motor function. Aging Clin Exper Res 27:711–716. https://doi.org/10.1007/240520-015-0340-5
Acknowledgements
We thank Louise McCready, R.N. for study coordination and Diana Hansen for data collection and processing.
Funding
This work was supported by National Institutes of Health [grant numbers R01AR027065 to SK/SA, T32HD07447 to J. R. Basford, NIH UL1TR000135 to SK]. The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
Jeremy R. Crenshaw, Ph.D.: conceptualization, methodology, formal analysis, investigation, writing—original draft, and visualization. Kathie A. Bernhardt, B.S.: methodology, software, investigation, data curation, writing—review & editing, and project administration. Elizabeth J. Atkinson, M.S.: software, formal analysis, data curation, and writing—review & editing. Sara J. Achenbach, M.S.: software, formal analysis, data curation, and writing—review & editing. Sundeep Khosla, M.D.: conceptualization, resources, writing—review & editing, and funding acquisition. Shreyasee Amin, M.D. M.P.H.: conceptualization, methodology, resources, writing—review & editing, supervision, project administration, and funding acquisition. Kenton R. Kaufman, Ph.D. P.E.: conceptualization, methodology, resources, writing—review & editing, supervision, project administration, and funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
None, this paper is the authors’ own original work, which has not been previously published elsewhere.
Statement of human and animal rights
This study was approved by the Mayo Clinic Institutional Review Board.
Informed consent
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
An 89-year-old participant undergoes assessments of single- and multiple-stepping thresholds. Electronic supplementary material 1 (MP4 23740 kb)
Appendix 1
Appendix 1
See Table 3.
Rights and permissions
About this article
Cite this article
Crenshaw, J.R., Bernhardt, K.A., Atkinson, E.J. et al. Posterior single-stepping thresholds are prospectively related to falls in older women. Aging Clin Exp Res 32, 2507–2515 (2020). https://doi.org/10.1007/s40520-020-01480-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01480-9